Fig. 26.1
Diagnostic steps in ultrasound diagnosis of vascular anomalies
1.
Search and recognition of a vascular anomaly, its site, and involved vessels.
2.
Definition of the main morphology, finding out if it is a truncular or an extratruncular defect or even a combination, according to the Hamburg classification.
3.
Definition of the borders, including easily to detect anatomical landmarks, size, and in- and outflow vessels. Calcifications, thrombosis, and infiltration of organs and tissues should be recognized. At the end of the examination, it should be possible to classify the malformation according to the Hamburg classification.
Technique
Study should be performed according to guidelines for the examination of abdomen, neck, and limbs. At the limbs, a bilateral study is recommended to recognize other eventually existing unknown malformations and also to compare the malformed anatomy with the normal limb.
Subcutaneous and soft tissues with a contralateral comparison are necessary to recognize and measure tissue hypertrophy or atrophy
Examination of the limbs should be performed in both upright and lying position, as some venous malformations may not be visible in lying position due to a collapse of low-flow structures. All flow evocative tests should be undertaken in order to clarify as much as possible the hemodynamic map of the limb [7].
Examination should include all axial principal vessels (arteries and veins) and their flow characteristics. After that, the attention should be addressed to the vascular anomalies which are external to the axial vessels (extratruncular anomalies) [1].
Hemodynamic Patterns
Three types of flow pattern are recognizable in CVM:
Slow-flow pattern: Typical of venous malformations. Flow may be spontaneous or only evocated by provocation maneuvers. The physiologic direction of flow should be unidirectional (to the heart). The presence of a reflux component longer than 0.5 may be a sign of incompetence of the underlying vein (Fig. 26.2).
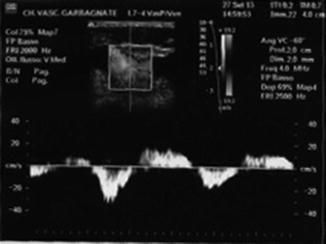
Fig. 26.2
Reflux in truncular malformed veins
This component may be analyzed in order to highlight the reflux time and the reflux volume.
In presence of a reflux, the origin and the pattern should be defined. A continuous venous flow without influence of the respiratory activity to the proximal veins is sign of a possible venous stenosis.
Fast-flow pattern: Typical pulsatile arterial pattern which includes monophasic and triphasic waves. Monophasic waves are typical of low-resistance vessels that perfuse kidneys and brain. This pattern is also typical of AV shunts associated with pulsatile flow in the outflow veins. Distal to the shunt, we observe a slowing and dampening of the arterial velocity profile which may be responsible of peripheral ischemia. Contemporary on the venous side, we can record pulsatile flow proximal to the shunt and blood stasis distally (Fig. 26.3) [6].

Fig. 26.3
Flow characteristics in AV shunt. (a) Arterial component with high diastolic velocity. (b) Venous component with pulsatile flow
Hemodynamic parameters obtained from the study should be recorded in order to allow a quantifiable follow-up of the malformation. Most useful data are flow rate, resistivity index, pulsatility index in AV shunts, and reflux time and reflux volume in venous malformations. Additional important hemodynamic data are segmental pressure measurement in arterial and arteriovenous malformations and dynamic venous measurement in venous malformations (by an invasive method).
Morphology
Truncular anomalies are characterized by the presence of aplasia/obstruction, hypoplasia, or dilatation of the involved vessels (see Chap. 22). Persistence of embryonic structures like sciatic artery, sciatic vein, and embryonal vein is also possible and may be combined with the other truncular defects or with areas of dysplastic vessels in the tissues (extratruncular forms). Course of all vessels should be investigated in order to find out/exclude anomalies of number, position, and morphology.
More complex is the examination of extratruncular malformations. The tissue echogenicity may be very different in relation to the ratio vessels/tissue and to the existing edema [8].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree