The History of Diabetes
Donald M. Barnett
Leo P. Krall†
†Deceased
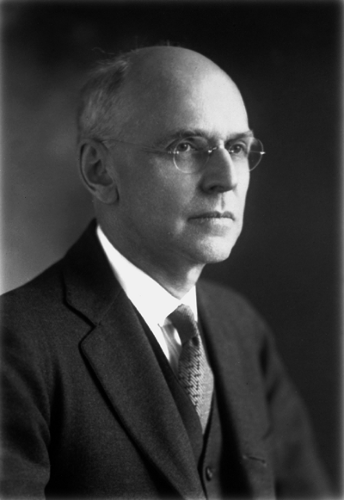
When Elliott Proctor Joslin first published his textbook The Treatment of Diabetes Mellitus more than 85 years ago in 1916, it represented the first rendition of its kind in the English language (1). During Joslin’s long professional life, he remained the senior editor for 10 editions, maintaining the same enthusiasm as he and his team continued to report the experience of the Joslin Clinic and increasingly that of other investigators. Elliott P. Joslin (1869–1962) (Fig. 1.1) was part of the last generation of physicians who received much of their postgraduate training in Europe (2). After his 1895 graduation from Harvard Medical School, he became inspired by the examples of the French and German medical schools that sought to combine laboratory and clinical medicine. From the start of his practice in 1898, he continued to attract assistants and students to observe and apprentice with him in the treatment of an increasing number of patients with this hitherto poorly defined condition, diabetes.
Fifteen years before the discovery of insulin, Joslin began collaborating with the physiologist Francis Benedict of the Carnegie Institute on studies of metabolic balance (3). Joslin’s simultaneous association with the young polymath investigator Frederick Allen at the Harvard Medical School also proved fortunate. Allen, who was observant of all the known literature on the subject up to that time, was able to translate his ideas from his experimental animal models to humans on the wards of the new Rockefeller Institute (4). By 1914, Joslin, desperate to lower the death rate from ketoacidosis in his mostly young patients with diabetes, combined Benedict’s balance study format with diets in a wide range of human subjects in near or actual acidosis (2). By 1917, he had become progressively convinced that he had developed a regimen that could extend the life expectancy of these fatally ill patients (5).
In his writings and lectures on diabetes, Joslin was an early proponent of several concepts, with two being especially important. First, as early as 1920 he emphasized the need to contain the “epidemic” of the disease by judicious diet and exercise (6); second, he pioneered patient education as a primary part of treatment. His goals were to prevent the onset of the disease or to retard its progression. To accomplish these aims, he created a freestanding clinic devoted to a single disease.
Joslin’s interest in all matters of medicine could be inferred from pictures on the walls of his office, as well as from the bas relief panels on the modern exterior of his institute, where sculptured portraits were displayed of many of his “medical saints,” as he phrased it, from Thomas Hunter, the father of comparative anatomy, to Charles Best, the “codiscoverer of insulin.” Three investigators of the 19th century particularly influenced Joslin’s world: Louis Pasteur, Claude Bernard, and Rudolf Virchow. Two were Frenchmen, Pasteur, who understood the cause-and-effect contributions of microbes in the pathogenesis of infection, and Bernard, who established modern physiologic investigation. The third investigator, Virchow, the leading German pathologist of his time, demonstrated that disease entities were characterized primarily by a disruption of the integrity of normal cellular health (7).
The story of diabetes and dates in the life of Joslin were closely intertwined. In 1869, the year of Joslin’s birth, Paul Langerhans,
a senior medical student in Virchow’s department, published his medical dissertation on pancreatic histology in which he described “clumps of cells,” which were named the islets of Langerhans shortly after his premature death in 1888 (8,9 and 10). By 1889, the year that Minkowski and Von Mering, in Strassburg, Germany, discovered the central role of the pancreas in diabetes (11,12), Joslin decided to spend a postgraduate year in physiologic chemistry at Yale’s Sheffield School of Science, an experience that led to his initial interest in diabetes. It was not until midcareer, when Joslin was in his early 50s, that the discovery of insulin ended years of frustration encountered in caring for desperately ill patients with diabetes.
a senior medical student in Virchow’s department, published his medical dissertation on pancreatic histology in which he described “clumps of cells,” which were named the islets of Langerhans shortly after his premature death in 1888 (8,9 and 10). By 1889, the year that Minkowski and Von Mering, in Strassburg, Germany, discovered the central role of the pancreas in diabetes (11,12), Joslin decided to spend a postgraduate year in physiologic chemistry at Yale’s Sheffield School of Science, an experience that led to his initial interest in diabetes. It was not until midcareer, when Joslin was in his early 50s, that the discovery of insulin ended years of frustration encountered in caring for desperately ill patients with diabetes.
By 1952 organizational efforts in many countries developed to the point that the International Diabetes Federation was formed to increase awareness of the disease and to promote better investigation and treatment programs worldwide. Elliott Joslin became honorary president of the International Diabetes Federation, confirming his role as the international “dean” in the cause of diabetes. By this time he had initiated the first population survey and follow-up studies demonstrating a surprisingly high prevalence rate of diabetes in a typical U.S. population, the study being carried out in his hometown of Oxford, Massachusetts. In addition, the prevalence rate was nearly equally divided among those people with undetected disease and those with diagnosed diabetes (13). These studies set the stage for early-detection programs countrywide sponsored by the American Diabetes Association.
Joslin and his early associates became identified with the conservative viewpoint that “good” control delayed or prevented microvascular complications, particularly in type 1 diabetes. This position inaugurated an intense nationwide 30-year debate that only ended in 1993 with the publication of the results of the Diabetes Control and Complications Trial (14), which clearly supported Joslin’s claim.
THE ROAD TO INSULIN
The story of the earliest recognition of diabetes and the path to the discovery of insulin is filled with marvelous insights as well as egregious errors, serendipity and futile labors, triumphs, and defeats. The best early evidence of a description of the symptoms of diabetes in the world’s literature is recorded in the Ebers papyrus that appears to date from 1550 B.C. This links the description of polyuria to Imhotep, a man of medicine, architecture, and magic, who was a high priest and minister to the Pharaoh Zosser in 3000 B.C. (15). Two Greek physicians in the Roman era, Galen (A.D. 130–201), who practiced in Rome, and Arateus of Cappadocia, delineated the disease further. Arateus is credited, despite the survival of only fragments of his documents, with some of the best descriptions of medicine in the ancient literature. In his work Acute and Chronic Diseases, he coined the term diabetes, meaning “siphon,” to explain the “liquefaction of the flesh and bones into urine” (16).
The following masterly description of severe diabetes by Arateus from about A.D. 150 represents the sum of our knowledge up until the second half of the 17th century (17):
Diabetes is a wonderful affection, not very frequent among men, being a melting down of the flesh and limbs into urine. Its course is of a cold and humid nature, as in dropsy. The course is the common one, namely, the kidneys and the bladder; for the patients never stop making water, but the flow is incessant, as if from the opening of aqueducts. The nature of the disease then, is chronic, and it takes a long period to form: but the patient is short-lived, if the constitution of the disease be completely established; for the melting is rapid, the death speedy.
In 1674, Thomas Willis, a physician, an anatomist, and a professor of natural philosophy at Oxford, discovered (by tasting) that the urine of individuals with diabetes was sweet (18). This was actually a rediscovery, for unbeknownst to him, an ancient Hindu document by Susruta in India in about 400 B.C. had described the diabetic syndrome as characterized by a “honeyed urine” (19). Willis could not pinpoint the chemical nature of the “sweet” substance, because a variety of different chemical substances could be equally sweet to the sense of taste. It was Matthew Dobson of Manchester, England, who demonstrated, in 1776, that persons with diabetes actually excrete sugar in the urine. After boiling urine to dryness, he noted that the residue, a crystalline material, had the appearance and taste of “brown sugar” (20).
Dobson’s definitive finding soon began influencing clinicians as to the possible causes of the disease and the bodily organs primarily involved. The prevalent view up to that time was that the kidneys were the major source of the problem, because its most striking signs and symptoms were the frequency and degree of urination. Some clinical observers also noted a tendency toward enlargement of the liver, which we now know to be usually due to intense infiltration of the organ with fat in persons with uncontrolled diabetes. In a case report, which also gave a detailed description of postmortem findings, Thomas Cawley reported in 1788 (without particular comment) on a shriveled pancreas with stones in a diabetic patient at autopsy (21). This may have been the first published reference
to the pancreas in relation to human diabetes, but no deductions were drawn regarding etiology.
to the pancreas in relation to human diabetes, but no deductions were drawn regarding etiology.
It was John Rollo, Surgeon General of the Royal Artillery, who in 1797 first applied the discovery of glycosuria by Dobson to the quantitative metabolic study of diabetes. Aided by William Cruickshank, “apothecary and chemist to the ordinance,” Rollo devised the first rational approach to the dietary treatment of the disease, shifting the view then current that the primary seat of the disorder was the kidneys to a view of its being the gastrointestinal tract (22). Rollo studied Captain Meredith, a corpulent man with adult-onset diabetes and severe glycosuria. Rollo made daily recordings of the amounts and kinds of food Meredith ate and weighed the sugar cake obtained by boiling Meredith’s daily urine output. Rollo noted that the amount of sugar excreted varied from day to day, depending primarily on the type of food ingested. “Vegetable” matter (i.e., breads, grains, fruits) increased glycosuria, whereas “animal” matter (i.e., meat) resulted in a comparatively lower excretion of sugar. Rollo and Cruickshank concluded, therefore, that the glycosuria was secondary to the “saccharification” of “vegetable” matter (i.e., carbohydrate-containing foods in the stomach and the influx of sugar into the body) and concluded that the “morbid” organ in diabetes was not the kidney but the “stomach,” which overproduced sugar from “vegetable” matter. The indicated treatment was thus a diet low in carbohydrates and high in fat and protein (22). It was not until the advent of insulin that this dietary prescription was altered significantly.
Although Rollo suspected the presence of excessive sugar in the blood of persons with diabetes, at that time there was no convincing proof of the existence of hyperglycemia. William Wollaston (1766–1828), a renowned chemist and physician, tried to measure “sugar” in the blood but failed to detect it, possibly because he assumed it had the same chemical characteristics as table sugar (19). In 1815, Chevreuil showed that blood sugar behaved chemically as if it were “grape” sugar (i.e., dextrose or glucose) (23). Only in the period 1914 to 1919 were specific methods of analysis devised and used to measure glucose as the major “reducing substance” in the serum and urine (24,25 and 26). Rollo’s predictions were confirmed—that in diabetes an increase in blood sugar level causes the excretion of sugar and that the “seat” of diabetes was outside the kidneys.
Lavoisier’s Legacy
A set of experiments initiated in the late 18th century deepened understanding of the basic metabolic principles of human physiology and had far-reaching consequences for medicine and for diabetes in particular. Antoine Lavoisier (1743–1794) established the concept of the respiratory quotient and with the aid of calorimetric studies measured oxygen consumption at rest and under different conditions, such as during food ingestion and work; however, his studies were interrupted by his death by guillotine during the French Revolution. A generation later, Baron Justus von Liebig (1803–1873) advanced the field of physiologic chemistry by determining that there were three categories of food: protein, carbohydrate, and fat. As described by Rosen (27), Liebig showed how protein was used to build up or repair the organism while carbohydrate and fat were used for fuel. He determined how much oxygen was needed to burn the different classes of food and how much energy was released as heat. Carl Voit, writing in 1865, described his teacher’s work in these terms: “Liebig was the first to establish the importance of chemical transformations in the body. He stated that the phenomena of motion and activity which we call life arise from the interaction of oxygen, food and the components of the body. He clearly saw the relation between metabolism and activity G52 and that not only heat but all motion was derived from metabolism….” Voit’s work, as carried on by his student Max Rubner in Germany and by his American students Graham Lusk and W. O. Atwater, made it possible to study metabolic activities more precisely and to apply the results to clinical and theoretical problems. Rubner, in 1888 to 1890, finally produced incontrovertible experimental proof that the principle of the conservation of energy held for living systems, a finding confirmed for humans by Atwater and Benedict in 1903 (28). In 1874 the unique respirations seen in diabetic ketoacidosis were de-scribed by Adolph Kussmaul as being deep and having long pauses between expiration and inspiration (29).
Turning their attention to the pancreas, clinicians in England, France, and Germany in the mid-1800s described cases of diabetes with postmortem findings of diseased, atrophic, or stone-filled pancreases. Speculations on the role of this organ in diabetes abounded, but the evidence was not at all convincing, because in the vast majority of patients with diabetes, the pancreas was of normal size and appearance at autopsy. With the pancreas being thought of only as a purely exocrine gland, the finding of pathologic lesions in the pancreas in a small group of diabetic individuals was interpreted as only a chance phenomenon.
In France, Claude Bernard was aware of the findings and speculations regarding the possible role of the pancreas in diabetes. To test this hypothesis, he ligated pancreatic ducts of dogs and/or injected them with oil or paraffin to block all secretion, which led to profound atrophy of the gland. Because only a few strands of what appeared to be lifeless scar tissue remained, Bernard assumed that the atrophy was indeed complete. Despite this, the animals showed neither glycosuria nor any other indication of diabetes (30). Such experiments also were performed by Moritz Schiff, with equally negative results. This “antipancreatic” viewpoint was thus immeasurably strengthened by the authoritative voices of the foremost physiologists of the age. Bernard’s celebrated findings of glycosuria after “piqûre” of the IVth ventricle drew attention to the possibility that alterations in the central nervous system could be etiologically related to diabetes. A lesion in the brain would cause hyperglycemia by way of the “visceral” nerves acting on the liver.
The Search for the Cause of Diabetes
Between 1840 and 1860, physiologic studies in metabolism as they relate to diabetes began their advance, especially in France under the leadership of Claude Bernard. His epoch-making discovery that blood glucose was derived in part from glycogen as a “secretion” of the liver thus identified the liver as a central organ in diabetes and explained how a diabetic patient whose liver was scarred by the end stages of cirrhosis might be “cured” of his hyperglycemia and glycosuria.
The two strongest forces arguing for a “pancreatic” factor in the etiology of diabetes were Apollinaire Bouchardat and E. Lancereaux. Bouchardat, who trained in organic chemistry and was an early pioneer in the study of fermentation and a professor of public health, did meticulous long-term studies on human diabetes. These began in 1835 and were gathered into his 1875 book, De la Glycosurie ou Diabète Sucré (31). He followed the essentials of Rollo’s dietary regimen in treating diabetes but added a very important therapeutic arm by encouraging hard physical labor, having observed ameliorative effects of muscular work on glycosuria and hyperglycemia. Yet above all, his clinical experience taught him to distinguish at least two different types of diabetes: the severe type in younger persons who
responded poorly to his regimen and the type in older, obese persons for whom the prescribed therapy of diet and physical exertion worked admirably. The clinical behavior of the two types of diabetes and the postmortem findings led Bouchardat to suggest that the more severe form was pancreatic in origin.
responded poorly to his regimen and the type in older, obese persons for whom the prescribed therapy of diet and physical exertion worked admirably. The clinical behavior of the two types of diabetes and the postmortem findings led Bouchardat to suggest that the more severe form was pancreatic in origin.
Lancereaux and his students came to identical conclusions about etiology and introduced the terms diabète maigre (diabetes of the thin) and diabète gras (diabetes of the fat) for the two common clinical forms of the disease (32). Because diabète gras was the more frequently occurring type, it now became understandable why severe pancreatic damage was found less frequently than expected. A pancreatic etiology for diabète maigre thus became an acceptable postulate, even though one could not yet form a sound notion about the mechanisms involved.
The concept that the body possesses glands that deliver their products directly to the blood (ductless or “blood” glands) gained substantial ground through Berthold’s study of castration in 1849 (33), the clinical description of Addison disease in 1849 (34), and the experimental ablation of the adrenal gland by Charles Brown-Séquard in 1856 (35).
Pancreatic Diabetes
A decisive turning point in the history of diabetes was marked by the experimental work of Joseph von Mering and Oscar Minkowski in 1889 (11,12). Von Mering was interested in the possible role of the pancreas in the digestion and absorption of fats. From the literature then available, primarily the writings of Claude Bernard, von Mering understood that it was virtually impossible for an animal to survive total removal of the pancreas. He consulted with Minkowski, the assistant to Albert Naunyn, the foremost European clinician in diabetes at that time. Undaunted by the previous experiments, von Mering and Minkowski operated on two dogs, and both animals survived the complete pancreatectomy. Within less than a day, these animals exhibited unexpected behavior—in particular, frequent and voluminous urination. Minkowski’s experience with severe human diabetes led him to examine the urine for sugar. During the next 2 years, Minkowski extended this serendipitous finding into an in-depth, now classic, study of experimental diabetes and its metabolic deviations. The study remains a model of scientific physiologic inquiry. He demonstrated clearly that the pancreas was a gland of internal secretion and that a small portion of the gland, when implanted under the skin of a freshly depancreatized dog, prevented the appearance of hyperglycemia until the implanted tissue was removed or had degenerated spontaneously.
Confirmation of these findings came very quickly from Hedon and coworkers in France. In 1893 Laguesse drew proper attention to the almost forgotten original observations of Langerhans and suggested the collections of interacinar cells (which he designated the islets of Langerhans) as a gland of secretion within the pancreas (36).
Thus, modern experimental and clinical endocrinology developed during the last decade of the 19th century. The term hormone was introduced by William Bayliss and Ernest Starling in 1902 to designate a specific chemical material elaborated by a ductless gland into the blood that is conveyed to other parts of the body and exerts an effect upon its “target” tissues (37). In 1910, Jean de Meyer suggested that the pancreatic secretion that was lacking in the diabetic state should, when found, be called “insulin” to denote its origin from the “insulae” of Langerhans (38).
Between 1895 and 1921, experimental work developed in two directions. One was the careful histologic study of the islets, which led to the finding of several distinct cell types, thus foreshadowing our present knowledge that the islets of Langerhans are the site of production and secretion of several hormones in addition to insulin. Of note was the description of hyalinization in islets of people with diabetes by E. L. Opie in 1900 (39). This hyalinization has since been shown to be the amyloid commonly found in the islets of people with type 2 diabetes, but this observation again linked the islets of Langerhans with diabetes. The other was a search for insulin itself. The requirements for insulin as a potential therapeutic agent were stringent: (a) the preparation had to be of consistent potency; (b) it should reverse the metabolic abnormalities of the depancreatized animal; (c) it should reverse the signs, symptoms, and chemical abnormalities of human diabetes; and (d) it should produce no harmful side effects.
The difficulties in the early attempts to isolate insulin were legion. There was total ignorance of the chemical nature of the postulated antidiabetic substance, making the extraction procedure a hit-or-miss proposition. At that time, quantitative estimates of the blood sugar required inordinate amounts of blood and the procedure was not generally available. Because of ignorance about the profound effects of low blood sugar levels on the nervous system (hypoglycemic convulsions), they were also not recognized as such and were initially attributed to a “toxic” action of the extract. In addition, fever and infections were frequent sequelae of the injections of extracts. In view of the protein nature of the hormone (which, of course, was not yet known), it is obvious that those workers who used oral administration of the extract were bound to fail. Of the many forerunners of Banting and Best, those who came closest to the mark were E. L. Scott, Israel Kleiner, Ludwig Zuelzer, and Nicolas Paulesco, as has been well described by Bliss (40). Indeed, Paulesco, a distinguished Romanian physiologist, produced a pancreatic extract that fulfilled all the criteria for “insulin” in animal experimentation but did not succeed in showing its application in human diabetes (41). Thus, the significance of his contribution was appreciated only much later.
Frederick Banting, a young surgeon; John Macleod, a professor of physiology; Charles Best, a graduate student; and J. B. Collip, a skilled chemist, succeeded during the years 1921 and 1922 in fulfilling all of the criteria for a therapeutically active insulin and produced the first useful and consistently successful insulin preparation for the treatment of human diabetes. Thus, the pancreatic etiology of diabetes was finally established (42).
The Nobel Prize for the Discovery of Insulin
The awarding of the Nobel Prize in Medicine in October 1923, 18 months after the first news of the discovery of insulin, was part of a gripping tale of success, disappointment, and conflict. The story of Banting, Best, Collip, and Macleod brought to light the tensions of a 6-month period that began in the summer of 1921 and intensified when the new extract corrected the metabolic acidosis in the first person to receive the substance in January 1922 (Leonard Thompson, age 14 years, at the Toronto General Hospital in Canada).
The drama started when Frederick Banting, a World War I veteran surgeon who was barely employed, was asked to be an instructor in physiology at the University of Western Ontario in Canada and became inspired by reading an article in the fall of 1920 by the pathologist Moses Barron. The article was entitled“ The Relation of Islets of Langerhans to Diabetes with Special Reference to Cases of Pancreatic Lithiasis” (43). Armed with this information, the 29-year-old Banting persuaded Professor Macleod of the University of Toronto to provide him the space and equipment to attempt to extract a pancreatic hormone from dog pancreases. Banting’s original idea was to extract the
substance, or “ferment,” from the dog pancreas after ligating the pancreatic ducts, but this failed. They were successful only with the total extraction of the pancreas from numerous laboratory dogs followed by injection of the resultant crude extract to demonstrate partial correction of the elevated blood sugar level in depancreatectomized dogs. Alone, except for one graduate student (Best), during the first 3 months of the project, because Macleod was in Europe, starting in August 1921, Banting and Best demonstrated a significant lowering of the elevated glucose level in depancreatectomized dogs with their dog pancreas extract.
substance, or “ferment,” from the dog pancreas after ligating the pancreatic ducts, but this failed. They were successful only with the total extraction of the pancreas from numerous laboratory dogs followed by injection of the resultant crude extract to demonstrate partial correction of the elevated blood sugar level in depancreatectomized dogs. Alone, except for one graduate student (Best), during the first 3 months of the project, because Macleod was in Europe, starting in August 1921, Banting and Best demonstrated a significant lowering of the elevated glucose level in depancreatectomized dogs with their dog pancreas extract.
By November, Macleod felt that biochemical expertise was critical for further refinement of the “hormone,” then given the name isletin by the young investigators. The following month James Collip, a young professor of biochemistry on a sabbatical leave in Macleod’s department, joined the three researchers. Despite Collip’s ability in January to prepare an effective extract for the first human recipient, Leonard Thompson, the success did not last. By the spring of 1922, both Banting and Best, as well as Collip, found it impossible to reproduce useful material. The prospects for the production of insulin brightened with the help of a brilliant strategist, George Clowes, the research director at the then small company called Eli Lilly, who developed a favorable contract with the trustees of the University of Toronto to work out conditions for large-scale production (40). Clowes fortunately had employed a rare talent at that time in the person of a chemical engineer by the name of George Walden, who made the critical observation in the fall of 1922 that maintenance of the isoelectric point of insulin afforded a maximum extraction of insulin from beef and pork pancreases (44). This paved the way for production of enough insulin to meet the needs of desperate patients and physicians worldwide.
Apart from the objective merits of the work and the investigators who produced it, the complexity of the Nobel Committee’s assignment of merit to only Banting and Macleod requires comment. In 1951 the Nobel Foundation published a historical commentary on its work, which contained information about the selection process in 1923 (45). Banting and Macleod, but not Best, were nominated, an essential requirement for Nobel laureate consideration. Furthermore, the Nobel report admitted that the committee reviewed only three pres-entations reporting on the insulin discovery. These articles did not include the first Banting and Best article of February 1922 (42), but they did review the seven-authored May 1922 article published in the Transactions of the Association of American Physicians (46). From their vantage point of the mid-20th century, the Nobel report concluded that Collip and Best had probably been assumed to be assistants and therefore not prime candidates for recognition (45).
The historian Michael Bliss, after all the principal parties in the case had died, was able to search anew, mainly in the archives at the University of Toronto, and concluded that all four of the investigators were essential to the discovery and could share in what a sage of the early 1920s had remarked was “glory enough for all” (40). Likewise, the scholar investigator Rachmiel Levine gave a good degree of closure on this matter when he commented in the 1993 version of this chapter:
As such things commonly proceed [the discovery of insulin in 1921], there was a tendency to overdo the interpretation. First, all diabetes was ascribed to insulin deficiency. The role of other hormones in metabolic control and an awareness of the bewildering heterogeneity of the diabetic syndrome belong to the half century and more that has elapsed since that momentous summer in Toronto in 1921. In 1922 Banting and Macleod received a Nobel Prize for this historic discovery. There was immediate controversy about the omission of Best and Collip from the prize—a controversy that has continued to the present day. Recent historical research into the details of the Banting and Best collaboration confirm that J. J. R. Macleod, Professor of Physiology at the University of Toronto, facilitated as much as he could the research suggested by Banting and was probably an appropriate co-recipient of the Nobel Prize [(44)]. It has always been clear that, of the participants, Macleod was certainly the most knowledgeable in the fields of carbohydrate metabolism and diabetes mellitus. The success of the work by Banting and Best was due to Macleod’s basic knowledge, Banting’s stubborn persistence, and the important specific skills of Best and Collip [(47)].
THE INSULIN ERA
The Years 1922 to 1960
During the period from the discovery of insulin through the 1950s, the effects of the availability of insulin were felt in three notable ways: an improved life expectancy for patients with type 1 diabetes, a surge of interest in understanding the mechanism of action of insulin on intermediary metabolism, and an increasing recognition of the syndromes we have come to appreciate as the chronic complications of diabetes. A combination of factors promoted a longer life span for the beleaguered patient with the disease, beginning with the near elimination of death from diabetic coma that coincided with improved means of treating the complications of diabetes. Hormonal regulation of glucose metabolism was clarified, with progress made in understanding the role of hepatic, adipose, and muscle tissues in the uncontrolled diabetic state. Success in defining the entire endocrine network, especially in demonstrating the importance of the pituitary-adrenal axis, gave the field of endocrinology a specialty status.
The Insulin Timetable
The discovery of insulin changed forever the treatment of diabetes; these and related developments are outlined in Table 1.1 (48).
TABLE 1.1. Insulin Timetable: 1921 through the Present | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
The arrival of an adequate supply of commercial insulin for patients from 1923 onward was followed by the development of procedures for purifying and standardizing insulin. By 1926 crystalline insulin in concentrations of 10, 20, and 40 units per milliliter became available worldwide. The task of purifying insulin continued for decades, starting with early efforts to avoid contaminants such as glucagon. Starting in 1936 protamine and zinc were used to prolong the action of insulin (49). In the 1970s, self-monitoring of blood glucose became a standard of care. Further changes were made possible with the tools of mo-lecular biology, which allowed the production of human insulin and analogues that change absorption characteristics. These insulin variations, coupled with the arrival of finer, less painful, needles, facilitated multi-injection programs that provide better glucose control. Pump delivery systems also became available. It is difficult for those involved with diabetes today to comprehend fully the changes that have taken place since the introduction of insulin. The first Joslin patient to receive insulin was Elizabeth Mudge, R.N., who was first treated on August 7, 1922, at the New England Deaconess Hospital in Boston. She had not been able to leave her apartment for 9 months, but after 6 weeks of insulin therapy, she could walk 4 miles daily, and she lived for 25 more years. Regarding the preinsulin days, Dr. Joslin noted, “I used to count the days my diabetic children lived” (50). This is emphasized by an episode that took place in the crowded original offices of the Joslin Clinic
on Bay State Road in the 1940s, when a child patient became more than a bit noisy. Dr. Joslin came by and said, “Make all the noise you want. We love noisy children around here. For many years there were no normal children. They were very quiet and after a visit or two they did not return” (L. P. Krall, personal communication).
on Bay State Road in the 1940s, when a child patient became more than a bit noisy. Dr. Joslin came by and said, “Make all the noise you want. We love noisy children around here. For many years there were no normal children. They were very quiet and after a visit or two they did not return” (L. P. Krall, personal communication).
Prior to the use of insulin, most young patients with diabetes died shortly after diagnosis. The Joslin Clinic experience (51) showed the commonest cause of death to be ketoacidosis (63.8% until 1914 and 41.5% until August 1921). The improvement from 1914 to 1921 was probably due to the introduction of Frederick Allen’s “semistarvation” therapy in about 1915. Even though patients with type 1 diabetes could sometimes survive for years using this form of starvation therapy, most died sooner. By comparison, in affluent countries, the rate of death due to coma is now a rare event, although in some developing countries, death rates still approach preinsulin levels.
When Joslin wrote the preface to his third edition of The Treatment of Diabetes Mellitus late in 1923, the experience he drew upon was based on 3,000 cases and his use of insulin had been extended to 1 year (52). He wrote: “Compared to the last decade, the doctor now has twice as many diabetics to treat…. Of the 48 children cared for in this period, 46 remain alive… and as for Bouchardat, Cantani, Kulz, Lepine and all the other diabetic saints, how they would have enjoyed this year!”
The Study of Diabetes and the Development of Clinical Care
The original physicians on the first Insulin Committee of the University of Toronto in 1922 were Elliott P. Joslin of Boston; Robert Williams of Rochester, New York; Frederick Allen of Morristown, New Jersey; Rollin Woodyatt of Chicago, Illinois; Russell Wilder of the Mayo Clinic, Rochester, Minnesota; and Richard Geyelin, of New York City (53). These men, each in his own way, were leaders in the new treatment of diabetes in the first decade after the discovery of insulin. They were the first physicians to report on the detailed management of children and adults presenting in metabolic acidosis. With time, new clinical problems emerged in the medical literature as the first decade of insulin use ensured longer-living patients. By the early 1930s, the occurrence of lower extremity neuritis was becoming more common, as was the number of persons with a combination of Bright’s disease (nephrotic syndrome) and hypertension. In 1928 Joslin described neuritis on one page of his 500-page fourth edition (54), but by his eighth edition (1946) the subject had been expanded to an entire chapter (55). By World War II the goals were clear: first, prevent death from diabetic coma; and second, train patients to help decrease the appearance and impact of diabetic complications.
Diabetic Manuals and Early Diabetes Education
Most of the leading physicians of the 1920s and 1930s who were interested in diabetes produced instructional guidebooks that covered the use of insulin, care of equipment, and management approaches to hyperglycemia and hypoglycemia. However, the majority of these instructional renditions went through only one edition, with the notable exceptions of the guidebooks of R. D. Lawrence of London and Joslin, which were revised approximately every 4 years. Lawrence titled his book appropriately The Diabetic Life, which set a publication record, reaching 17 editions by 1965 (56).
Joslin began to publish his first manuals shortly after the first edition of his diabetes textbook in 1916 (1), and by his third edition in 1923 (52), he had quickly adapted the contents to the arrival of insulin while maintaining the length of the manual to fewer than 200 pages. This practical “reader” for patients reached more people with diabetes in America than any other guide in the immediate decades following the introduction of insulin. The early editions were subtitled For Mutual Use of Doctor and Patient, as the practitioner absorbed, along with the patient, the details of the new treatment (57). Each table of contents boldly proclaimed the value of self-care in matters as far reaching as prevention of gangrene and constipation and proper dental care. He maintained that steady care of oneself, with proper treatment defined as a combination of more than one adjustable daily insulin dose (as a rule) and dietary restrictions along with regular, planned exercise, favored a longer life. His life-expectancy predictions for people with diabetes underlined the value of his advice by showing a steady improvement in longevity.
Joslin was a highly organized person who not only was interested in his patients’ health but also found time to inquire into the details of their lives. From the first use of “diet therapy,” he recognized the value of hospitalization in a hospital “cottage” or “schoolroom” setting that was dedicated to patient treatment through education. These cottages later evolved into an ambulatory inpatient ward he termed the Diabetes Treatment Unit. Patients were expected, while under supervision in this ambulatory setting, to enter into a team approach with doctor and educator in choice of insulin doses according to exigencies of the particular day’s program. However, in recent years, cost-containment restraints on medical insurance have moved diabetes education to outpatient venues.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree