Fig. 25.1
Cutaneous steal presenting as pallor in the skin overlying arteriovenous malformations (AVM). (a) Pallor surrounding fine telangiectasias overlying a dermal AVM. (b) Pallor surrounding a combined venous, microcystic lymphatic malformation overlying a subcutaneous AVM
A mature subcutaneous AVM may manifest as a warm, enlarged pulsating mass. The mass effect is due to enlargement of the anomalous vessels as well as an associated soft tissue hypertrophy and fibrosis. Lesions in deeper tissues may not always be clinically recognizable and hemorrhage can be a presenting sign of an occult AVM.
Associated Findings
AVMs often cause soft tissue and bony hypertrophy. The soft tissue hypertrophy results in asymmetry and in time can cause disfigurement. Soft tissue and bony hypertrophy can result in enlargement of the affected limb in length and circumference. This can lead to a secondary scoliosis. When there is an associated venous or lymphatic malformation (Parkes Weber syndrome), typical signs of chronic venous hypertension or lymphedema may be present.
Stewart-Bluefarb Syndrome
Stewart-Bluefarb syndrome (SBS) refers to acroangiodermatitis secondary to an underlying AVM [3]. First described by Bluefarb and Adams and later by Stewart in 1967, the term Stewart-Bluefarb syndrome was conceived by Earhart in 1974 [4].
Acroangiodermatitis is an angioproliferative skin eruption that represents a reactive endothelial hyperplasia [5]. It is possibly driven by an angiogenic response to high perfusion rates and the associated increase in venous and capillary pressures. Clinically, it presents with violaceous brown macules, papules, and nodules that may become confluent to form large plaques. Lesions may eventually ulcerate. Acroangiodermatitis has a predilection for extensor surfaces and in particular the dorsal aspect of the foot and the first three toes (Fig. 25.2a) [6].
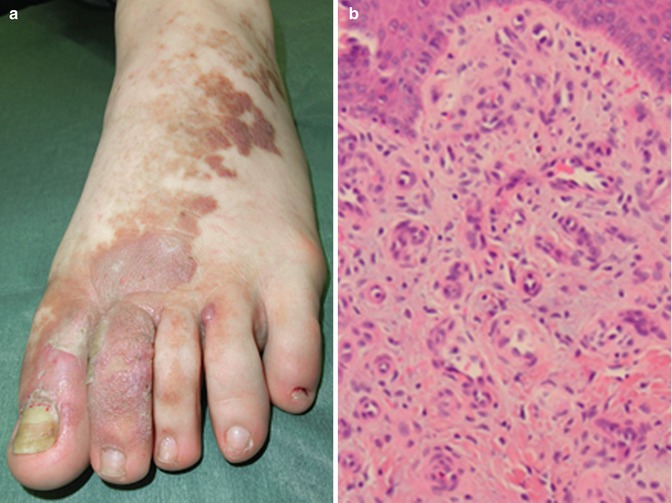
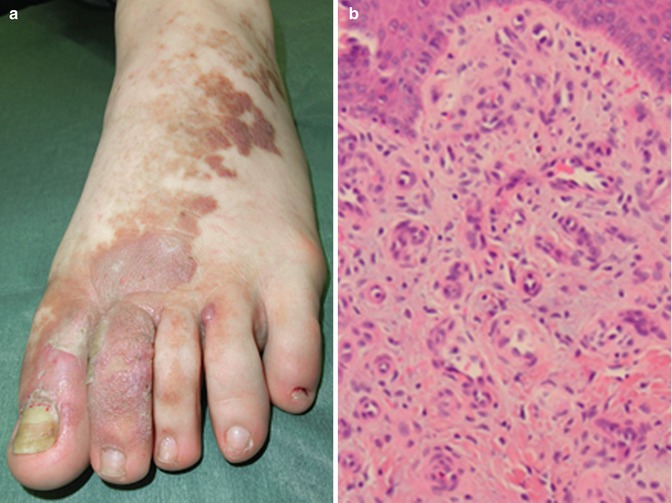
Fig. 25.2
(a) Acroangiodermatitis involving the dorsum of the foot. (b) Histology of acroangiodermatitis comprised of multiple capillaries lined by a single layer of endothelial vessels surrounded by fibroblasts
Histologically, acroangiodermatitis is characterized by profuse thin-walled capillaries lined by a single layer of endothelial cells and a perivascular proliferation of dermal fibroblasts. Secondary changes include extensive extravasation of erythrocytes and hemosiderin deposition in the dermis. There may be an associated inflammatory mononuclear infiltrate (Fig. 25.2b).
Clinically, acroangiodermatitis resembles Kaposi’s sarcoma (KS) and is often referred to as “Pseudo-KS .” Acroangiodermatitis lacks the typical histological features of KS such as the vascular slit pattern, the diverse inflammatory infiltrate, and a positive human herpes virus type 8 (HHV-8), factor VIII-associated antigen, and CD34+ antigen in endothelial cells.
Acroangiodermatitis is not always secondary to an AVM and may have an acquired etiology. The acquired form is referred to as “acroangiodermatitis of Mali” and is seen in the presence of severe venous hypertension at later stages of chronic venous insufficiency (CVI) or secondary to an iatrogenic AV fistula. While SBS is usually unilateral, acroangiodermatitis of Mali may be bilateral. Unlike SBS, histological changes in acroangiodermatitis of Mali are limited to the superficial dermis.
Clinical Pearl
A distinct violaceous pigmentation involving the dorsum of the toes and the feet should trigger a biopsy to diagnose acroangiodermatitis and a search for an underlying AVM.
Venous Malformations (VM)
Truncular Venous Malformations
Truncular VMs present as structural abnormalities such as aplasia, hypoplasia, obstruction, dilation, duplication, aneurysm, and valvular agenesis of the affected vessels. The clinical presentation is quite variable and correlates with the anatomical abnormality. Truncular VMs involving the lower limb veins can cause venous hypertension and present with typical dermatological signs of CVI. These include venous eczema, hyperpigmentation, depigmentation, atrophie blanche, lipodermatosclerosis, and ulceration. In severe cases, subcutaneous calcification and ossification can occur.
CVI secondary to an incompetent embryonic lateral marginal vein of the thigh will present with skin changes involving the lateral distal calf and ankle. Combined malformations such as the Klippel-Trenaunay syndrome (KTS) can present with typical signs of venous hypertension as well as signs of the associated anomalies. While KTS presents with hypertrophy of the affected limb (Fig. 25.3), Servelle-Martorell syndrome presents with bony hypotrophy and limb shortening.









