(1)
Research Oncology, Guy’s Hospital, London, United Kingdom
Abstract
There is substantial evidence of deleterious health behaviour in males both in terms of high-risk activities and avoidance of contact with doctors. This manifests as delay in diagnosis and upstaging of disease with a consequent worsening of prognosis. The incidence of male breast cancer is rising worldwide and this is not just as a result of increasing lifespan in that age standardised rates are also increasing. Neonatal breast tissue demonstrates plasticity irrespective of gender. Normal male breast anatomy is similar to that of prepubertal females but is often overshadowed by the presence of gynaecomastia, particularly in the overweight. The lack of model systems including established human MBC cell lines has hindered research but with collaborative studies there is promise of better understanding and treatment for MBC in the future.
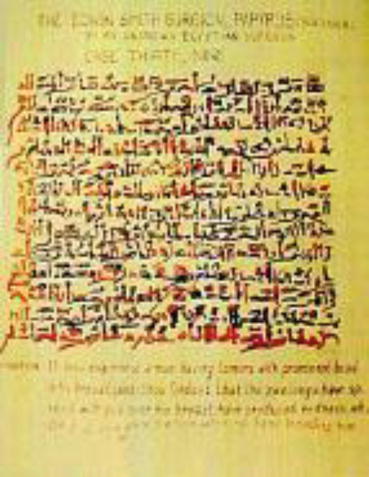
If thou examinst a man having bulging tumours on his breast and if thou puttst thy hand upon these tumours and thou findst them very cool, there being no fever at all when thy hand touches him, they have no granulation, they form no fluid, they do not generate secretions of fluid, and they are bulging to thy hand, thou shouldst say concerning him: One having bulging tumours: an ailment with which I will not contend Fig. 1.1. Edwin Smith Papyrus. 17th century BC.
Fig. 1.1
The Edwin Smith surgical papyrus
Introduction
Three thousand seven hundred years later, despite the advent of antisepsis, anaesthesia, cellular pathology and molecular biology, the outlook for men with advanced breast cancer remains poor. The ancient physician was correct, both in terms of the description of the disease and the dire prognostication. All is not gloom however: many men with early breast cancer treated promptly and correctly will live out their lives without recurrence.
Most men, when confronted with a personal diagnosis of breast cancer react with a mixture of concern and perplexity. Why have they developed a cancer normally associated with the feminine gender? What have they done, or not done, that has led to this potentially life-threatening disease? As with female breast cancer, epidemiology gives clues as to risk in the population but only rarely has been able to determine individual predisposition. It is this combination of a disease regarded by many as exclusively affecting females together with a male propensity to avoid medical attention that can lead to a life-threatening situation.
Male Health Behaviour
There are very few men who consider themselves to be at risk of breast cancer so that their “breast awareness” is at best desultory and at worst cavalier in ignoring signs and symptoms that would send their female partners hastening to seek medical help. Ample evidence is available from many countries of a gender mismatch in health attitudes and behaviour. As an example, a questionnaire on Japanese oral health administered to 245 men and 282 women who were aged between 20 and 29 years revealed significantly better oral care in females as measured by frequency of brushing teeth, use of dental floss and dental check-ups [1]. A survey of 27,344 rural Austrians showed that men were less likely to exhibit safe health habits and more likely to manifest potentially dangerous risk behaviour [2].
When invited for a health check at an inner city general practice in Cardiff, 115/22 (51%) of women attended compared with only 101/253 (43%) of males [3]. When 26,078 Canadian adolescents were asked about use of alcohol, marijuana and other illegal drugs in relation to off and on road vehicle driving, 10% reported driving while under the influence and 21% had been driven by someone in that state. Most reporting this behaviour were males [4]. Slovenians completed a questionnaire relating to non-use of seat belts in the front and rear seats and the major risk factor for failing to wear a seatbelt was being male [5].
In a study of health-related practices and behaviour, a self-administered questionnaire was given to students at Khon Kaen University, northeast Thailand [6]. Of the 539 participants 155 were male and 384 female, the mean ages being 19.7 and 19.6 respectively. The females were more likely to eat fruit, clean their teeth, avoid fat and not smoke compared with the males. Female students had significantly better eating habits than men and coronary heart disease prevention was practised more frequently by women, particularly those in the medical faculty.
Doctors are not immune to this ostrich-like behaviour. In a Nepalese study examining prevalence of alcohol and substance use among students and junior doctors, 64% of males and 32% of females had indulged [7]. Cannabis smoking was confined to males. In a longitudinal study of doctors that started when they were medical students while although women reported more ailments than men they took less sick leave. Cutting across countries and ages this gender difference regarding health, lifestyle and proactivity characterises the frequent delay in seeking medical advice for male breast cancer.
Delay in MBC
The first large series of MBC cases came from the Memorial Hospital in New York and included 146 men with histologically confirmed carcinoma [8]. Of those with known country of origin and religion, 42% were Jewish. The symptom duration ranged from 2 days to 44 years and only 22% consulted a doctor within 3 months. During a 30 year period, 87 men with breast cancer were seen at MD Anderson Hospital and for the 40 with known symptom duration the delay was 12 months [9].
A large Danish series of 257 MBC cases reported a median delay of 6 months [10]. This reduction in symptom duration despite the relative age of the study could be a reflection of a well organised national health system, allied with improved health awareness. Ribeiro treated 292 males at the Christie Hospital Manchester and reported a reduction in delay with time [11]. For those treated between 1941 and 1961 the mean delay was 18.5 months compared with 11 months for those seen between 1962 and 1983. A later report from the Memorial Hospital indicated that the delay had reduced to 4.5 months [12], another from Wisconsin reported a median delay of 3 months [13] and a Canadian study showed a 4 month delay [14].
Five years after South Africa emerged from the apartheid era, Vaizey et al. reported that there was a considerable racial difference in length of delay [15]. For the 69 black patients the a median delay was 12 months, compared with 2 months for the 20 white and 2 Asian males. More recent work shows that in North Africa there is considerable delay ranging from 8 to 28 months [16, 17, 18]. In Western Europe there are delays of 3–6 months [19, 20], whereas in West Africa men wait for a median of 11 months [21]. These studies are summarised in Table 1.1.
Table 1.1
Median delay before consultation in MBC
Author | Number | Country | Delay in months (median) |
|---|---|---|---|
Treves 1955 [8] | 146 | USA | 9 |
Scheike 1973 [10] | 257 | Denmark | 6 |
Yap 1979 [9] | 87 | USA | 12 |
Ribeiro 1985 [11] | 292 | UK | 1941–61 18.5 1962–83 11 |
Borgen 1992 [12] | 104 | USA | 4.5 |
Donegan 1998 [13] | 215 | USA | 3 |
Goss 1999 [14] | 203 | Canada | 4 |
Vaizey 1999 [15] | 91 | RSA | Whites 2 months Blacks 12 months |
Ben Dhiab 2005 [16] | 123 | Tunisia | 8 |
Liukkonen 2010 [19] | 58 | Finland | 6 |
Cutuli 2010 [20] | 489 | France | 3 |
Bourhafour 2011 [17] | 127 | Morocco | 28 |
El Beshbeshi 2012 [18] | 37 | Egypt | 9 |
Ahmed 2012 [21] | 57 | Nigeria | 11 |
Age and Stage at Presentation
The major risk factor for development of MBC is increasing age, as shown in Table 1.2 [10, 16, 17, 18, 22–27]. These series were sequential and not selected as having operable disease. The median age at diagnosis in these series was 62 years. Stage is based on the TNM classification, and the proportion of MBC cases presenting with stage IV disease ranged from 3 to 92%. Considerable geographical variation is present. The highest rates of metastatic disease at diagnosis were reported from North Africa [17, 18, 19].
Table 1.2
Advanced stage at presentation of MBC
Author | Number | Age (median) | Stage III (%) | Stage IV (%) |
|---|---|---|---|---|
Schieke 1973 [10] | 257 | 65.2 | 42 | 12 |
Gough 1993 [22] | 124 | 62.5 | 35 | 11 |
Joshi 1996 [23] | 46 | 64 | 13 | 10 |
Ben Dhiab 2005 [16] | 123 | 65 | 63 | 29 |
Zhou 2010 [24] | 72 | 61 | 39 | 3 |
Bourhafour 2011 [17] | 127 | 62 | 50 | 29 |
Liu 2012 [25] | 58 | 32 | 3 | |
Teo 2012 [26] | 21 | 68
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|