- ♦
The incidence of thyroid cancer is rapidly increasing in the United States, with 35,000 patients seen annually. Interestingly, mortality from thyroid cancer has remained unchanged over the past 25 years.
- ♦
The increase in thyroid cancers may be related to incidental diagnosis of thyroid cancer during investigations for other problems or subserial sectioning by pathologists enabling identification of microcarcinomas.
- ♦
The long-term outcome for well-differentiated thyroid cancer patients continues to be excellent, with a 5-year survival rate exceeding 95%. In spite of this, approximately 10% to 15% of patients present with locally advanced thyroid cancer involving the surrounding structures in the central compartment of the neck. The surgical management of these patients includes removal of all gross tumor, careful attention to extrathyroid extension of the disease, and appropriate surgical resection with presentation of vital structures.
- ♦
The incidence of advanced thyroid cancer is higher in long-standing thyroid tumors; it is also high in elderly males with generally aggressive histopathologic varieties, such as tall cell, insular, and poorly differentiated carcinomas. The larger the tumor, the more likely it will be locally aggressive with involvement of other structures in the central compartment of the neck. There clearly is a high incidence of local recurrence in these individuals and a higher incidence of regional and distant metastasis.
- ♦
Patients who presented with extrathyroid extension (ETE) in a Memorial Sloan-Kettering Cancer Centers (MSKCC) series had a 48% incidence of local recurrence, a 41% incidence of nodal involvement, and a 37% incidence of distant metastasis ( Fig. 2-1 ; from MSKCC data). It is crucial to achieve the best local control for long-term survival. The structures most commonly involved include the strap muscles, recurrent laryngeal nerve, and tracheal wall ( Fig. 2-2 ; from Mayo Clinic data). The involvement of the esophagus and larynx is quite rare.
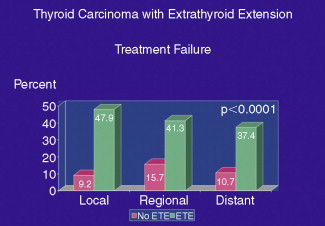
Figure 2-1
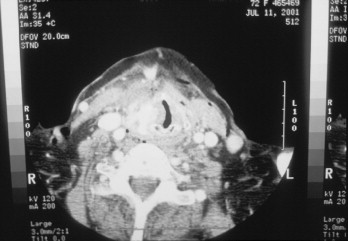
Figure 2-2
- ♦
Patients who experience recurrence of cancer in the central compartment may have tumors that involve the surrounding central compartment structures as well. A majority of these patients will require appropriate surgical excision of gross tumor; adjuvant therapy with radioactive iodine and external radiation therapy are required in selected patients.
Step 1
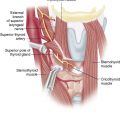
Surgical Anatomy
- ♦
The right recurrent laryngeal nerve originates from the vagus nerve and curves around the subclavian artery, going along the tracheoesophageal groove up to the cricoid cartilage, where it enters the larynx.
- ♦
Approximately 25% of the time the nerve may be anterior to the inferior thyroid artery or may be located between the branches of the inferior thyroid artery.
- ♦
The recurrent laryngeal nerve may be injured in the tracheoesophageal groove, where it crosses the inferior thyroid artery, or most commonly at the ligament of Berry. Small vessels in the region of the ligament of Berry may cause annoying bleeding, and the nerve may be injured in an effort to control the bleeding in this region.
- ♦
A nonrecurrent recurrent laryngeal nerve may occur in 1% of individuals on the right side of the neck. If the preoperative computed tomography (CT) scan is suggestive of a retroesophageal subclavian artery ( arteria lusoria ), the individual is likely to have a nonrecurrent recurrent laryngeal nerve. The nonrecurrent nerve is rarely present on the left side. The tumor may be adherent to the cricoid cartilage or first tracheal ring, where complete surgical resection is crucial because, if the recurrence occurs in this area, future control and surgical resection may be quite difficult.
- ♦
The superior laryngeal nerve arises from the inferior ganglion of the vagus nerve and tracks along the superior thyroid vessels medial to the artery, inserting in the cricothyroid muscle. The best way to avoid injury to this nerve is to pull the superior pole inferiorly and laterally, open the space between the superior thyroid vessels and the cricopharyngeus muscle (Joll’s triangle), and ligate the vessels close to the thyroid gland.
- ♦
Identify the parathyroid glands on the surface of the thyroid gland and dissect between the thyroid and parathyroid glands, preserving an intact blood supply to the parathyroids.
- ♦
If the parathyroid gland is devascularized, obtain a frozen section on a small piece of the tissue and autotransplant the remaining parathyroid gland by mincing it into small pieces and inserting it into the contralateral sternocleidomastoid muscle. In patients with locally aggressive thyroid cancer, the parathyroid glands may be difficult to identify. There is clearly a high incidence of both temporary and permanent hypoparathyroidism.
Step 2
Preoperative Considerations
- ♦
Evaluation of the exact extent of the disease is important. Patients presenting with locally advanced thyroid cancer may have symptoms of hoarseness of voice, tightening of the neck, dysphagia, or shortness of breath. If any of these symptoms are present, the clinical evaluation may suggest a frozen central compartment or tumor adherent to the surrounding structures in the neck. Preoperative evaluation should include indirect laryngoscopy to evaluate vocal cord function and appropriate imaging studies, such as ultrasound and CT scan.
- ♦
Computed tomography scan is best performed without contrast to facilitate postoperative radioactive iodine treatment. However, if the imaging studies are unsatisfactory, a CT scan with contrast may be performed for better evaluation of the extent of the disease. A preoperative needle biopsy will confirm the diagnosis of malignancy in most cases. Imaging studies are helpful to evaluate if the tumor is adherent to the trachea or larynx or is invading these structures with involvement of the submucosa or the lumen. The extent of surgery will differ in these scenarios. Preoperative medical evaluation, including pulmonary function tests, is important. Preoperative esophagoscopy, tracheoscopy, and bronchoscopy will be helpful to evaluate if there is any submucosal or intraluminal disease extension. Figure 2-3 shows the advanced nature of the locally aggressive cancer involving the entire left lobe with extension of the isthmus and esophageal musculature. Figure 2-4 shows locally aggressive thyroid cancer with paralyzed left vocal cord and calcification.
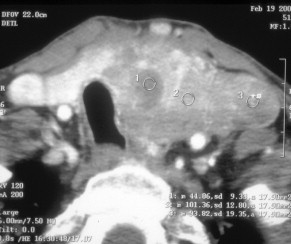
Figure 2-3
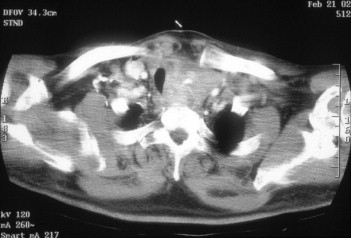
Figure 2-4
- ♦
Patients presenting with luminal involvement will require appropriate surgical resection of the trachea. Figure 2-5 shows extensive involvement of the cricoid cartilage with destruction of the cartilage, requiring total laryngectomy. Involvement of the esophageal mucosa is quite rare. However, involvement of these structures is fairly common in recurrent thyroid cancer. If the patient has had previous surgical procedures, a thorough evaluation of the previous operative records, pathology, extent of surgery and extent of disease, and the nature of recurrence are important preoperative steps.
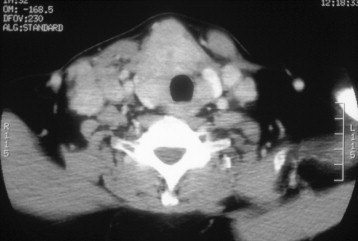
Figure 2-5
- ♦
Documentation of vocal cord function is crucial. If the patient presents with an ipsilateral paralyzed vocal cord, utmost care must be given to preserve the contralateral recurrent laryngeal nerve and achieve satisfactory surgical resection of the tumor in the ipsilateral tracheoesophageal groove by resecting the nonfunctioning recurrent laryngeal nerve.
- ♦
Ultrasound and ultrasound-guided needle biopsy are helpful to confirm the diagnosis of malignancy, so that appropriate complete resection can be undertaken. Those elderly individuals with advanced thyroid cancer necessitating sacrifice of vital organs should undergo a positron emission tomography (PET) study to evaluate the possibility of distant metastasis. An ultrasound-guided needle biopsy is helpful to confirm the diagnosis and rule out anaplastic thyroid cancer. If there is any suspicion of anaplastic thyroid cancer by rapid growth and involvement of the nerve and the trachea, a core biopsy may be considered because most patients with anaplastic thyroid carcinoma are not candidates for radical surgical resection. Figure 2-6 shows long-standing locally aggressive thyroid cancer with massive extension in the retrotracheal area and esophageal region with calcification.
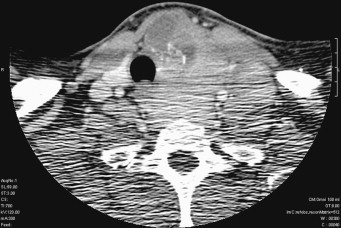
Figure 2-6
- ♦
Even though antibiotics are not necessary for routine thyroidectomy, if extensive dissection is anticipated in the central compartment, preoperative antibiotics may be considered and continued for a period of 24 hours. Broad-spectrum antibiotics, such as a cephalosporin or clindamycin, are generally preferred.
Step 3
Operative Steps
Anesthesia
- ♦
Preoperative evaluation in the clinic will guide the operating surgeon to more easily intubate patients with locally aggressive thyroid cancer.
- ♦
Intubation should be nontraumatic to avoid any postoperative laryngeal edema or tracheal irritation.
- ♦
A small endotracheal tube, such as #6 or #6½, should be used.
- ♦
The tip of the endotracheal tube should be well below the vocal cords to avoid any cuff-related trauma to the vocal cords.
- ♦
The endotracheal tube should be placed at the level of 24 to 26 cm, because there is considerable slackening and withdrawal of the endotracheal tube and the cuff may abut the vocal cords.
Positioning
- ♦
Standard thyroidectomy positioning involves a supine position with the head on the head plate, so that the head can be extended as necessary. Three flat sheets should be placed under the shoulder for appropriate extension of the neck.
- ♦
The neck should be prepared from the lip to the nipple. If there is any concern about the extent of surgery, the chest should be prepared should there be any need for sternal split, either for appropriate excision of the tumor or for control of bleeding in the mediastinum.
- ♦
The endotracheal tube should be well secured. A transparent drape on the endotracheal tube and the chin area is helpful to allow observation of the endotracheal tube position and anesthesia connections.
- ♦
The nape of the neck should be completely separated by sterile drapes from the operative site to avoid contamination and lodging of the operative instrument in this unsterile area.
- ♦
Both hands should be tucked by the side of the body.
Special Instrumentation
- ♦
Even though most of these patients do not require special instrumentation, surgical loops and microclamps are quite helpful for delicate and meticulous dissection around the recurrent laryngeal nerve.
- ♦
Monopolar and bipolar cautery are used, especially to control bleeding near the recurrent laryngeal nerve.
- ♦
A harmonic scalpel can be helpful in radical surgical procedures to cut the strap muscles and ligate the superior thyroid pedicle. However, due consideration should be given to the financial costs of these instruments.
- ♦
Even though a nerve monitoring system (Medtronic or Gyrus) is not necessary for every case, there may be some merit in the use of a nerve monitor for individuals who present initially with an ipsilateral paralyzed vocal cord, to avoid any injury and protect the nerve on the contralateral side. However, it is vitally important for the operating surgeon to understand the false-negative pitfalls of a nerve monitoring system. A special endotracheal tube is required for nerve monitoring.
- ♦
Appropriate hemostatic agents, such as Surgicel, Gelfoam, or Avitene, may be used at the end of the surgical procedure.
Paratracheal and Central Compartment Clearance, Including Superior Mediastinum
- ♦
The incidence of central compartment and nodal metastasis is quite high in patients presenting with locally aggressive thyroid cancer. It is appropriate to identify the recurrent laryngeal nerve and dissect in the paratracheal area.
- ♦
Every effort should be made to avoid any injury to the parathyroid glands. This dissection may be quite tedious due to small blood vessels, and appropriate use of bipolar cautery is helpful.
- ♦
The paratracheal nodes should be dissected as low as possible in the superior mediastinum, including resection of lymph nodes at levels 6 and 7. The superior mediastinum can be easily cleared, down to the innominate vessels. Again, every attempt should be made to avoid any bleeding in the thymic area.
- ▴
The thymus can be pulled in the superior mediastinum or pushed deep down in the mediastinum and the lymph nodes cleared from the superior mediastinum. This is more important in patients with locally aggressive thyroid cancer and patients presenting with medullary thyroid cancer.
- ▴
- ♦
The lymphatic channels may open in this area, and the soft tissue is best tied with nonabsorbing suture material.
Recurrent Laryngeal Nerve ( Box 2-1 )
- ♦
The preoperative evaluation for recurrent laryngeal nerve function is crucial. If the nerve is paralyzed preoperatively, it is important to take utmost care not to injure the nerve on the other side. Otherwise the patient will end up with a permanent tracheostomy.
- ▴
A decision may need to be made whether the contralateral lobe needs to be removed. Usually it is important to remove the contralateral lobe to facilitate radioactive iodine ablation. However, in older people with an aggressive form of thyroid cancer that is generally nonradioiodine-avid, the contralateral lobe may be left alone.
- ▴
- ♦
If the nerve is paralyzed preoperatively due to tumor, the nerve should be sacrificed with appropriate clearance of the paratracheal area. The most crucial area is the region of the cricoid cartilage where the tumor may be adherent to the cricothyroid area. If the tumor is adherent to the cricoid cartilage, an anterior shave of the cricoid may be necessary.
- ♦
A functioning nerve is rarely sacrificed in the operating room unless it appears that gross tumor may be left behind. If a functioning nerve is to be sacrificed, it is very important to evaluate the contralateral side, because the tumor may also be adherent to the contralateral recurrent laryngeal nerve. The recurrent laryngeal nerve may be adherent to the paratracheal lymph nodes, and meticulous dissection of the nerve and peeling of the nerve off the tumor are important. A nerve hook may be helpful to retract the nerve carefully. It is vitally important to avoid a traction injury to the nerve or to the vasa nervorum.
- ♦
The paratracheal nodes may be adherent to the recurrent laryngeal nerve, and every effort should be made to separate the disease, carefully avoiding any trauma to the nerve or damage to the vasa nervosum. A nerve hook is helpful to retract the nerve and dissect the paratracheal lymph nodes off the recurrent laryngeal nerve.