Total Breast Reconstruction Using Autologous Tissue: TRAM, DIEP, and SIEA Flaps: Introduction
The role of autologous tissue for total breast reconstruction after mastectomy has had a significant impact in cancer management. Breast reconstruction using autologous tissue or prosthetic devices will provide emotional, psychological, and physical benefits in the majority of women. An advantage of autologous reconstruction is that it will last forever, improve over time, and remain soft and supple. Aesthetic and functional outcomes are generally excellent, and patient satisfaction is high.
When considering autologous reconstruction, one of the decisions is to select the appropriate donor site. Although there are several potential donor sites available, the anterior abdominal wall is most commonly used. This is because the adipocutaneous component of the abdomen is ideal for creating and shaping a new breast. It was Carl Hartrampf’s initial description of the pedicle transverse rectus abdominis musculocutaneous (TRAM) flap in 1982 that changed the nature of autologous breast reconstruction and provided a foundation for many of the techniques currently available.1 Since then, the methods by which the skin, fat, and muscle of the anterior abdominal wall are transplanted have evolved such that donor site morbidities have declined without compromising the aesthetic outcomes of the breast. As microvascular techniques developed, the free TRAM was introduced and allowed for the transplantation of greater quantities of skin and fat with less sacrifice of the rectus abdominis muscle.2 An advantage of the free TRAM was its improved vascularity based on the perfusion characteristics of the deep inferior epigastric artery and vein. Further refinements in microvascular surgery resulted in the concept of perforator flaps for breast reconstruction.3 With these flaps, the adipocutaneous component of a flap was transplanted without sacrifice of the donor site musculature. The principle abdominal perforator flaps include the deep inferior epigastric artery flap (DIEP) and the superficial inferior epigastric artery flap (SIEA).2,4 Thus the abdominal wall is the source of 4 flaps that include the pedicle TRAM, free TRAM, DIEP, and SIEA.
This chapter will focus on the various abdominal flaps that are currently used for total breast reconstruction after mastectomy. Emphasis will be placed on patient selection, flap selection, and operative techniques. The perspective will be based on the authors’ personal experience with more than 900 breast reconstructions using the abdomen as the donor site.
It is becoming increasingly appreciated that proper patient selection and good outcomes are intimately related.5 Although many women interested in breast reconstruction may be candidates for autologous reconstruction, not all will be. Candidacy may be precluded for reasons such as medical comorbidities, extremes of body habitus, previous abdominal surgery, lack of interest, or a desire for a quick and simple procedure. That said, approximately 70% of my practice consists of women who have breast reconstruction using autologous tissues. This is in contrast to national trends in which approximately 75% of women have breast reconstruction using prosthetic devices.6 This demographic difference can be partially explained based on the phenomenon of “surgeon selection” that is becoming more prevalent as reconstructive surgeons super specialize in a particular operation. Some surgeons are recognized for their expertise using autologous flaps and microsurgical techniques, whereas others are recognized for their expertise using prosthetic devices. Both methods have the potential for excellent outcomes.
When evaluating a patient for autologous breast reconstruction, several factors should be considered that are related to specific characteristics of the patient and breast. These include breast volume and contour, body habitus, donor site considerations, medical comorbidities, tumor characteristics, patient preference, and the potential for adjuvant therapies. The abdomen has been the donor site of choice for most women for a variety of reasons but is primarily related to tissue availability and quantity as well as breast aesthetics. In general, the most important physical finding is a sufficient quantity of skin and fat in order to reconstruct the desired breast volume. Although a woman may be slender with a paucity of abdominal fat, she may still be a candidate for an abdominal flap if the breast volume requirement is low. In women who are overweight or obese and have a large volume requirement, an abdominal flap can still be performed; however, the flap should be tailored to sustain its perfusion requirement and to minimize the incidence of fat necrosis.7,8 The abdomen is usually not considered when there are abdominal scars that will preclude incorporating zones of tissue that would be needed for the reconstruction or when the patient is morbidly obese.
The topic of complications is discussed and reviewed with all patients considering total autologous reconstruction. Known complications include bleeding, infection, scar, flap failure, abdominal bulge or hernia, delayed healing, deep venous thrombosis, and further surgery. Success of an operation is dependent upon a variety of factors; however, flap survival is usually the primary concern. Personal success with the DIEP, free TRAM, and pedicle TRAM has been 98%. The risk of an abdominal bulge has ranged from 4% to 6% after a DIEP flap, 5% to 10% after a free TRAM flap, and 10% to 15% after a pedicle TRAM.9-11 A postoperative bulge or hernia is not usually observed after an SIEA flap because the fascia and muscle are not violated. Secondary operations of the anterior abdominal wall have been performed in approximately 20% of women.12 These have included elective procedures in 10% (scar revision, recontouring, and liposuction) and necessary procedures in 10% (bulge repair, hematoma evacuation, neuroma excision, debridement, and wound closure).
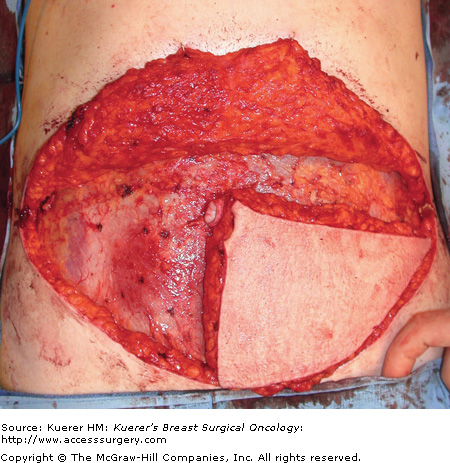
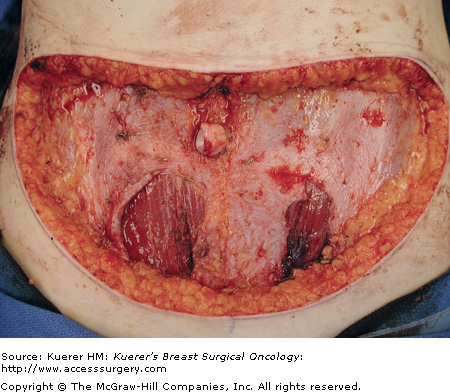
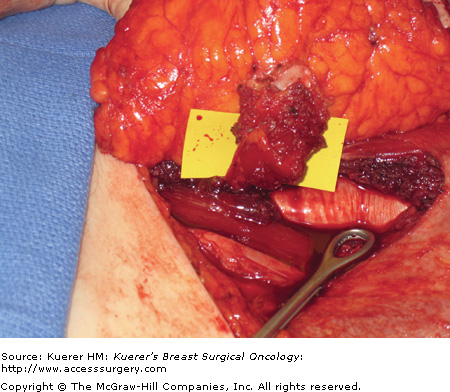
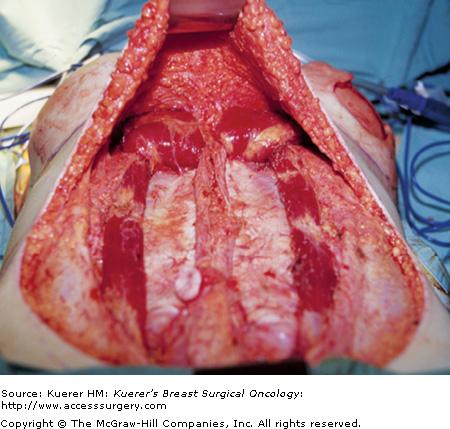
As previously mentioned, the abdomen is the preferred donor site for the majority of breast reconstruction procedures. It can be reasonably stated that the complexity of raising a given abdominal flap is directly related to the degree in which the abdomen musculature and anterior sheath are preserved. The SIEA flap does not violate the anterior rectus sheath or rectus abdominis muscle (Fig. 81-1) However, the superficial inferior epigastric vessels are present in roughly 60% of patients and suitable for microvascular anastomosis in approximately 30%. The DIEP flap requires an anterior rectus sheath incision and a myotomy in order to dissect out the perforator (Fig. 81-2). No muscle is removed. The blood supply is derived from the deep inferior epigastric artery and vein, which is present in all women and usually the dominant vascular system. The free TRAM by definition will include a segment of the rectus abdominis muscle and the anterior rectus sheath (Fig. 81-3). This flap is preferred for very large volume breast reconstruction or when the abdominal perforators are deemed inadequate. The pedicle TRAM usually results in sacrifice of the entire rectus abdominis muscle, although lateral preservation is sometimes possible (Fig. 81-4). A classification for the various types of muscle sparing has been established (Table 81-1).10
| Muscle-Sparing Technique | Definition (Rectus Abdominis) |
|---|---|
| MS-0 | Full width, partial length |
| MS-1 | Preservation of lateral segment |
| MS-2 | Preservation of lateral and medial segment |
| MS-3 (DIEP) | Preservation of entire muscle |
The frequency and incidence for each particular flap is variable and dependent upon the skill and experience of the reconstructive surgeon. In this author’s practice, a DIEP flap is performed in 80% of women, a free TRAM in 15%, and a pedicle TRAM or SIEA flap in the remaining 5%. The factors responsible for this are based on body habitus, quality of the perforators, integrity of the deep inferior epigastric artery and vein, and the presence and caliber of the superficial inferior epigastric vessels.13 If the perforators are suitable and the volume requirements are acceptable, then a DIEP flap is usually performed. In the event that the perforators are deemed inadequate, a muscle-sparing free TRAM is usually performed. If the inferior epigastric vessels have been previously ligated, a pedicle TRAM flap is considered. Some women are averse to the total harvest of the rectus abdominis muscle. In these women, an alternative donor site or prosthetic reconstruction will be considered. If the SIEA and SIEV are of suitable caliber, then it is considered. A limitation of the SIEA flap is that the angiosome is usually limited to the ipsilateral flap; therefore, inclusion of zone 3 will more likely than not result in fat necrosis.14,15 Thus the SIEA flap is ideal for women having unilateral or bilateral breast reconstruction in which only a hemi flap is used. The aesthetic outcomes of the breast are similar regardless of the flap used, assuming that patient and flap selection has been appropriate.
One of the principle decisions for the microvascular surgeon is whether to perform a muscle-sparing free TRAM, DIEP, or SIEA flap.13,16-19 This decision is ultimately made based on the presence and quality of the perforating vessels supplying the adipocutaneous component of the anterior abdominal wall.17,20-22 The anatomic details of these blood vessels can be assessed preoperatively and/or intraoperatively. Preoperative assessment is best achieved using computed tomography (CT) angiography.23,24 With this technique, the location and caliber of the perforating vessel or vessels can be adequately determined. This technique has proven to be effective for many surgeons. The advantage of preoperative CT angiography is that the “guesswork” regarding whether a perforator is present or suitable is essentially eliminated, and the harvesting of a DIEP flap can be more reliably executed. In addition, the CT angiogram can alert the surgeon regarding the subfascial course of the perforator. Although not routinely performed in these authors’ practice, the benefits of preoperative imaging to facilitate perforator selection are appreciated.
Intraoperative assessment is equally effective in identifying the abdominal wall perforating vessels. Reliance on intraoperative assessment requires more experience because of the variability associated with perforator location, caliber, and number. The “Gent” consensus described the 5 most common perforator types, some of which are not suitable to adequately perfuse a flap.25 In general, for a perforator flap to be successfully harvested and transferred, a single perforating artery and vein of at least 1.5 mm in diameter is recommended. These vessels are usually located in the periumbillical region. If a dominant perforator arising from the deep system is not identified, it may be because the superficial inferior epigastric system is the more dominant.26 In this situation, one can consider performing an SIEA flap or a muscle-sparing free TRAM. The MS-2 muscle-sparing free TRAM is the authors’ preferred flap. With this flap, a small central segment of the rectus abdominis muscle and anterior rectus sheath (2-4 cm) is harvested, incorporating several small (smaller than 1.5 mm) vessels. The authors’ current algorithm for the selection of a DIEP or muscle-sparing free TRAM is depicted (Table 81-2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree