Cerebral venous sinus thrombosis is an elusive diagnosis with profound potential neurologic consequences. Although there are numerous reported predisposing conditions, by far the most common is a prothrombotic hypercoagulable state. Recent advances in MRI and computed tomography have improved diagnostic accuracy for this increasingly recognized disorder. Familiarity with imaging techniques and potential pitfalls is essential for accurate diagnosis and management of these patients.
Key points
- •
CVT can be an elusive clinical diagnosis because of the varied and nonspecific presenting symptoms. A high index of suspicion is required for clinicians and radiologists, especially for the detection of isolated cortical vein thrombosis.
- •
A noncontrast head computed tomography is fairly insensitive for the detection of cerebral vein thrombosis (CVT), and a normal study does not exclude the diagnosis. Additional imaging is warranted when CVT is suspected.
- •
MRI/magnetic resonance venography is an excellent, noninvasive technique for diagnosing CVT. Newer sequences, including susceptibility-weighted imaging and postcontrast 3-dimensional gradient echo T1, allow for improved diagnostic sensitivity and specificity compared with traditional protocols.
- •
Most patients recover with medical management. Endovascular thrombectomy should be considered for patients with contraindication to heparin, with high morbidity/mortality risk factors, and those who progress despite conservative therapy.
Introduction
Thrombosis of intracranial veins and the dural venous sinus system has long been a diagnostic dilemma because of its protean, nonspecific clinical manifestations and subtle appearance on traditional imaging modalities. However, this complex condition has become increasingly recognized in recent years, particularly with the advance of MRI.
It is estimated that the annual incidence of CVT is between 2 and 7 cases per million people and that a typical tertiary-care center will see between 5 and 8 cases of CVT per year. These numbers are likely underestimated as sensitivity for detection of this disease has improved significantly in recent years. The disease affects a wide age group from newborn through elderly. Although there is no specific age demographic, it is well established that CVT preferentially affects women (by a ratio of approximately 3 to 1).
The exact cascade of events that result in CVT is not entirely understood, but predisposing conditions may include an underlying hypercoagulable state, mechanical obstruction, venous stasis, or some combination thereof. There are a wide variety of known risk factors, and most patients with CVT will have one or more. Intrinsic and acquired coagulopathies seem to be the most important factor, associated with up to 70% of cases.
Cancer is an important cause of venous thromboembolism and accounts for approximately 20% of all cases of this entity. Venous thrombosis is the second leading cause of death in patients with cancer. Thrombotic events in patients with cancer usually manifest as extremity deep venous thrombosis or pulmonary embolism but can also occur in the cerebral circulation.
The most common cancers associated with venous thrombosis involve the prostate, colon, lung, and brain in men and the breast, lung, and ovary in women. Importantly, idiopathic thromboembolic disease may be a predictor of the presence of occult malignancy; cancers in such patients are associated with an advanced stage and a poor prognosis.
The cause of venous thrombosis in malignancy is complex and incompletely understood. It is now thought that almost all types of tumor cells are capable of activating the clotting pathway, causing thrombosis by their ability to produce and release procoagulant substances and inflammatory cytokines and through their interaction with leucocytes, endothelial, and platelet host cells. In cancer, there seems to be a shift to a prothrombotic state, achieved by disruption of the fine balance between the coagulation and fibrinolytic systems that normally exist. This shift may occur either as a result of an excess of procoagulant proteins (s tissue factor, fibrinogen, and plasminogen activator inhibitor) or as a consequence of deficiency in other molecules (antithrombin III, proteins C and S, and tissue plasminogen activator). In addition, venous thrombosis may also occur as a consequence of chemotherapy, as is well known with l -asparaginase in patients with acute lymphoblastic leukemia and possibly with agents such as cisplatin, etoposide, medroxyprogesterone acetate, and tamoxifen. Also, factors such as surgery and postoperative immobility and placement of venous catheters play an important role in the predisposition to thrombosis.
Unlike deep vein thrombosis seen in the upper or lower extremities, external compression is typically not an issue for the cerebral venous sinus system. However, mechanical obstruction may occur from intracranial masses, such as a meningioma or focal disruption/distortion of the sinus as seen in a temporal bone fracture.
Venous stasis is another potential contributing factor in the development of CVT. Dehydration, hypovolemia, and intracranial hypotension are associated with thrombosis. The veins and dural sinuses distend in this setting as a compensatory reaction to decreased cerebrospinal fluid (CSF). This distention and associated delayed venous transit time may promote thrombus formation.
Alteration or obstruction of normal venous drainage from CVT results in increased venous and capillary blood pressure, which in turn can disrupt the blood-brain barrier. Depending on the severity and duration of this disruption, CVT can cause vasogenic edema, cytotoxic edema (venous infarction), and/or hemorrhage. The acuity of the venous thrombosis also seems to play a significant role in the development of edema and hemorrhage, likely related to the development of venous collateral system. For example, dural sinuses that become occluded over the course of months to years from slow-growing meningiomas rarely induce brain parenchymal injury, whereas those ligated during surgery commonly do.
In addition to localized venous hypertension, dural sinus thrombosis may result in elevated intracranial pressure. The choroid plexus produces CSF at a rate of approximately 500 mL/d, and resorption is thought to occur at the level of the dural venous sinuses through arachnoid granulations and arachnoid villi. Disruption of this homeostasis from thrombosis may result in hydrocephalus and increased intracranial pressure; symptoms and outcomes from CVT vary widely.
Patients will most commonly present complaining of a headache. This headache may be seen in isolation or with additional symptoms of intracranial hypertension, such as vomiting and visual disturbance. The features of the headache are not specific and may mimic other headache syndromes, such as migraine or subarachnoid hemorrhage. Headaches may be gradual in onset or acute, localized, or diffuse.
In addition to headaches, patients may develop focal neurologic deficits from vasogenic or cytotoxic edema. Motor and sensory deficits are the most commonly described, but verbal and visual defects also occur. As with most diseases affecting the brain, symptomatology is determined by the specific site and extent of involvement. Many neurologic deficits resolve with treatment; however, those patients who experience infarction or hemorrhage may never recover. CVT may cause focal or generalized seizures. Profound cases of CVT can cause encephalopathic symptoms, including disturbances of consciousness, cognitive dysfunction, and even coma.
CVT places patients at risk for the later development of dural arteriovenous fistulas. The exact mechanism for which is not entirely understood, but localized venous hypertension may result in enlargement of physiologic arteriovenous shunts or promote neoangiogenesis. The development of these abnormal shunts between dural arteries and venous sinuses can lead to delayed complications from venous hypertension.
Introduction
Thrombosis of intracranial veins and the dural venous sinus system has long been a diagnostic dilemma because of its protean, nonspecific clinical manifestations and subtle appearance on traditional imaging modalities. However, this complex condition has become increasingly recognized in recent years, particularly with the advance of MRI.
It is estimated that the annual incidence of CVT is between 2 and 7 cases per million people and that a typical tertiary-care center will see between 5 and 8 cases of CVT per year. These numbers are likely underestimated as sensitivity for detection of this disease has improved significantly in recent years. The disease affects a wide age group from newborn through elderly. Although there is no specific age demographic, it is well established that CVT preferentially affects women (by a ratio of approximately 3 to 1).
The exact cascade of events that result in CVT is not entirely understood, but predisposing conditions may include an underlying hypercoagulable state, mechanical obstruction, venous stasis, or some combination thereof. There are a wide variety of known risk factors, and most patients with CVT will have one or more. Intrinsic and acquired coagulopathies seem to be the most important factor, associated with up to 70% of cases.
Cancer is an important cause of venous thromboembolism and accounts for approximately 20% of all cases of this entity. Venous thrombosis is the second leading cause of death in patients with cancer. Thrombotic events in patients with cancer usually manifest as extremity deep venous thrombosis or pulmonary embolism but can also occur in the cerebral circulation.
The most common cancers associated with venous thrombosis involve the prostate, colon, lung, and brain in men and the breast, lung, and ovary in women. Importantly, idiopathic thromboembolic disease may be a predictor of the presence of occult malignancy; cancers in such patients are associated with an advanced stage and a poor prognosis.
The cause of venous thrombosis in malignancy is complex and incompletely understood. It is now thought that almost all types of tumor cells are capable of activating the clotting pathway, causing thrombosis by their ability to produce and release procoagulant substances and inflammatory cytokines and through their interaction with leucocytes, endothelial, and platelet host cells. In cancer, there seems to be a shift to a prothrombotic state, achieved by disruption of the fine balance between the coagulation and fibrinolytic systems that normally exist. This shift may occur either as a result of an excess of procoagulant proteins (s tissue factor, fibrinogen, and plasminogen activator inhibitor) or as a consequence of deficiency in other molecules (antithrombin III, proteins C and S, and tissue plasminogen activator). In addition, venous thrombosis may also occur as a consequence of chemotherapy, as is well known with l -asparaginase in patients with acute lymphoblastic leukemia and possibly with agents such as cisplatin, etoposide, medroxyprogesterone acetate, and tamoxifen. Also, factors such as surgery and postoperative immobility and placement of venous catheters play an important role in the predisposition to thrombosis.
Unlike deep vein thrombosis seen in the upper or lower extremities, external compression is typically not an issue for the cerebral venous sinus system. However, mechanical obstruction may occur from intracranial masses, such as a meningioma or focal disruption/distortion of the sinus as seen in a temporal bone fracture.
Venous stasis is another potential contributing factor in the development of CVT. Dehydration, hypovolemia, and intracranial hypotension are associated with thrombosis. The veins and dural sinuses distend in this setting as a compensatory reaction to decreased cerebrospinal fluid (CSF). This distention and associated delayed venous transit time may promote thrombus formation.
Alteration or obstruction of normal venous drainage from CVT results in increased venous and capillary blood pressure, which in turn can disrupt the blood-brain barrier. Depending on the severity and duration of this disruption, CVT can cause vasogenic edema, cytotoxic edema (venous infarction), and/or hemorrhage. The acuity of the venous thrombosis also seems to play a significant role in the development of edema and hemorrhage, likely related to the development of venous collateral system. For example, dural sinuses that become occluded over the course of months to years from slow-growing meningiomas rarely induce brain parenchymal injury, whereas those ligated during surgery commonly do.
In addition to localized venous hypertension, dural sinus thrombosis may result in elevated intracranial pressure. The choroid plexus produces CSF at a rate of approximately 500 mL/d, and resorption is thought to occur at the level of the dural venous sinuses through arachnoid granulations and arachnoid villi. Disruption of this homeostasis from thrombosis may result in hydrocephalus and increased intracranial pressure; symptoms and outcomes from CVT vary widely.
Patients will most commonly present complaining of a headache. This headache may be seen in isolation or with additional symptoms of intracranial hypertension, such as vomiting and visual disturbance. The features of the headache are not specific and may mimic other headache syndromes, such as migraine or subarachnoid hemorrhage. Headaches may be gradual in onset or acute, localized, or diffuse.
In addition to headaches, patients may develop focal neurologic deficits from vasogenic or cytotoxic edema. Motor and sensory deficits are the most commonly described, but verbal and visual defects also occur. As with most diseases affecting the brain, symptomatology is determined by the specific site and extent of involvement. Many neurologic deficits resolve with treatment; however, those patients who experience infarction or hemorrhage may never recover. CVT may cause focal or generalized seizures. Profound cases of CVT can cause encephalopathic symptoms, including disturbances of consciousness, cognitive dysfunction, and even coma.
CVT places patients at risk for the later development of dural arteriovenous fistulas. The exact mechanism for which is not entirely understood, but localized venous hypertension may result in enlargement of physiologic arteriovenous shunts or promote neoangiogenesis. The development of these abnormal shunts between dural arteries and venous sinuses can lead to delayed complications from venous hypertension.
Preimaging planning
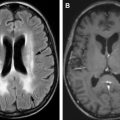
An understanding of venous anatomy is necessary for accurate image interpretation. The supratentorial venous system is traditionally divided into superficial and deep drainage. The deep venous system drains deep gray and white matter structures in a centripetal fashion collecting in the paired internal cerebral veins and basal veins of Rosenthal, which lead to the vein of Galen and straight sinus. The superficial cerebral veins drain the cortex and subcortical white matter in a centrifugal fashion, collecting in the dural venous sinuses (superior sagittal sinus, transverse sinuses). ( Fig. 1 ) Infratentorial veins may drain into the vein of Galen, the petrosal sinuses, or the dural venous sinuses. The superficial and deep venous systems coalesce at the torcula herophili, which is formed at confluence of the superior sagittal sinus, straight sinus, and transverse sinuses. Extracranial drainage is through the internal jugular veins via the sigmoid sinuses (see Fig. 1 ).
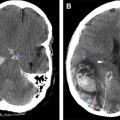
Venous anatomy is highly variable. Superficial cortical veins vary in size and number among patients and are asymmetric, complicating imaging interpretation. Because of the expected variation from one side to another and between patients, absent signal from a thrombosed vessel can easily be overlooked. One of the most commonly confusing anatomic variations is the difference in the size of the transverse sinuses, occurring in almost 50% of people. In 20% of cases, the smaller sinus (typically left sided) is atretic or absent ( Fig. 2 ). This anatomic variation may lead to a false-positive result for inexperienced readers who assume absent enhancement equals thrombosis.
Developmental venous anomalies (DVAs) are the most commonly occurring vascular malformations. These variations occur as a primary dysplasia of normal venous drainage, which results in a radiating collection of small medullary veins that converge on a solitary transcerebral vein ( Fig. 3 ). Although thought to be benign entities composed of mature vascular elements, numerous cases of isolated DVA thrombosis with or without infarction and hemorrhage have been reported. Many investigators think that these structures have abnormal elevated venous pressures and associated vascular stasis.