Fig. 29.1
(a) Plain film radiograph reveals multiple phleboliths identified within an extensive infiltrative VM of the forearm with thickening and mass effect on cutaneous and subcutaneous soft tissue. (b) Long-standing radiograph of Klippel-Trénaunay syndrome. 14-year-old girl with typical limb length discrepancy due to increased longitudinal growth in the affected right limb; the CVM also causes thinning of cortical bone at the distal third of peroneal diaphysis (white arrow). (c) Plain film radiograph of an AVM involving the left shoulder. Plain film radiograph shows the involvement of glenohumeral junction with osteolysis of inferior glenoid labrum and of the head of the humerus. Black arrow indicates radiopaque material (Onyx®) due to previous endovascular treatment
A typical finding, present in the 70 % of cases of Klippel-Trénaunay syndrome, is mild limb length discrepancy due to increased longitudinal growth in the affected limb; this aspect can be easily assessed with long-standing radiograph (Fig. 29.1b) [3].
Other radiographic findings can be identified within VM-containing syndromes: plain film findings of Maffucci’s syndrome include the sine qua non finding of multiple enchondroma phlebolith formation; because a high percentage of enchondromas can undergo malignant degeneration to chondrosarcoma, clinical and radiographic vigilance is required. Gorham-Stout syndrome, or disappearing bone disease, is a rare skeletal disorder that is associated with diffuse VMs. The disease is characterized of progressive relentless osteolysis usually within the skull, shoulder, or pelvis that may be preceded by trauma. Intramedullary and subcortical lucent foci coalesce to diminish the diaphyses resulting in tapered ends of the long bone creating a cone-like or “sucked candy” appearance [3].
Vascular malformations may alter bone structure and bone growth. Arteriovenous malformations (AVM) may be sited inside the bones showing some typical images in plain film radiograph pictures of bone. The precise study of these defects, especially the areas of thinning of cortical or even the aspects of cortical “holes,” is useful in order to detect specific bone point where direct puncture may be attempted if an intraosseous direct injection in the malformation (coils, glue, alcohol, etc.) is planned (Fig. 29.1c).
Venography
The phlebographic techniques (ascending or descending venography and direct percutaneous venography [DPV]) are by far less performed than in the past because other noninvasive methods like US, MR, and CT give excellent results [8]. However, in some specific conditions, when noninvasive tests failed to confirm the diagnosis, they may be effective to complete diagnosis or in the preoperative planning in low-flow CVM [9].
Ascending phlebography is mainly performed to study the deep venous system of the lower limbs: anomalies of the deep venous system in fact occur in almost one half of congenital vascular malformations of venous predominance [10]. The correct diagnosis of these anomalies represented by avalvulia, aplasia, hypoplasia, phlebectasia, and venous aneurysms (Fig. 29.2a–e) is important to prevent serious therapeutic consequences [10].
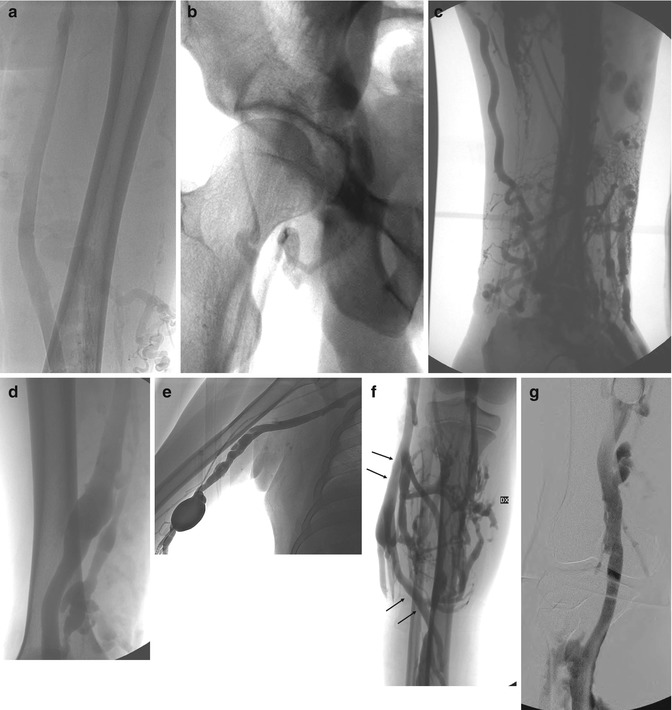

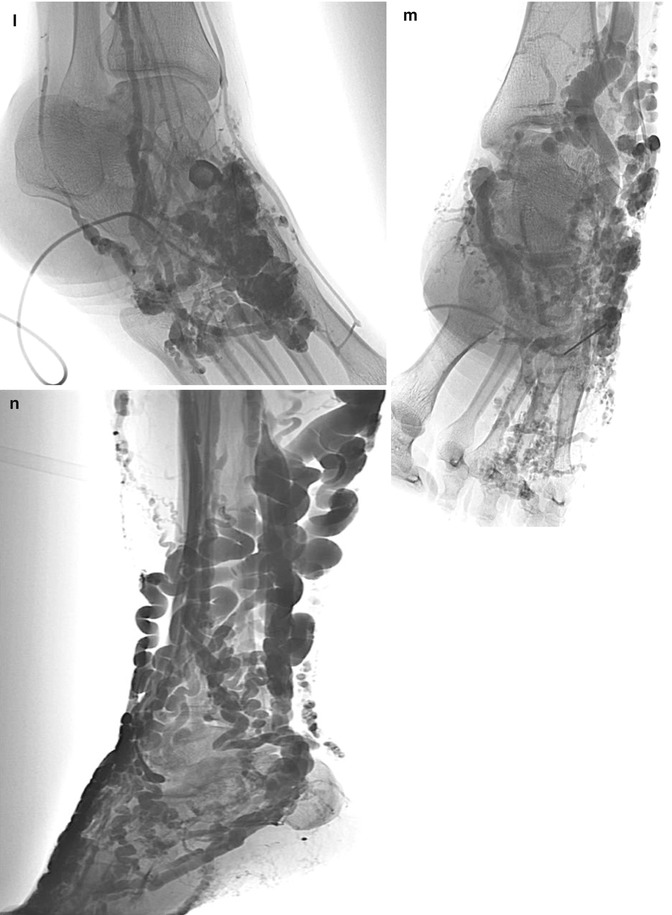
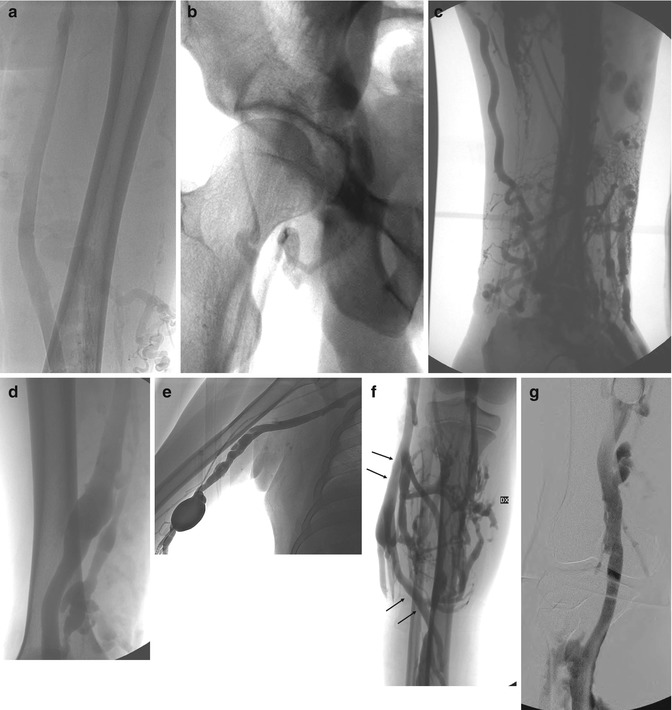

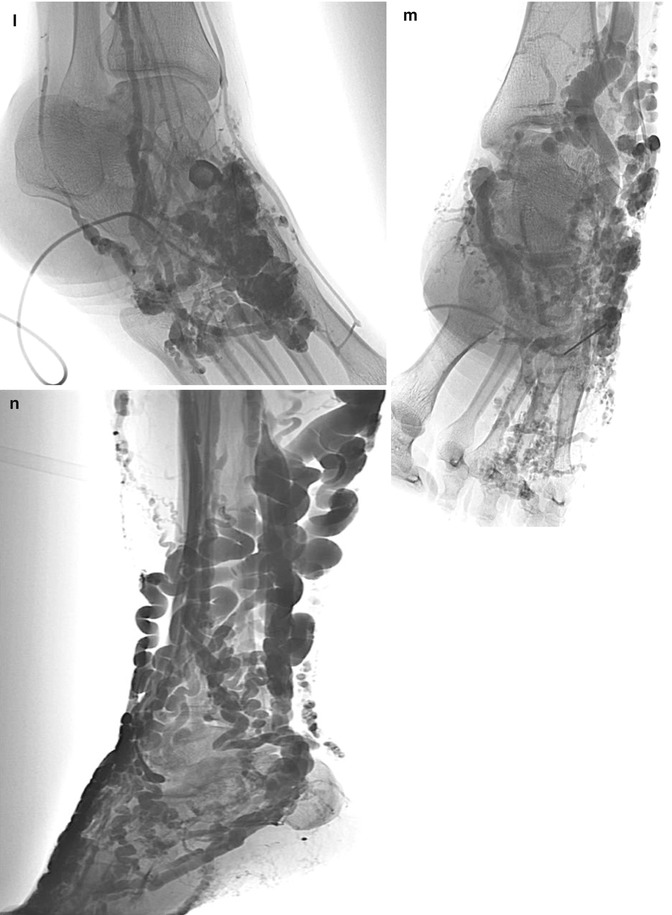
Fig. 29.2
(a–f) Ascending phlebography performed after cannulation of the dorsal vein of the great toe shows different type of deep venous system anomalies such as avalvulia (a), aplasia (b), hypoplasia (c), phlebectasia (d), and venous aneurysms (e); marginal vein (f: arrows), type II according to Weber classification. (g) Descending phlebography shows severe incompetence of venous system (Grade IV) with reflux into the calf veins. (h–j) Direct percutaneous venography: Dubois classification of phlebographic appearance of VMs: cavitary pattern illustration (h), spongy pattern (i) and dysmorphic illustration (j). (k–n): Puig classification of VMs based on venous drainage pattern. (k): Type I VM showing negligible venous drainage into normal venous circulation. (l) Type II VM anatomy revealing normal venous outflow into general venous circulation. (m) Type III anatomy demonstrates drainage from the VM by way of abnormally ectatic or dysplastic veins. (n) Type IV lesions are composed entirely of ectatic or dysplastic veins
This apparently easy technique requires specific knowledge about CVM and skills to be really useful, as wrong results are common. Missing to visualize deep venous system which is hypoplastic (but not aplastic) in some segment is not uncommon because preferential outflow alternative ways may canalize contrast media to superficial vessels. Normal deep venous system may be failed to contrast because of abnormal large perforants to the superficial veins, like in cases of marginal vein (Fig. 29.2f).
Venipuncture is performed via the dorsal vein of the great toe using a size 22-gauge cannula; for venous cannulation, the patient then sits on the edge of the bed or chair with the legs dependent. Before cannulation, the feet are bathed in warm water for 5 min, allowing the veins to become dilated and more prominent. The warm water has the additional effect of softening the skin and may also provide a mild analgesic effect. The dorsal vein of the great toe has the advantage of being easily located, even in an edematous foot, by gently squeezing the dorsum of the toe with both thumbs; a more proximally and laterally located venous cannulation results in inadequate filling and opacification of the deep venous system with contrast more likely to pass into the dorsal venous arch, which then drains into the long and short saphenous veins.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







