THERAPEUTIC OPTIONS AND RESULTS BY TYPE OF PITUITARY ADENOMA
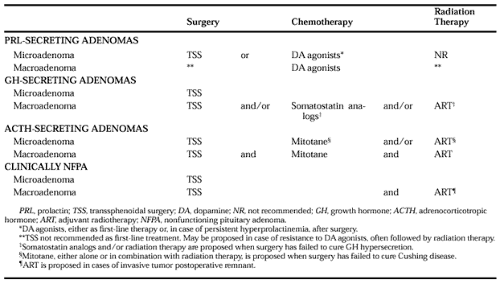
The recommendations for treatment of the different types of adenomas are summarized in Table 24-2.
GROWTH HORMONE–SECRETING PITUITARY ADENOMAS
THERAPEUTIC OPTIONS
Surgery and Radiotherapy.
Surgery and radiotherapy, as previously summarized, are commonly used in the treatment of acromegaly.
Medical Treatment.
Bromocriptine and other dopamine agonists are able to improve symptoms of acromegaly in a few patients and to decrease GH secretion.28,29
Somatostatin, the hypothalamic GH-release inhibitory factor and its analogs, SMS 201-995 (octreotide) and BIM 23014 (lan-reotide), are able to reduce GH secretion. The native somatostatin peptide has a half-life that is too short for it to be administered easily. However, octreotide, given subcutaneously three times daily, has been shown to control GH hypersecretion and to decrease tumor volume in a significant proportion of patients with acromegaly with relatively few side effects.30,31,32,33,34,35 and 36 The availability of a long-acting form of octreotide allows once-monthly intramuscular injections with the same efficacy.37 Another somatostatin analog, lanreotide, when encapsulated in microspheres, has a prolonged release; it has proved to be effective in lowering levels of GH and insulin-like growth factor-I (IGF-I), and often in decreasing the tumor mass of acromegalic patients, in a manner comparable to that of octreotide.38,39,40 and 41 The side effects of somatostatin analogs are benign. Digestive problems (i.e., abdominal cramps, diarrhea, flatulence) are minor and most often transitory. Cholelithiasis occurs in 10% to 55% of patients, with the incidence related to the duration of the study.30,33,34,36 Generally, it is asymptomatic and is treated conservatively. Despite the reduction in insulin secretion due to the use of somatostatin analogs, glucose-tolerance alterations are of minor significance. Somatostatin analogs are very expensive drugs and need to be given for the remainder of life.
Importantly, scintigraphy after administration of labeled octreotide (somatostatin-receptor scintigraphy) allows for the visualization of pituitary tumors.42 The resulting images are thought to reflect the concentration of the somatostatin receptors that are present at the surface of the tumor cells. However, scintigraphic findings are poor predictors of long-term results of treatment with somatostatin analog, regardless of the type of pituitary adenoma43 (also see Chap. 169).
CRITERIA OF CURE OF ACROMEGALY
The results of the various modes of therapy for acromegaly should be analyzed according to stringent criteria. Currently, “cure” (or good control) of acromegaly is defined by plasma GH levels: the mean of sequential sampling or the nadir after oral glucose administration should be <2.5 μg/L and the IGF-I level should be normal.44,45 Indeed, when these goals are achieved, the life expectancy of patients with acromegaly seems comparable to that of the general population.46,47,48,49,50 and 51 In the future, even more stringent criteria (nadir GH after oral glucose administration of <1 μg/L, and age- and sex-normalized IGF-I levels without clinical indications of activity) will probably be proposed for defining good therapeutic control of acromegaly.52 In the interim, the following section, using the currently accepted criteria for good control (plasma GH of <2.5 μg/L and normal IGF-I level), compares the effects of the different treatments as indicated by several studies.
RESULTS OF TREATMENT
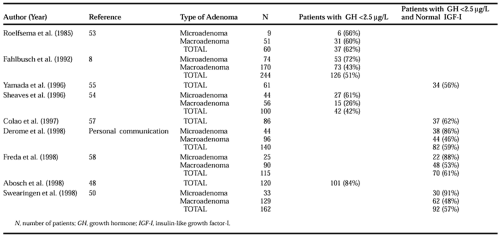
Transsphenoidal Surgery.
According to the stringent criteria indicated above, 42% to 62% of patients can be considered to have their disease “well controlled” by surgery alone.8,45,48,50,53,54,55,56,57 and 58 (Table 24-3). The results depend on the size of the tumor: surgery is able to cure 61% to 91% of patients with microadenomas and 26% to 60% of those with macroadenomas. When the macroadenoma is very large, or when parasellar or sphenoid sinus invasion has occurred, the cure rate decreases to 17% and 40%, respectively.8 Also, the success rate of surgery in patients with acromegaly varies according to preoperative GH levels: surgical treatment is successful in ˜70% of patients with preoperative GH levels of <10 μg/L, 43% to 55% of those with GH levels of 10 to 50 μg/L, and 18% to 40% of those with GH levels of >50 μg/L.8,54 The relapse rate after surgical cure is <3%53,54,59,60 (also see Chap. 12 and Chap. 23).
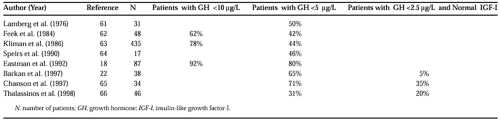
Irradiation Therapy.
Irradiation therapy is able to decrease GH levels in a large proportion of patients. Mean plasma GH levels of <5 μg/L are obtained in ˜50% of patients (40% to 80%, depending on the length of follow-up).18,22,61,62,63,64,65 and 66 However, when more stringent criteria for cure (as stated earlier) are applied, radiation therapy leads to cure of the disease in only 5% to 38% of the cases after a median follow-up of ˜7 years22,65,66 (Table 24-4). Irradiation is almost always followed by hypopituitarism, however, and the full impact on GH hypersecretion is delayed for many years. Preliminary results with radiosurgery are now available, but the follow-up is short. In one study,67 at 20 months, 20% of patients had “normalized” GH and IGF-I levels after radiosurgery, and the mean delay for “normalization” of hormonal parameters was reduced (1.4 years as
opposed to 7.1 years after conventional radiotherapy).68 Studies involving a higher number of patients followed for a longer period of time and assessed with more stringent criteria of cure are needed before one can conclude that radiosurgery is superior to conventional radiotherapy.
opposed to 7.1 years after conventional radiotherapy).68 Studies involving a higher number of patients followed for a longer period of time and assessed with more stringent criteria of cure are needed before one can conclude that radiosurgery is superior to conventional radiotherapy.
Therapy with Bromocriptine and Other Dopaminergic Agonists.
Treatment with bromocriptine or other dopaminergic agonists produces improvement in clinical symptoms of acromegaly in half of the patients. These drugs substantially decrease GH levels in some patients but only rarely normalize GH and IGF-I levels (i.e., in <10% of cases).28 Better results seem to be obtained with cabergoline than with bromocriptine, however; in a multicenter study, nearly 40% of patients acromegaly treated with cabergoline were reported to have normalized IGF-I levels.29
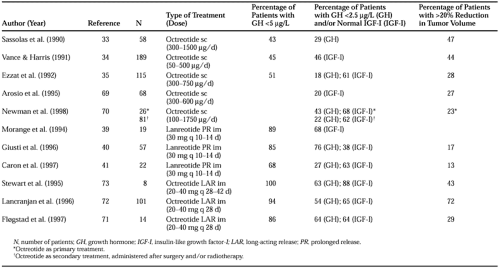
Therapy with Somatostatin Analogs.
Somatostatin-analog therapy has now gained wide acceptance in the medical treatment of acromegaly. GH levels are decreased in 50% to 80% of patients treated with octreotide subcutaneously three times daily.30,33,34,35 and 36,45,69,70 With this treatment, up to 50% of acromegalic patients may be considered as “cured” (GH plasma levels of <2 μg/L [20–30% of cases] and/or normal IGF-I [20–60% of cases]) (Table 24-5). Similar results are obtained with lanreotide LAR (long-acting release), 30 mg administered intramuscularly every 10 or 14 days (GH plasma levels of <2 μg/L [30–70% of cases] and/or normal IGF-I [40–70% of patients]),38,39,40 and 41 or with octreotide LAR. This latter drug has been administered intramuscularly every month at a dose of 20 to 30 mg (yielding GH plasma levels of <2 μg/L [50–60% of patients] and/or normal IGF-I [60–90% of cases])37,71,72 and 73 (see Table 24-5). Such variations in the data obtained from one study to another is probably explained by differences in the methods used for IGF-I assay and by differences in the inclusion criteria used. Thus, in some of the studies assessing the efficiency of long-acting forms of somatostatin analogs, patients were included if they had previously been shown to be responsive to subcutaneous octreotide, whereas in others, patients were entered blindly, without any knowledge of whether or not they were responsive. As demonstrated by a multicenter prospective study, the efficacy of octreotide as primary treatment (in 26 previously untreated patients) proved to be equivalent to that of secondary treatment (in 81 patients previously treated with surgery and/or radiotherapy).70
A small reduction in tumor volume may be observed (in general at the level of the suprasellar expansion) in 15% to 70% of patients with acromegaly30,33,34,35,36 and 37,39,40 and 41,45,69,70,71,72 and 73 (see Table 24-5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree