(1)
Department of Radiation Oncology, Wake Forest Baptist Health, Medical Center Boulevard, Winston-Salem, NC 27157, USA
Keywords
Breast cancerRadiotherapyRegional nodal irradiationPostmastectomy radiotherapyInternal mammary nodal irradiationNeoadjuvant chemotherapyIntroduction
The role of radiation therapy in the management of breast cancer has evolved significantly over the past several decades. In this modern era of improving surgical techniques and more effective chemotherapeutic, targeted biological agents and hormonal therapies, its use in patients with early stage as well as locally advanced breast cancer continues to be refined. Enhanced screening efforts have reduced the relative incidence of late-stage breast cancer with an associated increase in early-stage disease [1]. These trends highlight a need for clear guidelines in the management of early-stage breast cancer, which, given the heterogeneity of clinicopathologic risk factors, are sometimes difficult to elucidate. In the late twentieth century, breast-conserving surgery (BCS ) followed by radiotherapy to the whole breast became an established standard of care in early-stage breast cancer with similar ipsilateral breast control rates relative to mastectomy alone [2, 3]. The addition of radiotherapy to breast-conserving surgery significantly reduced local recurrence rates at 5 years which translates into a 15-year breast cancer-specific mortality rate, irrespective of nodal status [4]. In locally advanced disease, radiation therapy to the chest wall and regional lymph node stations (supraclavicular, infraclavicular, axillary, and internal mammary) in addition to chemotherapy following mastectomy reduced locoregional recurrence (LRR ) and improved disease-free and overall survival for patients with T3–T4 primary tumors or involved axillary lymph nodes [5–7]. High-risk patients with large tumors, high-grade histology, and increasing number of axillary lymph nodes involved at the time of mastectomy with axillary lymph node dissection (ALND ) reaped the greatest benefit from adjuvant postmastectomy radiotherapy (PMRT ). It has been generally accepted that patients with four or more positive lymph nodes are at highest risk for LRR and thus would benefit most from PMRT to minimize that risk. These studies were limited by variability in axillary lymph node evaluation and less efficacious chemotherapy than that available in the present day. In this chapter, we will further discuss the radiotherapeutic management of the axilla and regional lymph nodes in the era of increasing surgical efficacy and sensitivity (via sentinel lymph node biopsy) and significantly improved adjuvant and neoadjuvant systemic treatment options.
Regional Nodal Irradiation for Patients with One to Three Lymph Nodes Involved
Since the aforementioned trials that initially defined the role of PMRT in node-positive breast cancer, there remains controversy regarding the optimal indications for regional nodal irradiation. The uncertainty lies mostly in the setting of less than four axillary lymph nodes involved. Previous trials designed to answer this question have closed without adequate accrual; current randomized controlled trial evidence remains forthcoming. Retrospective, single-institution analyses suggest that regional nodal irradiation for patients with one to three nodes involved does indeed reduce locoregional recurrence and improve disease-free survival, but despite a trend toward improvement in overall survival, a statistically significant survival benefit has not been demonstrated [8–10]. Furthermore, population-based analysis of T2N1 patients with one, two, and three lymph nodes positive at the time of mastectomy who did not receive radiation therapy revealed statistically significant differences in overall and cause-specific survival directly related to the number of LN involved [11]. Based on these results, the risk associated with involved axillary lymph nodes may be better considered as a continuous spectrum rather than on an ordinal scale. Upon subgroup analysis of patients with one to three positive lymph nodes after mastectomy with ALND , regional nodal radiotherapy resulted in a significant relative risk reduction of 87% (ARR 20%) for LRR and 17% (ARR 9%) for overall survival [12]. Meta-analysis of over 8000 patients undergoing mastectomy with axillary surgery randomized to chest wall/regional nodal irradiation vs. no radiotherapy assisted in further clarifying the role for regional nodal radiotherapy in patients with one to three positive lymph nodes after ALND [13]. This patient population experienced reductions in 10-year locoregional (20.3% vs. 3.8%, 2p < 0.00001) and any recurrence rates (45.7% vs. 34.2%, 2p = 0.00006), as well as 20-year breast cancer -specific mortality (50.2% vs. 42.3%, 2p = 0.01). These risk reductions were similar to those experienced by the patients with four or more lymph nodes involved – the benefit of RT was not proportional to the number of lymph nodes involved. The benefits also remained irrespective of the use of systemic therapy, though approximately 90% of patients received at least one form of chemotherapy or hormonal therapy. These data regarding the benefit of postmastectomy RNI are, however, limited by the age of the comprising trials and do not evaluate the potential toxicities of additional radiotherapy to the regional nodes, including increased risk of pulmonary, cardiac, skin/soft tissue, and lymphatics.
A recent randomized trial (EORTC 22922/10925) compared the addition of regional nodal (internal mammary and medial supraclavicular fossa) irradiation to either whole breast or chest wall irradiation versus no RNI in patients with externally located tumors and axillary nodal involvement or medially located tumors regardless of nodal involvement [14]. The majority (76%) of patients underwent BCS ; the others received mastectomy (24%). Both groups underwent ALND ; SLNB was allowed in the later years of the trial to be followed by completion ALND if pathologically node positive. The addition of IMN and supraclavicular RNI to either whole breast or chest wall radiotherapy resulted in reduced disease-free (HR 0.89, CI 0.80–1.00, p = 0.04) and breast cancer-specific mortality (HR 0.82, CI 0.70–0.97, p = 0.02). Overall survival at 10 years was 82.3% in the RNI group and 80.7% in the control group with a trend toward statistical significance (p = 0.05). Analysis of 3- and 10-year toxicity rates revealed elevated risks of pulmonary fibrosis with the addition of RNI (4.4% vs. 1.7%) but no difference in cardiac fibrosis or heart disease (p = 0.06 and p = 0.25, respectively) or skin toxicity [15].
Recent consensus guidelines published by a joint American Society of Clinical Oncology, American Society for Radiation Oncology, and Society of Surgical Oncology panel regarding the use of PMRT in this setting “unanimously agreed that the available evidence shows that PMRT reduces the risks of locoregional failure (LRF ), any recurrence, and breast cancer mortality for patients with T1-2 breast cancer and one to three positive lymph nodes [16].” This panel did, however, caution that patients may exist with such an inherently low risk of LRF that the potential toxicity may outweigh the benefits of PMRT . There is no validated predictive model to aid in identification of patients within this particular subgroup. As such, careful consideration of clinical (advanced age, short life expectancy, comorbidities, or coincident conditions that may increase radiation toxicity) and pathologic factors (T1 tumor size, absence of LVSI, single LN positive, small size of nodal metastases, or good response to NAC) for each individual patient is necessary to evaluate each patient’s risk of recurrence which may then be compared to their risk of toxicity from PMRT .
Regional Nodal Irradiation After Breast-Conserving Surgery
The results of an international randomized controlled trial (NCIC-CTG MA.20) comparing the addition of RNI to whole breast irradiation (WBI) after breast-conserving surgery in node-positive or high-risk node-negative (primary tumor size ≥5 cm or size ≥2 cm with <10 axillary nodes dissected and either grade 3 histology, ER negativity, or the presence of LVSI) patients allow for the comparison of clinical outcomes as well as toxicity rates for WBI with or without RNI in early-stage breast cancer patients [17]. All patients underwent BCS with either axillary lymph node dissection or sentinel lymph node biopsy, 91% received adjuvant chemotherapy based on institutional practice, and 76% received hormonal therapy. Radiation to the whole breast and internal mammary nodes (IMN) was delivered to 50 Gy in 25 fractions using opposed tangents using either wide tangents to include the IMN or standard tangents with a matched IMN field. High axillary, supraclavicular and infraclavicular nodal regions were covered with an anteroposterior beam alignment; posteroanterior field was recommended but not required. A 10–16 Gy boost in 2 Gy fractions to the lumpectomy cavity was allowed per institutional policy. At 10 years, locoregional disease-free survival was significantly higher in the RNI group compared to the control (95.2% vs. 92.2%, p = 0.009). Overall 10-year disease-free survival was also improved in the RNI group (82% vs. 77%, p = 0.01; HR 0.76, CI 0.61–0.94, p = 0.01). These differences were comprised mostly by a reduction in regional recurrence rates; the regions at highest risk were the axillary and supraclavicular areas. This translated into an improvement in distant disease-free survival (HR 0.76, CI 0.60–0.97, p = 0.03) but not in overall survival (HR 0.91, CI 0.72–1.13) at 10 years.
Upon comparison of adverse outcomes following WBI alone versus WBI + RNI, significant increases in acute toxicities such as Grade 2–3 radiation dermatitis (40.1% vs. 49.5%, p < 0.001) and Grade 2 pneumonitis (0.2% vs 1.2%, p = 0.01) were observed. Significantly more frequent delayed toxicities included moderate to severe lymphedema (4.5% vs. 8.4%, p = 0.001) and late skin and subcutaneous tissue changes such as telangiectasia, atrophy, or fibrosis (skin, 4.3% vs. 6.9%, p = 0.02; subcutaneous tissue 2.0% vs. 4.1%, p = 0.01). There were no differences in the rates of fatigue, pain, delayed cardiotoxicity, neuropathy, late pneumonitis, or second cancers between the two groups. Grade 4 toxicity was rare and occurred in only 3 of the 893 patients in the WBI + RNI group. These results suggest that for carefully selected patients with node positive or high-risk node negative disease, the addition of regional nodal irradiation to whole breast irradiation improves locoregional and disease-free survival with a modestly increased risk of few acute and delayed toxicities.
Regional Nodal Irradiation by Extent of Axillary Surgery
The twenty-first century has witnessed a growing body of evidence in support of a novel approach to limited axillary surgery in the form of sentinel lymph node biopsy for the clinically negative axilla. Multiple randomized trials have demonstrated equivalent clinical outcomes when ALND is foregone after a negative SLNB [18, 19]. In the NSABP B-32 control group, which underwent SLNB followed by completion ALND , accuracy was high (97%), and false-negative rates were relatively low (approximately 10%) [20]. Additionally, SLNB alone is significantly better tolerated in comparison to ALND with respect to ipsilateral arm function, lymphedema, and ipsilateral arm paresthesias [21, 22]. These findings suggest that modern breast surgeons may avoid relatively high-risk axillary procedures without significantly sacrificing staging and therapeutic efficacy. However, in this nascent era of limited axillary dissections, the indications for postoperative regional nodal irradiation must simultaneously adapt.
The American College of Surgeons Oncology Group (ACOSOG) Z0011 trial aimed to identify the optimal axillary therapy with regard to overall and disease-free survival for early-stage, clinically node-negative (cT1–2N0) patients found with positive sentinel lymph nodes [23]. All patients underwent lumpectomy followed by adjuvant whole breast radiotherapy; no third-field axillary directed radiation was permitted. Despite the difference in median number of nodes obtained by SNLB and ALND (2, IQR 1–4 and 17, IQR 13–22, respectively), the number of positive nodes was equal in both groups (1, IQR 1–2). The majority of both groups received adjuvant systemic therapy: 97% in the SLNB arm and 96% in the ALND arm. Long-term follow-up has revealed 10-year locoregional recurrence rates of 6.2% in the ALND arm vs. 5.3% in the SLNB arm (p = 0.36). Specific ipsilateral axillary regional recurrence rates at 10 years in the ALND and SLNB groups were low: 0.5% vs. 1.5%, respectively [24]. It should be noted that at the time this trial was ongoing , many radiation oncologists would consider RNI as the standard of care for patients with positive lymph nodes, especially in the setting of incomplete axillary evaluation such as SLNB. The fact that no further axillary directed therapy was permitted was controversial, prompting concerns regarding deviations from protocol by the participating radiation oncologists. Of the radiotherapy records obtained by Jagsi and colleagues, high tangential fields (covering the low axilla) were used for at least one-half of the patients in both groups and 18.9% received RNI using at least three fields [25]. Further review of patients with radiation field deviations revealed that no RT resulted in statistically significant increases in LRR but that the addition of high tangents or supraclavicular fields to the standard breast tangents did not significantly affect this risk [24].
A modern European trial comparing axillary lymph node dissection versus axillary nodal radiotherapy in patients with positive sentinel lymph nodes was also recently published [26]. Women with primary tumors <3 cm who were clinically node negative were randomized prior to SLNB to either ALND or axillary RT in the setting of SLN-positive disease. Patients randomized to the RT arm received 50 Gy in 25 fractions to all three axillary levels as well as the medial supraclavicular region. Adjuvant nodal RT was allowed in the setting of >4 lymph nodes positive in the ALND arm. Representative of a common breast cancer patient today, the majority (82%) underwent BCS , and 90% received systemic treatment (hormonal and/or chemotherapeutic). Five-year axillary recurrence rates were low in both arms: 0.43% (CI 0.00–0.92) after ALND and 1.19% (CI 0.31–2.08) after axillary RT. The SLN-negative group experienced a similar 5-year axillary recurrence rate of 0.72% (CI 0.39–1.04). There was no difference in overall or disease-free survival between the groups, but rates of clinically significant lymphedema were significantly higher after ALND than after RT at 1, 3, and 5 years. This trial puts forth compelling evidence that, in the setting of sentinel lymph node-positive disease, axillary radiotherapy may be comparable to axillary dissection with regard to outcome. As expected, RNI was better tolerated with regard to ipsilateral arm lymphedema. Nonetheless , due to the low rates of axillary recurrence (consistent with the aforementioned ACOSOG study), this study was underpowered to detect noninferiority of axillary RT. These findings do, however, stand testament to the improving efficacy of systemic therapy in reducing regional recurrence compared to historical trials in which no systemic therapy was given and more aggressive surgical interventions were performed [27].
There is growing evidence in support of axillary radiotherapy after sentinel lymph node biopsy in lieu of axillary lymph node dissection in patients undergoing mastectomy, though this practice remains controversial. This is in part related to modern trials as described above which included proportionally more patients receiving breast-conserving surgery than mastectomy. Based on the available data, if the patient and the multidisciplinary team decide to omit axillary lymph node dissection after SLNB alone, patients determined to be at high risk of locoregional recurrence based on primary tumor and SLNB data alone may warrant adjuvant PMRT irrespective of the prognostic and therapeutic effect of ALND . This is reflected in recent guidelines which recommend PMRT after mastectomy and SLNB “only if there is already sufficient information to justify its use without needing to know that additional axillary lymph nodes are involved [16].”
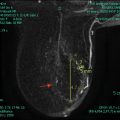
Internal Mammary Nodal Irradiation
The internal mammary nodes (IMN) have been a suspected harbor for regional spread in patients with central-medial tumors [28, 29]. In multiple previous trials, IMN irradiation (IMNI) has been considered a standard component of complete regional nodal irradiation, despite recent controversy over its utility [5, 6, 14, 17, 30]. Further evidence regarding radiation-induced cardiotoxicity has emerged as impetus to further evaluate the risks and benefits of IMNI [31, 32].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree