Thyroid Disruptors
Elizabeth N. Pearce
Introduction
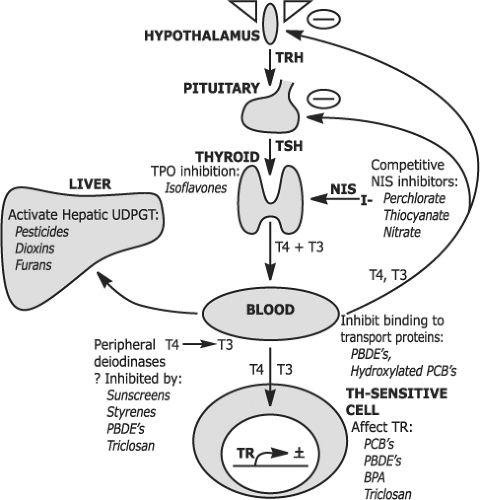
Over the past decades, there has been increasing concern about human and wildlife exposure to endocrine disruptors, chemicals that could disrupt endogenous hormone function. Over 100 naturally-occurring and synthetic substances have been reported to affect thyroid function or thyroid hormone metabolism (1,2,3,4,5,6,7). Because thyroid hormone is essential for normal development in utero and in infancy, environmentally mediated alterations in thyroid function are of particular concern for pregnant women and infants. The population risk conferred by disruptors is a function of their ability to perturb thyroid function and the extent of exposure (i.e., widespread environmental contaminants vs. substances encountered only by workers in specific occupations). Some potential thyroidal disruptors have been studied exclusively in vitro or in animal models; this discussion focuses primarily on exposures whose thyroid effects have been characterized in humans. A summary of the potential effects of these agents is shown in Figure 57.1.
Substances that Inhibit Thyroidal Iodine Uptake
The anions perchlorate, thiocyanate, and nitrate are competitive inhibitors of the sodium/iodine symporter (NIS). When present in sufficiently high concentrations, these substances will decrease the active transport of iodine into the thyroid and thereby decrease thyroid hormone synthesis. They could also potentially inhibit NIS-mediated uptake of iodine into breast milk, thus decreasing the amount of dietary iodine available to nursing infants. There has been recent concern that low
levels of perchlorate might pose a health hazard by inducing or aggravating underlying thyroid dysfunction (8,9,10).
levels of perchlorate might pose a health hazard by inducing or aggravating underlying thyroid dysfunction (8,9,10).
Perchlorate
Perchlorate salts are used as oxidizers in solid propellants for rockets and missiles, fireworks, road flares, matches, and air bag inflation systems. Perchlorate is also in Chilean nitrate fertilizers exported for use around the world. Low levels of perchlorate may also be found in the environment due to natural processes (11). Perchlorate has been detected in the drinking water of communities around the United States and worldwide. Since perchlorate is essentially not biodegradable, industrial contamination of water supplies is difficult and expensive to remove. Perchlorate has also been detected in foods such as lettuce and other produce, wheat, cows’ milk, wine and beer, and multivitamins (including prenatal multivitamins). Most US perchlorate exposure likely occurs through the diet rather than the water supply (12). Perchlorate exposure appears to be ubiquitous. In the US population, perchlorate was detectable in all 2,820 spot urine specimens from the 2001–2002 National Health and Nutrition Examination Survey (NHANES) with a median urine concentration of 3.6 μg/L (13). Among the 36% of women with urinary iodine values <100 μg/L in the NHANES data set, there was a significant positive correlation between urinary perchlorate concentrations and serum TSH and an inverse correlation between urinary perchlorate concentrations and serum T4 values (14). Among women with urinary iodine values >100 μg/L, there was a positive association between urinary perchlorate concentrations and serum TSH, but there was no association between urinary perchlorate concentrations and serum T4 values. There were no significant associations between urinary perchlorate concentrations and thyroid function values in men, irrespective of their urinary iodine concentrations.
However, the administration of 3 mg perchlorate to normal volunteers throughout the day for 14 days did not affect serum TSH, thyroid hormone concentrations, or the 24-hour thyroid 123I uptake (15). In a second study, 10 mg perchlorate daily for 14 days also had no effect on thyroid function tests in spite of a 50% decrease in the thyroid 123I uptake (16). Volunteers who received doses ranging from 0.5 to 35 mg perchlorate daily for 14 days had no change in serum TSH, T4, or T3 concentrations; there was a slight decrease in the thyroid 123I uptake at the 1.4 mg and higher doses, but not at the 0.5 mg dose (17). Normal volunteers who received daily doses of 0.5 or 3.0 mg perchlorate for 6 months had no changes in serum TSH, thyroglobulin, T4, FT4 index, total T3, and the thyroid 123I uptake, although this study was underpowered (18).
An occupational study examined 29 men working in a factory producing ammonium perchlorate who had been exposed to high-level airborne perchlorate in 12-hour shifts 3 to 4 days/week for an average of 3 years (19). Thyroid function was normal and did not differ at the end of three 12-hour shifts compared to their 3 days away from the plant, apart from a decrease in the 14-hour thyroid 123I uptakes. Thyroid ultrasounds did not reveal any significant abnormalities, and thyroid volumes were similar to 12 unexposed community controls.
The developing fetus is likely to be most vulnerable to the adverse effects of perchlorate exposure since thyroidal iodine turnover is highest in fetal life and the fetus requires adequate thyroid hormone for normal neurodevelopment. A Chilean study found that thyroid hormone and TSH levels in pregnant
women and their neonates did not vary among three towns with drinking water perchlorate concentrations of 0.5 μg/L, 6 μg/L, and 114 μg/L (20). However, the women in all three towns had high urinary iodine concentrations (median 269 μg/L), which may have made them less vulnerable to the adverse effects of perchlorate. In Israel, neonatal T4 levels did not differ in the infants of women who had consumed drinking water with high compared to low perchlorate concentrations during pregnancy (21). An ecologic study in California found increased neonatal TSH levels in communities with drinking water perchlorate concentrations >5 μg/L compared to communities with lower drinking water concentrations (22). However, there were no correlations between urinary perchlorate concentrations and first-trimester serum free T4 or TSH values in a group of 1,641 pregnant women from Cardiff, Wales and Turin, Italy, including the majority who had urinary iodine concentrations <100 μg/L (23). Similarly, no associations were detected between urine perchlorate concentrations and thyroid function among 134 women from Los Angeles and 107 pregnant women from Córdoba, Argentina (24).
women and their neonates did not vary among three towns with drinking water perchlorate concentrations of 0.5 μg/L, 6 μg/L, and 114 μg/L (20). However, the women in all three towns had high urinary iodine concentrations (median 269 μg/L), which may have made them less vulnerable to the adverse effects of perchlorate. In Israel, neonatal T4 levels did not differ in the infants of women who had consumed drinking water with high compared to low perchlorate concentrations during pregnancy (21). An ecologic study in California found increased neonatal TSH levels in communities with drinking water perchlorate concentrations >5 μg/L compared to communities with lower drinking water concentrations (22). However, there were no correlations between urinary perchlorate concentrations and first-trimester serum free T4 or TSH values in a group of 1,641 pregnant women from Cardiff, Wales and Turin, Italy, including the majority who had urinary iodine concentrations <100 μg/L (23). Similarly, no associations were detected between urine perchlorate concentrations and thyroid function among 134 women from Los Angeles and 107 pregnant women from Córdoba, Argentina (24).
Iodine, required for infant nutrition, is secreted into breast milk via NIS (25), and this process may be inhibited by perchlorate. A recent study measured perchlorate in the breast milk of women from around the US and found detectable levels in all 36 samples (range 0.6 to 92.2 μg/L) (26). Breast milk iodide and perchlorate concentrations were inversely correlated in the six samples with perchlorate concentrations ≥10 μg/L, although there were no correlations between breast milk iodide and perchlorate in the full data set. In a study of 56 Boston-area lactating women, perchlorate was detectable in all breast milk samples (median, 9.1 μg/L) (27). However, there were no significant correlations between breast milk iodine and perchlorate concentrations, including in the subset of 23 women whose breast milk perchlorate concentrations were ≥10 μg/L. It has been shown that perchlorate itself is transported into breast milk via NIS (28). In a study of 92 full-term infants, higher urinary perchlorate, nitrate or thiocyanate was associated with higher urinary TSH values (29). However, the correlation between urine and serum TSH was relatively poor (Spearman correlation coefficient 0.49) in the subset of 50 infants for whom serum testing could be performed and there were no significant associations between perchlorate and serum thyroid function tests in those 50 infants. A preliminary study in 64 mother–infant pairs found no associations between maternal breast milk or infant urine iodine concentrations and infant thyroid function at 2 months of age (30). Overall, the effects of low-level environmental perchlorate exposure on thyroid function remain unresolved.
Thiocyanate
Thiocyanate is about 15 times less potent than perchlorate as an NIS competitor (31). Cigarette smoke contains cyanide that is metabolized to thiocyanate. Thiocyanate is also a metabolite of cyagenic glucosides present in plant foods such as cassava, cabbage, turnips, broccoli, brussels sprouts, and cauliflower. It has been reported that women who smoke during pregnancy are more likely to give birth to neonates with decreased serum T4 levels, increased TSH levels, and thyroid enlargement (32,33). Among Boston-area women in the first trimester of pregnancy, FT4I levels were lower in women who reported current smoking than they were in non-smokers (34). Other studies concluded that cigarette smoking decreases breast milk iodine concentrations (35,36). These effects are postulated to be related to thiocyanate exposure. It has also been shown that diets high in thiocyanate contribute to the development of goiter in iodine deficient regions (37). However, overall the effects of cigarette smoke on thyroid function appear to be complex and somewhat contradictory. Large population studies have demonstrated lower serum TSH levels (38) and higher free T4 and free T3 levels (38,39) in smokers than nonsmokers; the mechanism is unknown.
Nitrate
Nitrate is about 240 times less potent than perchlorate as a competitive inhibitor of NIS (31). Nitrates occur naturally in soil and groundwater due to the decomposition of organic materials, and are present in plants. Sodium nitrite is also used as a preservative in cured meats and other foods. In the United States, the average daily dietary intake of nitrate in adults is about 75 to 100 mg, with about 80% to 90% from vegetables such as beets, celery, lettuce, and spinach (40). Vegetarians may have nitrate intakes of up to 250 mg/day. In addition, inorganic nitrates are used as fertilizers. High nitrate ingestion may occur due to contamination of the water supply by human sewage or livestock manure, especially from feedlots, or by runoff from farmland. The World Health Organization has defined the safe upper limit for nitrate in drinking water as 50 mg/L (41) and the U.S. Environmental Protection Agency (EPA) has set a maximum contaminant level at 45 mg/L (42); these guidelines were adopted to protect against methemoglobinemia in bottle-fed infants rather than because of concerns about thyroid health.
Among 3772 iodine-sufficient adults in the Study of Health in Pomerania, there was no cross-sectional association between urinary nitrate concentrations and thyroid volume by ultrasound (43). Similarly, in 10 healthy volunteers, no changes in thyroid function tests or radioactive iodine uptake were found following 4 weeks of the daily ingestion of 15 mg/kg sodium nitrate, far above the nitrate concentration typically ingested in the US diet (44). Recent studies have described the effects of very high nitrate exposures due to drinking water contamination in areas of Eastern Europe. Among iodine-sufficient schoolchildren in a Bulgarian village where drinking water nitrate levels were 75 mg/L, the odds ratio for goiter was 3.01 compared to children in a nearby village where drinking water nitrate levels were only 8 mg/L (45). Another Bulgarian study found an odds ratio of 5.3 for thyroid dysfunction among pregnant women living in a village with high drinking water nitrate content (93 mg/L) compared to women in a village without high nitrate exposure (46). Finally, sonographic thyroid volumes in iodine-sufficient Slovakian schoolchildren from a region with high drinking water nitrate levels (51 to 274 mg/L) and the prevalence of subclinical hypothyroidism were significantly higher compared to age-matched children without high nitrate exposure (47).
Two recent studies have suggested an association between high nitrate ingestion and thyroid cancer. An ecologic study in 21,977 Iowa women found no effect of drinking water nitrate concentrations on thyroid function, but did find an increased relative risk (2.6; 95% CI 1.1 to 6.2) for thyroid cancer with higher nitrate exposures (48). Among 490,194 participants
in the NIH-AARP Diet and Health Study, increased thyroid cancer risk was observed in men, but not women, with higher self-reported dietary nitrate intakes (49).
in the NIH-AARP Diet and Health Study, increased thyroid cancer risk was observed in men, but not women, with higher self-reported dietary nitrate intakes (49).
Compounds with Direct Actions on the Thyroid Hormone Receptor
Polychlorinated biphenyls Polychlorinated biphenyls (PCBs) are paired phenyl rings with different degrees of chlorination. PCB manufacture for use as coolants and lubricants in transformers, capacitors, and other electrical equipment began in the early 20th century and peaked in the 1960s. There are 209 possible PCB congeners, and most commercial PCB formulations included mixtures of 60 to 90 of these. Starting in the late 1960s, there were increasing concerns about the toxicity of PCBs and their ability to persist in the environment. Due to these concerns, production of PCBs was outlawed in the U.S. in 1979, in Germany in 1983, and in most other developed countries about 25 years ago. Since it was drafted in 2001, over 180 countries have ratified the Stockholm Convention on Persistent Organic Pollutants, which calls for a ban on the use of PCBs and other chemicals, including dioxins and hexachlorobenzene (HCB), which may persist in the environment for long periods and spread over wide geographic areas. It has been estimated that a total of about 1.5 million metric tons of PCBs were produced worldwide before bans were imposed, and although levels have decreased, PCBs remain widespread in the environment and the food chain. Most human PCB exposure is via food sources, especially fish (50).
PCBs are lipophilic and tend to concentrate in adipose tissues and serum. Their biologic half-life in humans is up to 7 years (51). They may also be present in relatively high amounts in breast milk. In 1989, the World Health Organization reported that in Belgium, Germany, and the Netherlands, the countries with the highest reported levels, breast milk PCB concentrations ranged from 392 to 762 μg/kg (52). Breast milk monitoring programs worldwide over the last three decades have demonstrated decreasing amounts of PCBs in breast milk as a result of increased regulation of these compounds (53).
The structure of PCBs is similar to that of thyroid hormone, and they are thought to bind to and interact with the thyroid hormone receptor (54). PCBs may act as TH receptor agonists or antagonists, with effects that may be specific to different congeners and/or their metabolites (5). These interactions are likely complex, and remain poorly understood. In rat studies, PCB exposure is consistently associated with low serum T4 levels, although the relationship between PCB exposure and thyroid function in humans has been less clear (5,55,56,57).
In the NHANES 2001–2002 study, associations between total serum PCB burden and TSH and T4 were inconsistent across age and gender groups: PCB exposure was inversely related to serum T4 levels and positively related to serum TSH in older women but was inversely associated with serum TSH in older men (58). Effects in other non-pregnant populations have been variable (59,60).
Multiple studies have demonstrated that prenatal exposure to PCBs is associated with decreased cognitive function in children, especially executive function, verbal abilities, and visual recognition memory (61,62). One hypothesis is that these adverse neurocognitive consequences are due to a PCB-induced state of relative hypothyroidism in the developing brain, although the evidence for this has not been consistent in animal studies (5). Several human studies have examined the effects of PCB exposure on thyroid function in pregnancy. One study of 78 Dutch women found a negative association between PCB exposure, as assessed by breast milk levels, and serum T4 and T3 within 2 weeks following delivery (63). Another found an inverse association between PCB exposure and serum T3 concentrations in 101 Canadian pregnant women (64). Among 182 pregnant women from the Faroe Islands, serum TSH was negatively correlated with PCB exposure, although this relationship was not statistically significant (65). In a cohort of 118 Taiwanese women, PCB levels were inversely related to free T4 in cord blood (66). In 334 pregnant women from California, PCB exposure was inversely correlated with serum free T4 concentrations (67). Finally, among 1090 pregnant Spanish women, levels of PCB congeners were inversely associated with serum free T3 and positively associated with serum free T4 (68). Unfortunately, anti-thyroid antibody status of the pregnant women was not assessed in any of these studies.
Although serum PCB concentrations are higher in breastfed infants than among those fed only formula (69), breastfeeding itself appears to protect infants from the adverse developmental effects of PCBs (70). Interestingly, a recent study suggested that the effects of PCBs on neonatal thyroid function may be modified by type of birth (71). Finally, high PCB exposure has been linked to increased thyroid volumes in iodine-sufficient regions, although the mechanism for this is unclear (57).
Polybrominated Diphenyl Ethers Like PCBs, the chemical structure of polybrominated diphenyl ethers (PBDEs), discussed below, is similar to that of T4 and T3. Hydroxylated PDBE metabolites may bind to thyroid hormone receptors with low affinity (72).
Bisphenol-A
Isopropylidenediphenol, or bisphenol-A (BPA) has been shown to bind to the thyroid hormone receptor and antagonize its activation (73). BPA is a plastic monomer used to produce polycarbonate plastic. Over 6 billion pounds of BPA are produced and over 100 tons released into the atmosphere worldwide annually (74). It is used in food containers, baby bottles, and reusable water bottles, and is found in epoxy resin linings of some metal food cans. It may leach from these containers into stored food and drink. BPA is also used in dental sealants. Studies from developed countries around the world have found BPA in human serum, urine, amniotic fluid, and breast milk (75). In a reference population of 394 U.S. adults, BPA was detected in 95% of urine samples with a median concentration of 1.28 μg/L (76). The U.S. EPA has defined the reference dose for BPA as 50 μg/kg/day. The European Union has set a no-observed-adverse-effect level (NOAEL) of 5 mg/kg/day.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree