Agent
Target
Stage
Phase
NCI number
Glembatumumab vedotin
gpNMB
Metastatic
I
NCT01997333
Panitumumab + chemotherapy
EGFR
Neoadjuvant
II
NCT02593175
Selumetinib
MEK
Neoadjuvant
II
NCT02685657
Veliparib + lapatinib
PARP, EGFR/Her-2
Metastatic
Pilot study
NCT02158507
Afatinib + paclitaxel
EGFR
Neoadjuvant
II
NCT02511847
Everolimus + eribulin
PI3K/mTOR
Metastatic
II
NCT02616848
Everolimus + cisplatin
PI3K/mTOR
Neoadjuvant
II
NCT1931163
Pemetrexed + sorafenib
Multikinase inhibitor
Metastatic
II
NCT02624700
Sacituzumab govitecan
Trop-2
Metastatic
III
NCT02574455
Trametinib + GSK2141795
AKT, MEK
Metastatic
II
NCT01964924
Ipatasertib + paclitaxel
AKT
Metastatic
II
NCT02162719
BKM120, BYL719 + olaparib
PI3 kinase, PARP
Metastatic
I
NCT01623349
Enzalutamide
AR
Adjuvant
Feasibility study
NCT02750358
GTx-024
AR
Metastatic
II
NCT02368691
PARP inhibitors are targeted agents that inhibit the activity of the PARP polymerase family of enzymes. These enzymes are essential in repairing DNA damage, particularly single-strand breaks through the base excision repair pathway [34]. In cells that are deficient in alternate DNA repair pathways, inhibiting the activity of PARP enzymes leads to cell death through synthetic lethality [34]. An example of synthetic lethality is illustrated by the use of PARP inhibitors in BRCA-mutated cancers. BRCA-mutated cells are deficient in the homologous recombination (HR) pathway for repair of DNA double-strand breaks. By inhibiting the activity of the PARP enzymes, the base excision repair pathway is also eliminated as a potential mechanism for DNA repair. Single-strand breaks can then accumulate, due to inefficient base excision repair, and lead to double-strand breaks at replication forks. In this way, cell death can occur through synthetic lethality [35]. This concept has been tested clinically in populations of BRCA-mutated carriers and shown to be active in BRCA-mutated cancers [35]. A phase II trial of the PARP inhibitor, olaparib, in BRCA-mutated metastatic breast cancer patients showed objective response rates ranging from 21 to 44%. Over 50% of these patients had TNBC. Objective response rates ranged from 21 to 44% [35]. Since BRCA-mutated breast cancers and TNBC share clinical and pathologic characteristics, such as sensitivity to DNA-damaging agents, high pathologic grade, and high rate of p53 mutations, it is proposed that TNBC, which is most like BRCA-mutated breast cancer, is also deficient in the HR pathway [34]. This characteristic would render TNBC vulnerable to PARP inhibition in the same way as BRCA-mutated breast cancer. The use of PARP inhibitors in TNBC is an area of active research. A phase II trial of the intravenous PARP inhibitor, iniparib (BSI-201), in combination with gemcitabine and carboplatin was performed in a population of 120 women with metastatic, pretreated TNBC [36]. Clinical benefit rates were 62% in patients who had received BSI-208 versus 21% with chemotherapy alone. Progression-free and overall survival were also improved with the addition of BSI-201 [36]. A phase III follow-up study compared iniparib in combination with gemcitabine and carboplatin to gemcitabine and carboplatin alone in 519 women with metastatic, pretreated TNBC. The primary endpoints of overall survival and progression-free survival were not met. Subgroup analysis showed that there was a survival benefit in the group of women who had received two or more prior lines of treatment [37]. In vitro data has shown, however, that iniparib demonstrates little or no ability to inhibit formation of PARP polymers or induce apoptosis in cell lines which are deficit in homologous repair pathway, such as BRCA-mutated cells [38, 39]. Further studies of agents with true PARP inhibition have shown promising results. A neoadjuvant study of the PARP inhibitor, veliparib, in combination with paclitaxel and carboplatin showed pCR rates that improved from 26 to 51% with the addition of veliparib in TNBC. Potential biomarker candidates to predict pCR were also evaluated [40, 41]. This combination will be evaluated in a phase III trial.
The PI3K/AKT/mTOR pathway is frequently activated in breast cancer and is another area of active research. This pathway leads to cell survival through activation of a series of proteins, including AKT kinase and mTOR (mammalian target of rapamycin inhibitors) [42]. The pathway is activated by binding of a ligand to various tyrosine kinase receptors, including HER proteins, EGFR, and IGF-1 (insulin growth factor) receptors [42]. This rich pathway presents a number of options for drug targets. A neoadjuvant study of an AKT inhibitor, MK-2206, in combination with standard chemotherapy showed a pCR rate of 40% [43]. The PI3K/AKT/mTOR pathway provides stability of the homologous recombination repair pathway, which is deficient among BRCA-mutated cells. Inhibition of AKT has been shown to render TNBC more sensitive to PARP inhibitors by inducing deficiencies in the HR pathway [42]. In an in vitro study of TNBC, the AKT inhibitor, buparlisib, was shown to sensitize TNBC cells to the PARP inhibitor, olaparib [44]. The tyrosine kinase inhibitor, neratinib , which inhibits binding of the ligand for ErbB and Her family of receptors, was evaluated in the neoadjuvant setting in all subtypes of breast cancer. While neratinib was found to be most efficacious in ER-, Her-2 + breast cancers, there was a subset of TNBC which showed pCR rates of up to 66% with neratinib in combination with anthracycline and taxane. Molecular signatures of these responders show that these tumors showed phosphorylation of EGFR or Her-2/neu [45].
Antibody-drug conjugates are being tested in the treatment of TNBC. Sacituzumab govitecan is a humanized anti-Trop-2 antibody linked to a high concentration of SN-38, which is the active metabolite of irinotecan. Trophoblast cell-surface antigen, Trop-2, is a target that is expressed in multiple solid tumors. The Trop-2 gene encodes a transmembrane calcium signal transducer, which is linked to cell migration. The gene is also referred to as tumor-associated calcium signal transducer 2 (TACSTD2) [46]. Among breast cancer patients, increased expression of Trop-2 is linked to shorter survival [47]. Expression of TACSTD2 is active among TNBC cell lines [48]. A phase II trial of sacituzumab govitecan conducted in 58 TNBC patients, with a median of 4 prior therapies, demonstrated an overall response rate (CR + PR) of 31% and clinical benefit rate (CR+PR+SD) of 49%. Given that this study was conducted among a heavily pretreated population, these outcomes are very promising in patients with refractory TNBC [49]. Glembatumumab vedotin is an antibody-drug conjugate of the cytotoxin, monomethyl auristatin E, that targets glycoprotein NMB (gpNMB). gpNMB is overexpressed in a multiple tumor types and is a poor prognostic factor among breast cancer patients. A phase I trial glembatumumab vedotin among metastatic breast cancer showed response rates of up to 40% among TNBC patients with gpNMB overexpression [50].
Targeted Therapies by TNBC Subtype
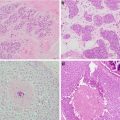
Different molecular subtypes of TNBC have been identified through gene expression profiling. Six molecular subtypes have been identified: two types of basal-like (BL1 and BL2), mesenchymal (M), mesenchymal stemlike (MSL), luminal androgen receptor (LAR), and an immunomodulatory subtype (IM) [51]. These subtypes have been further refined in four subtypes (BL1, BL2, M, and LAR) [52]. The responses to neoadjuvant chemotherapy have been correlated by different subtypes and suggest varying responses to treatment among the different subtypes.
The luminal androgen receptor (LAR) type is characterized by hormonally regulated pathways, expression of androgen receptors and display positivity for phosphatidylinositol-4,5-bisphosphae 3-kinase subunit PIK3CA-α activating mutations with less responsiveness to chemotherapy. This type of TNBC has the lowest responsiveness to chemotherapy, which is estimated to be about 10% pathologic complete response rates in the neoadjuvant setting [53]. Preclinical models have suggested the utility of androgen receptor antagonist in the androgen receptor (AR)-positive TNBC. One study combined PI3K kinase inhibitors with an AR antagonist and showed inhibitory effects in laboratory models [51]. In a study of 50 metastatic TNBC patients with IHC >10% for AR, a 19% 6-month clinical benefit rate was achieved with single-agent bicalutamide, an AR antagonist, [54]. Enzalutamide is an androgen receptor inhibitor that is approved for use in metastatic prostate cancer patients. Because of the mechanism of action, it is also a potential treatment for the AR subtype. A phase II study of enzalutamide was conducted among TNBC patients with advanced disease. AR expression was measured by immunohistochemistry , and an androgen-driven gene signature was constructed by genomic profiling of tumors. Results were measured by those patients with tumors that displayed the androgen-driven signature (AR+) and those that did not (AR−). Of 118 patients enrolled, 47% of patients were AR+. Patients in this group had better outcomes, with a clinical benefit rate (CBR) of 39% and 36% at 16 and 24 weeks of follow-up, respectively. Among AR− patients, CBR was 11% and 7%, respectively. Among the AR+ group, progression-free survival was 16 weeks, compared to 8 weeks among the AR− group [55]. Median PFS extended to 32 weeks among patients who received enzalutamide in the first- or second-line setting.
The mesenchymal type of TNBC tends to be enriched in cell motility and interactions of the extracellular matrix receptors. The IM subtype is represented by enrichment in genes related to immune cell processes and may be a viable target for immunotherapies. The basal-like type shows enrichment in cell cycle pathways, increased expression of DNA damage response genes, and high Ki-67 expression [32].
Immunotherapy in TNBC
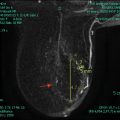
Immunotherapy has changed the treatment landscape for several solid tumors, including melanoma and lung cancer. Approved drugs, such as pembrolizumab, act by disrupting binding of programmed death ligand 1 (PD-L1) expressed on tumor cells to PD-1 receptors on T-cells. Binding of PD-L1 to PD-1 results in T-cell inhibition. Blocking this interaction results in T-cell activation. There is evidence to suggest that immunotherapy may be a viable option in the treatment of TNBC patients and several clinical trials are ongoing (Table 11.2). The presence of tumor-infiltrating lymphocytes (TILs ) is associated with better prognosis in TNBC. Higher numbers of TILS in patients with TNBC showed a strong correlation with prognosis in the GeparSixto neoadjuvant trial of TNBC patients. Higher levels of TILs in the tumor specimen correlated with greater pathologic complete response rates [29]. Mittendorf and colleagues reported overexpression of programmed death ligand 1 (PD-L1) in 20% of patients with TNBC, which correlated with higher numbers of TILs [56]. Overexpression of PD-L1 suggests that antibodies to PD-L1 may be efficacious in TNBC. In a phase I clinical trial with pembrolizumab, a humanized monoclonal antibody that blocks interaction of PD-L1 and PD-L2 with PD-1 receptors, overall response rate among metastatic TNBC patients was 18.5% with some durable responses. All patients on trial had tumors which stained positive for PD-L1 expression [57]. A phase I study of atezolizumab , a humanized monoclonal antibody which inhibits PD-L1 binding to PD-1 and B7, in combination with nab-paclitaxel demonstrated that the combination was tolerable with activity among metastatic TNBC patients [58].
Table 11.2
Current clinical trial of immunotherapy in TNBC
Agents | Target | Stage | Phase | NCI number |
|---|---|---|---|---|
Pembrolizumab + chemotherapy | PD-1 | Neoadjuvant | Ib | NCT02622074 |
Pembrolizumab + eribulin | PD-1 | Metastatic | Ib/II | NCT02513472 |
Pembrolizumab + cyclophosphamide | PD-1 | Metastatic | II | NCT02768701 |
Pembrolizumab + niraparib
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|