The Histologic Biopsy of Thyroid—Technical Aspects
Historically, the use of incisional biopsies and more recently the use of core needle biopsies had been advocated by some who felt that the preservation of tissue architecture was important in the evaluation of thyroid lesions. However, both incisional and core biopsy suffer from some significant drawbacks that lead us to recommend fine needle aspiration (FNA) in most instances with histologic sampling reserved for limited applications.
Currently, incisional biopsy is infrequently employed and for obvious reasons. Incisional biopsy is an open procedure with greater consumption of health care resources. Incisional biopsy also requires entry into the same compartment that may have to be reentered for definitive surgery, potentially complicating the later procedure. Needless to say the patient is left with a scar in addition to the loss of the time required for the procedure.
Needle core biopsy overcomes some of these limitations. Core biopsy is done as an outpatient, thereby reducing health care resource consumption and is less invasive into the anterior compartment of neck than an incisional biopsy. However, needle core biopsy carries substantially greater risks than FNA and in particular the risk of hemorrhage and significant hematoma [1, 2, 3, 4, 5].
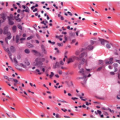
Both incisional biopsy and needle core biopsy are traumatic to a lesion that has been sampled and may disrupt, scar, or even infarct the lesion. This may also occur with FNA, but as FNA typically employs a smaller gauge needle, the frequency and severity of lesional injury is reduced. In most cases, lesional injury is not of major significance, but if a follicular lesion is diagnosed and requires careful evaluation of the capsule to determine malignancy, previous sampling procedures can compromise the correct interpretation of the histologic diagnosis on a subsequent surgical specimen [6].
Some tout the potential need for ancillary studies as necessitating a histologic sample. It should be remembered that any ancillary technique applicable to a histologic specimen can be applied to FNA specimen. For example, if immunoperoxidase staining is required, a formalin-fixed cell block preparation from a good FNA needle rinse can provide numerous fragments for interpretation.
With regard to diagnostic accuracy, studies to date have not been able to document any consistent superiority of either FNA or core needle biopsy [2, 3, 7, 8]. Some studies have shown that the use of both is advantageous [9], and others report higher diagnostic yields from core biopsies [10]. Admittedly, the attempts to study this question have been flawed and due to inherent pathologist biases favoring certain specimen types for interpretation, so it is difficult to establish that one technique is truly superior to the other. At best, the studies suggest that both FNA and core biopsy result achieve similar diagnostic accuracy in the majority of cases. In a small minority of patients, one sampling technique will establish a diagnosis where the other will fail (FNA success while core biopsy nondiagnostic or alternatively core biopsy diagnostic with a nondiagnostic FNA); however, this cannot be prospectively predicted in a given patient. It should be pointed out that the studies have suggested a reduction in inadequate samples when needle core biopsy is engaged [2, 8, 9, 10, 11]. It also goes without saying that the greatest diagnostic accuracy is achieved when an expert histopathologist interprets the histology, and similarly, the best results are achieved when the FNA is interpreted by an expert cytopathologist. Thus, the choice of core needle biopsy or FNA is occasionally determined by the preference of the individual collecting the sample but more frequently is determined by the preference of the pathologist who interprets the sample either explicitly or implicitly.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree