Fig. 42.1
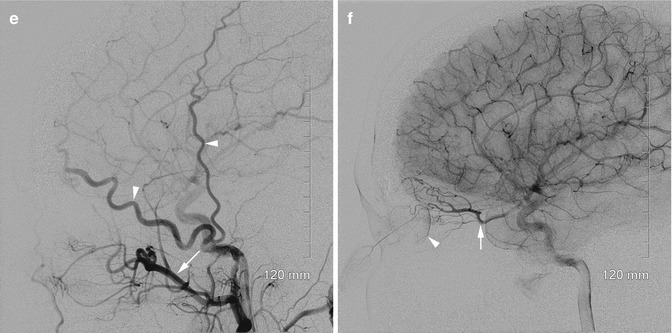
Arteriovenous malformation of the orbit and eyelids. (a) Clinical photo demonstrates anterior displacement of the eyeball (proptosis), with upper eyelid ptosis and conjunctival swelling (chemosis). Arterialized veins can be seen in the eyelid. (b) Axial views of this T2-weighted MRI in a different patient with orbital AVM demonstrates multiple serpiginous flow voids in the preseptal soft tissues of the left orbit with a dilated left superior ophthalmic vein (arrow). (c) Left distal EXTERNAL carotid artery angiogram shows two branches of the superficial temporal artery, one of which is supplying blood to the AVM (arrow). Venous drainage can be seen posteriorly along the superior ophthalmic vein (arrow head) and inferiorly along the facial vein (small arrows). (d) Left INTERNAL carotid artery angiogram shows AVM with blood supply from supraorbital and ethmoidal branches of the ophthalmic artery (arrow). Choroidal blush can be seen identifying the outline of the retina (arrow head). (e) Left EXTERNAL carotid artery angiogram post-embolization shows complete elimination of the malformation with preservation of all the normal arteries including the maxillary branch (arrow) of the external carotid and two major branches of the superficial temporal artery (arrow heads). (f) Left INTERNAL carotid artery angiogram post-embolization. The supply to the AVM from the ophthalmic artery (arrow) has been completely eliminated. Choroidal blush remains (arrow head), indicating retained blood supply to the retina
Nonenhanced CT is helpful in visualizing the small foci of calcification often associated with arteriovenous malformations and foci of hemorrhage if any exist. Contrast-enhanced CT reveals enhancement of the vascular channels, whereas MRI demonstrates these lesions as vascular channels that appear as flow voids (Fig. 42.1c, d). More adequate evaluation is usually obtained by a magnetic resonance angiography or CT angiography, but the gold standard remains traditional angiography [4] (Fig. 42.1e).
Treatment
Angiographic embolization can occlude the nidus and major bleeding vessels in an orbital AVM [4, 5] (Fig. 42.1f). The most serious risk of this treatment is ophthalmic artery or central retinal artery occlusion and is stratified according to specific location of the AVM. The effect of embolization is often temporary, however. Surgical resection, in contrast, can be definitive. Without embolization, surgical resection is possible but difficult due to the risk of massive bleeding. A combination of embolization and surgical excision offers better control and ultimately an optimal outcome. Gamma knife radiotherapy, according to Liscak et al., resulted in obliteration of AVMs in 74 % of cases after the first cycle and 69 % after the second [6].
Carotid-Cavernous Fistula
A carotid-cavernous fistula is an abnormal shunt between the carotid artery and cavernous sinus, or a directly related ophthalmic vein. These fistulae are sometimes categorized as arteriovenous malformations in the ophthalmic literature.
Direct carotid-cavernous sinus fistulae can be caused by trauma or spontaneous rupture of an aneurysm of the intracavernous carotid or an atherosclerotic artery [7]. Indirect carotid-cavernous sinus fistulae are characterized by arterial blood that flows through the meningeal branches of the internal or the external carotid arteries indirectly into the cavernous sinus [7].
Diagnosis
Carotid-cavernous sinus fistulae usually present with epibulbar injection, pulsatile proptosis, and a bruit or thrill. Blepharoptosis and hemorrhagic chemosis can also be seen. The patient can experience limitations of extraocular movements and complain of decrease in vision, headache, and eyelid swelling. The presence of increased intraocular pressure is typically caused by elevation in episcleral venous pressure, limiting outflow of aqueous humor. Anterior segment ischemia, characterized by corneal edema, iris atrophy, and rubeosis iridis, can be seen. Retinal hemorrhages are possible.
CT and MRI can detect a prominence of the superior ophthalmic vein. An arterial angiography helps in making the definitive diagnosis.
Treatment
In most cases, observation allows spontaneous resolution of the fistula. Selective embolization to occlude the fistula is usually done if visual impairment becomes progressive or in case of severe proptosis or if the patient is complaining of intolerable headache or bruit [8].
Venous Malformations
Venous malformations (VM) can be encapsulated or distensible. The former have been incorrectly called “cavernous hemangiomas,” while the latter are sometimes referred to as “varices.”
Encapsulated venous malformations are the most common orbital lesions found in adults. They are benign, slow-growing vascular lesions of the orbit [9].
Diagnosis
Patients with encapsulated venous malformations typically present with axial proptosis described as painless, slowly progressive protrusion of the eye associated with mild eyelid swelling. Axial proptosis (direct forward displacement of the eyeball) is produced most commonly, as these lesions tend to be found in the intraconal space defined by the four rectus muscles. Less commonly, the encapsulated venous malformation is seen extraconally, in which case the eyeball may be displaced vertically or horizontally. With direct observation alone, this can be difficult to distinguish from strabismus, a condition in which the eye is rotated vertically or horizontally. Alternate cover testing reveals the difference; in the strabismic condition, the uncovered eye rapidly rotates back into primary fixation, whereas the eye does not move back from horizontal or vertical translation. When located close to the orbital apex, encapsulated venous malformations can cause compressive optic neuropathy and decreased visual acuity. Diplopia, when present, is explained by distortion or distension of the extraocular muscles rather than by direct intramuscular involvement [1, 10]. Differential diagnosis usually includes schwannoma because of the similarity in size, shape, and location [11].
As with all orbital conditions, imaging studies are critically important. First, an orbital ultrasound, with the advantage of being a noninvasive technique, can detect a uniformly high-echogenic lesion with well-defined borders. A color Doppler US helps in detecting the blood flow and mapping the vasculature. Computed tomography should be performed with contrast. It shows an oval- or round-shaped, sharply demarcated homogenous lesion with slow contrast enhancement. On MRI, the lesion is seen isointense on T1 and hyperintense on T2; few internal septa can be seen, with a progressive accumulation of the contrast on late-phase images [12] (Fig. 42.2a).
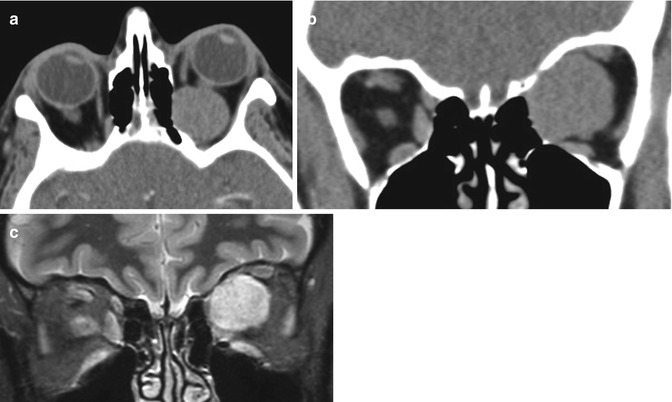
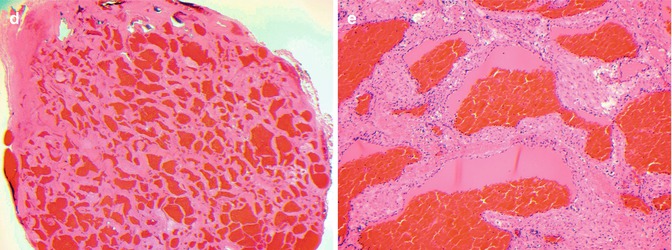
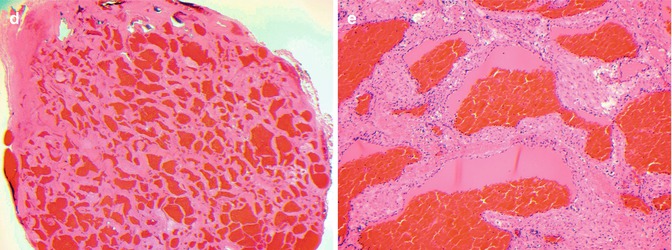
Fig. 42.2
Encapsulated venous malformation of the orbit. (a) Axial view of computed tomograph (CT) of the orbit without contrast demonstrates an ovoid, clearly delimited lesion of approximately 2 cm in the intraconal space. (b) Coronal view of the same CT shows the lesion abutting the medial wall and roof of the orbit in the superomedial quadrant of the orbit. (c) This coronal view of this T1-weighted, gadolinium-enhanced, fat-suppressed MRI demonstrates numerous septations within the lesion but fails to highlight the relationship of the lesion to the thin bones of the orbit. Additional findings include displacement of the extraocular muscles and optic nerve sheath complex. (d) Histopathologic section of the lesion above demonstrates the general architecture of the lesion with numerous thick fibrous septa (hematoxylin and eosin, 20×). (e) Higher magnification view demonstrates large vascular spaces filled with erythrocytes, with flattened endothelial cells (hematoxylin and eosin 100×). D2–40 stain for lymphatic endothelial cells was negative (not shown)
Treatment
The treatment of orbital venous malformations is mostly conservative, but an intervention is needed in case of high orbital pressure or unbearable pain, deep orbital hemorrhage causing drop in vision, and cosmetic deformity [13].
In the cases in which surgical excision is indicated, the approach is dictated by the location of the lesion within the orbit. Most cavernous hemangiomas are found within the intraconal space between the extraocular muscles and the optic nerve. When the lesion is located lateral to the optic nerve, a lateral approach is used, either with or without temporary removal of the orbital rim. Inferior or inferomedial lesions can be removed endoscopically [14]. The medial intraconal space can also be accessed transconjunctivally, sometimes requiring temporary disinsertion of the medical rectus; occasionally the lateral orbital rim is removed to allow retraction of the eyeball during medial tumor removal. Inferiorly located lesions can be approached with a subciliary incision or transconjunctivally, while superiorly located lesions can be removed via an eyelid incision. Superior-posterior lesions may require cranio-orbitotomy for complete removal (Fig. 42.2b).
Distensible Venous Malformations
In contrast to encapsulated venous malformations, distensible venous malformations are meandering and poorly demarcated. They are more likely located outside the muscle cone and also tend to involve the eyelids. These lesions are not encapsulated and do not respect anatomic boundaries. Whereas the encapsulated lesions are almost always seen in isolation, the distensible lesions are more commonly associated with venous malformations of the hemiface including scalp, airway, buccal space, and masseter. These lesions have been described as a “bag of grapes” [1]. The most striking feature of distensible venous malformations, a feature starkly contrasted in encapsulated venous malformations, is a dramatic volumetric response to changes in venous pressure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







