TABLE 25.1 Rates of Device-Associated Infections per 1,000 Device-Days by Type of ICU in CDC NHSN Hospitals, January to December 2010 | |||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||
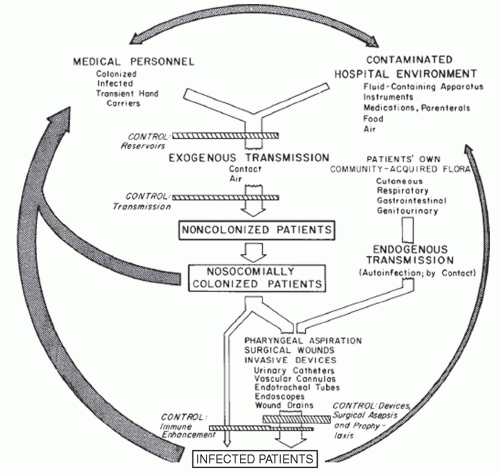
should have airborne infection isolation rooms for patients with tuberculosis or other airborne infections. For ICUs involved in the care of bone marrow transplant patients or hematologic malignancy, positive pressure isolation rooms using high-efficiency particulate air (HEPA) filtration should be available. All surfaces contiguous to the ICU patient should be wiped down with the general hospital disinfectant at least daily, and urine-measuring devices, a frequent reservoir of gram-negative bacilli, should be rinsed with a disinfectant after each use. Each ICU patient should have a dedicated stethoscope and sphygmomanometer.
TABLE 25.2 Strategies to Improve Hand Hygiene Compliance | ||
|---|---|---|
|
parachlorometaxylenol, and alcohol-based products (17). A number of before-after studies using time-series analysis and HAIs as the primary outcome in ICUs (15,16,30,31,32,33,34) have shown that alcohol-containing waterless hand rubs were associated with significant HAI reductions. Three large, well-conducted, randomized trials assessing the efficacy of chlorhexidine-containing hand hygiene products showed a 27% to 47% relative reduction in HAIs (30,33,34). The CDC recommendations for hand hygiene have been published (35), emphasizing hand antisepsis with an antiseptic-containing soap or detergent, or an alcohol-based hand rub: (a) before and after direct contact with patients or the environment and equipment in the immediate vicinity of the patient and (b) before performing invasive procedures, such as insertion of an intravascular device or urinary catheter. Alcohol-based waterless hand rubs are now widely used in hospitals for hand hygiene because of their convenience and broad-spectrum activity (17). However, all have limited efficacy with gross soilage so that visibly soiled hands should always be washed with antiseptic soap and water (36).
TABLE 25.3 Handwashing and Hand Antisepsis Recommendations from the CDC/HICPAC Guideline on Hand Hygiene | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||
mandates a multifaceted approach, encompassing antimicrobial stewardship, hand hygiene, and barrier precautions for HCWs in contact with high-risk patients. The CDC’s Campaign to Prevent Antimicrobial Resistance aims to prevent antimicrobial resistance in healthcare settings (44). The campaign centers on four main strategies: prevent infection, diagnose and treat infection, use antimicrobials wisely, and prevent transmission.
be placed in contact isolation, which requires a private room for the patient (or cohorting the patient in a semiprivate room with another patient who is also colonized or infected by the same organism). HCWs are expected to wear gloves on entry to the room and gowns if substantial contact with the patient or the environment is anticipated. Gloves and gowns should be removed and hands treated with a medicated hand hygiene product while still in the isolation room. Noncritical patient-care items should be dedicated; if reused, they must be disinfected between patients.
TABLE 25.4 Antimicrobial Usage Strategies for Reducing the Emergence of Antimicrobial Resistance in the Intensive Care Unit | |||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||
(55,56,59); two showed benefit with a reduction in all HAIs in ICU patients (relative risk reduction, 52% to 81%) (55,56).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree