(1)
Institute of Oncology “Prof. Ion Chiricuță”, Nuclear Medicine & Endocrine Tumors, Cluj-Napoca, Romania
Salus populi suprema lex esto.
—Health of the people should be the supreme law—Marcus Tullius Cicero
4.1 Basic Factors in Radiation Protection
One delicate issue in nuclear endocrinology is radiation protection. There are a multitude of documents, legislations and rules, recommendations, and approvals that endocrinologists should obtain from the national authorities before starting to work with nuclear products and to treat patients with radiopharmaceuticals.
Depending on the national legislation, there are different restrictions in the usage of radiopharmaceuticals. There are countries or states where the use of radiopharmaceuticals is allowed only for inpatients, while other countries permit treatments of the outpatients, restricted only by an established national dose limit.
In any of these conditions, endocrinologists should know the basic requirements of safety both for medical staff and for patient and his family. In this section of the book, there are provided several general rules available in direct relation with the basic principles of radiation protection, recognized worldwide.
All medical activities using ionizing radiation must be held under strict regulation respecting the legal requirements: the International Commission on Radiological Protection (ICRP) recommendations; European Union directives regarding medical exposure and basic safety standards; National Council on Radiation Protection and Measurements, legislation, and national codes of practice; and local hospital radiation protection arrangements, reporting, and record-keeping regulations.
The issues related to radiation protection are strictly dependent on the type of radiation; different rays need various modalities of protection to be efficient in relation with humans.
Radiation effects are deterministic and stochastic, also being influenced by the sensitivity of different types of cells to radiation.
Schematic Fig. 4.1 presents three different materials in relation with radiation protection.
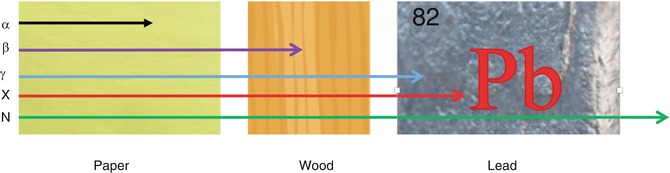
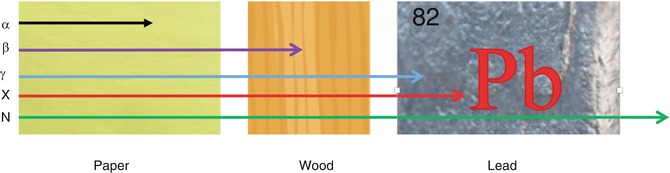
Fig. 4.1
Different materials in relation with radiation protection and ionizing radiations. α—alpha rays are stopped by a piece of paper of 2 mm; β—beta rays pass the paper, but are stopped by wood; γ—gamma rays pass through paper and wood, but are stopped by lead; X-rays pass the paper, wood and are stopped by lead; N-neutrons need special precaution
Considering the above example, we conclude that the attenuation of the radiation through a given medium might be summarized as follows: the thicker the absorbing material is, the greater is the attenuation, and the greater the atomic number of the material is, the greater is the attenuation. An important characteristic for attenuation is the half-value layer (HVL). HVL can be defined as the thickness of an absorbing material that reduces the radiation beam intensity to half of its original value.
The main factors affecting radiation doses in nuclear medicine are:
- 1.
The radionuclide used (the dose depends on the energy, type, and number of emissions). Gamma emitters provide imaging information but give local and long-range dose to other organs. Beta emitters do not give imaging information and give much higher local doses.
- 2.
The physical half-life of the radionuclide (the dose increases when half-life increases). The half-life should be long enough to complete the study but short enough for the radiation to effectively disappear after the study.
- 3.
The administered activity for the procedures (the dose increases when the activity increases). The activity should be kept to a minimum level but high enough to obtain the required diagnosis information.
- 4.
The target and critical organs. Although usually one organ is targeted, other organs also receive a radiation dose.
- 5.
Physiological factors. For example, in case of investigations involving isotopes of iodine, the radiation dose targeted to the thyroid may be decreased, by blocking it with stable iodine. In general, the radiation dose will be reduced, if there is fast excretion.
There are three basic requirements in daily medical practice with ionizing radiation:
- 1.
No practice shall be adopted unless its introduction produces a positive relevant benefit (justification).
- 2.
All exposures shall be kept as low as reasonable achievable—ALARA principle (optimization).
- 3.
The patient doses should not exceed those prescribed by the International Commission on Radiological Protection (ICRP dose limits).
All over the world, the national authorities have published and implemented regulations, which represent the basic legal patterns in order to be able to work with radiation. In Europe, the European Atomic Energy Community (EURATOM) has specific legislation regarding the basic safety standards for the health protection of the general public and workers against the dangers of ionizing radiation. This standard, 96/29/EURATOM, was implemented on May 13, 1996, and renewed by 2013/59/EURATOM.
The directive applies to all practices, which involve a risk from ionizing radiation, either from an artificial source or from a natural source, where natural radionuclides are processed because of their radioactive, fissile, or fertile properties. Prior authorization is required for the disposal, recycling, or reuse of radioactive substances or materials containing radioactive substances resulting from any practice, which is compulsory, reported, or authorized, unless the clearance levels established by the competent national authorities are complied with.
Before they are adopted or approved for the first time, member states must ensure that all new classes or types of practices involving exposure to ionizing radiation are justified regarding their economic, social, or other benefits outweighing any adverse effects they may have on health. Persons under the age of 18 may not be assigned to any work, which would make them exposed workers.
The effective dose for exposed workers is limited to 100 mSv during a period of 5 consecutive years and must not exceed 50 mSv/year.
As soon as a pregnant woman or nursing mother informs an undertaking of her situation, she may not be assigned to work involving a significant risk of bodily radioactive contamination.
Regarding the medical exposure directive, EURATOM has established the effective dose limits, which must be complied with by the authorized personnel (occupational dose limits) and by the general public (public dose limits).
The effective dose limit for the occupational personnel (workers with ionizing radiation) is 20 mSv/year/averaged during defined periods of 5 years (Table 4.1).
Table 4.1
The effective dose limits for authorized personnel
The annual dose limits (mSv) | |
|---|---|
Whole body | 20 |
Lens | 150 |
Skin (cm2) | 500 |
Hands and feet | 500 |
Areas where there is a risk of exposure must be designated as controlled or supervised areas; designation depends on the extent of likely exposure.
Controlled and supervised areas must include: monitoring and recording of the activities, doses and dose rates, lay down working instructions, indication of area types, nature of the sources, and correct signs for hazardous risks.
Controlled areas must be delineated and must have controlled access.
The effective dose limit for the general public is 1 mSv in a year (Table 4.2).
Table 4.2
The effective dose limits for general public
Annual dose limits (mSv) | |
|---|---|
Whole body | 1 |
Lens | 15 |
Skin (cm2) | 50 |
Hands and feet | 50 |
Justification and optimization of the ionizing medical procedures underline that the ionizing radiation exams must outweigh radiation risk. The results may be sufficiently consistent to improve the management of the patient. Any errors should be avoided in any part of the procedure starting from patient selection to the interpretation of final results. The misadministration leads to an increased radiation dose not only to the patient but also to the staff.
4.2 Staff Protection in Nuclear Medicine Units
For staff protection, there are several rules that must be respected: adequate dose monitoring, continuous education and training, implementation of local hospital rules, informing the supervisor as soon as a pregnancy is confirmed, employer must undertake risk assessment, reassignment of staff if required, restriction of tasks if required (e.g., injection), remember principles of time and distance and shielding, and escort staff for nuclear medicine patients must not be pregnant.
Radiation protection measures for handling radiopharmaceuticals:
Wear dedicated single-use coat.
Remove coat when leaving the area.
Wear gloves when handling radioactive materials or containers that may have been contaminated.
Wash and monitor hands frequently.
Do not eat, drink, or smoke in an area where radioactive materials are used.
Remove gloves when leaving the area.
Work in a suitable contained workstation.
Use different gloves to touch instrument switches.
Prepare all materials required before starting to handle radioactive materials so that there is no need to open recipients, etc.
Routine quality control of equipment.
Practical information for pregnant and breastfeeding staff:
Unborn child should be protected as a member of the public.
Radiation dose should be limited to 1 mSv after declaration of pregnancy.
Breastfeeding staff: in case of breastfeeding, work must not involve significant risk of bodily contamination (e.g., iodine therapy).
4.3 General Measures to Reduce the Irradiation of Patient
Examination must be clinically justified.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree