- Diabetes results in a range of distressing symptoms, altered daily functioning (requiring attentive monitoring and treatments), changed family roles, higher costs, lost productivity and premature mortality, which are felt by households, communities, and national economies.
- Diabetes is the fifth leading cause of death in the world (4 million deaths annually), outnumbering global deaths from HIV/AIDS; 80% of this mortality occurs in low and middle income countries, disproportionately affecting the young and economically active populations.
- Cost appraisal methods require epidemiologic, clinical, and economic data, and utilize different approaches to calculate the direct medical costs (of treatment, diagnosis, monitoring), indirect costs (of lost outputs from disability and premature death) and intangible losses (psychosocial burdens) attributable to diabetes.
- Even though there are large variations in methods of cost appraisal, cost items incorporated and purchasing power, as well as accessibility to and patterns of clinical care resulting in widely varied between-country per capita expenditures, it is clear that the presence of diabetes results in excess consumption of resources worldwide.
- Progressive severity of disease complications, co-morbidities and complexity of therapy all increase the monetary, infrastructural and human resource costs of care.
- Individuals in vulnerable subpopulations are at an elevated risk of developing diabetes and progression toward significantly harmful outcomes, and devote a large proportion of resources toward their therapies and diabetes care; confronting the increased susceptibility and burdens will require addressing the underlying political, socioeconomic and behavioral factors that perpetuate disparities.
Introduction
Diabetes has emerged as a major health problem worldwide, with serious health-related and socioeconomic impacts on individuals and populations alike. Furthermore, the pandemic growth of diabetes is being spurred on by transitioning demographic (e.g. population aging), socioeconomic, migratory, nutritional and lifestyle patterns, and an affiliated proliferation in overweight and obese adults and children [1–2]. The International Diabetes Federation estimates there are 285 million people with diabetes worldwide in 2010 [3], and projects the absolute number will surpass 400 million in the coming twenty years. The overwhelming majority of this escalation will be attributable to growth of type 2 diabetes (T2DM). Rapid socioeconomic transformations seen with globalization, increasing urbanization, industrialization and marketization of developing regions will also result in a parallel growth of diabetes precursors (impaired fasting glucose [IFG] and impaired glucose tolerance [IGT]) and ensuing health consequences [4–6].
Current estimates suggest that two-thirds of those affected by diabetes live in low and middle income countries (LMIC). This challenges traditional paradigms that segregated chronic non-communicable diseases (NCDs) as problems of affluent countries alone. Eight out of the top 10 countries with the highest absolute numbers of people with diabetes are developing or transitioning economy countries [3]. While this burden of greater absolute numbers may be partially explained by larger population size, the rates at which NCDs are increasing in these countries amid transition are much steeper when compared with those in more developed affluent countries [7]; by 2025, the number of diabetes cases will increase by 170% in low and middle income countries, compared to a 41% increase in developed countries [8].
Thus far, the attention on health burdens in the developing world has focused justifiably on the persistence of infectious diseases and nutritional deficiencies; however, these same countries must also contend with 80% of global mortality associated with chronic diseases [9,10]. Projections suggest that this already overwhelming “double burden” will be exacerbated by the growth of NCDs. Altogether, projected increases in diabetes in all corners of the globe will result in corresponding escalation of burdens in the form of serious morbidity, disability, diminished life expectancy, reduced quality of life, loss of human and social capital, as well as individual and national income losses. This chapter describes these burdens in a global context, and systematically introduces data regarding regional patterns and associated themes.
Distribution and trends
Epidemiologic evidence quantifies the impacts and predictors of disease, identifies vulnerable populations and their needs, and facilitates formulation of appropriate disease prevention and control strategies; however, there are still limited representative epidemiologic data originating from a great many LMICs. Moreover, the utility of currently available estimates is hampered by methodological deficiencies (inconsistent diagnostic criteria, poor standardization of methods) and limited coverage (regional sampling with a predominance of urban studies whereas the vast majority of the populations in question are rural inhabitants). Despite this, notable patterns can be discerned and can be described by giving examples from regions where they are particularly noteworthy.
In Africa, there is:
- A general lack of awareness about chronic diseases and their risk factors.
- Limited data originating from a few localized centers in certain regions (western, eastern and southern) of the continent. The latest data (1998–2004) show prevalence rates of 1–3% in rural areas and 6–10% in urban environments [11].
- A growing double burden of communicable diseases and nutritional deficiencies, along with NCDs, especially where there is rapid economic development and globalization. Between-country differences in NCD prevalence likely reflect different stages of socioeconomic and epidemiologic transitions [12].
- A tendency for cultural (perceptions of excess weight and imported processed foods as symbols of status and luxury) and societal (stigmas regarding loss of weight as a sign of HIV infection) factors to influence health-seeking behavior [11,13].
- Variation in risk by ethnicity, with Black Africans showing a greater preponderance toward hypertension, while those of Egyptian and Asian Indian origin demonstrate higher prevalence of diabetes [14].
In Europe, the USA and Canada:
- Available data are derived from population studies, records of insulin and antidiabetic medication sales and/or reimbursement claims. Estimates still suggest 30–50% of people in these high income countries (HIC) have undiagnosed diabetes [4].
- Annual incidence of type 1 diabetes (T1DM) is increasing in Europe (+3.2% per year) and North America (+5.3% per year); the highest reported incidence rate is in Finland (40.9/100,000 per year) [15,16].
- Prevalence of T2DM is highest and growing fastest in vulnerable subgroups such as lower socioeconomic groups and the elderly [4].
- Life expectancy of people with diabetes, although reduced when compared with the general population, is markedly higher than in developing regions of the world. This is largely attributable to differences in access to self blood glucose monitoring and therapies to control glycemia.
- Uptake and costs related to newer and more expensive investigations and therapies are associated with inflated national health expenditures.
In Latin America:
- There is wide variation in prevalence rates (1.2–8%) of diabetes, reflecting the diversity of ethnicities and stage of development between countries.
- The pattern of T1DM incidence seems to correspond to the size of the population of Caucasoid origin.
- Diagnosis of diabetes frequently occurs late in the course of disease. Thus, complications may be present in 30–40% of cases at time of presentation for health care.
- Poor accessibility to health services results in only 30–40% of cases actually receiving therapy [17].
Asia is emerging as the epicenter of the cardiometabolic pandemic, because:
- Populous countries in this region are confronted with diabetes risk being manifest at younger ages and at lower body mass indices compared with populations in other regions.
- Patterns of genetic and/or ethnic propensity; South Asians and peninsular Arabs have markedly elevated metabolic risk [18]; Japanese are reported to have the highest prevalence of genetic polymorphisms [19]. Rural–urban differences in prevalence together suggest both gene–environment interactions and influences of the “thrifty” genotype.
- Estimates suggest a three- to fivefold increase in prevalence of T2DM over the last three decades, and an increasing prevalence of T2DM in children, with major implications for future burden in this region [20,21].
- India is estimated to have 50.8 million people living with diabetes [3], the highest absolute number in any country [22] and projections suggest that one-fifth of all people with T2DM will be living in the Indian subcontinent by 2030 [23].
- The “Asian Indian phenotype” is characterized by a preponderance to deposition of metabolically active visceral adiposity which may explain the greater vulnerability to diabetes in this population [24–26], while Western Pacific Islanders also demonstrate a markedly elevated risk.
Diabetes is renowned as a “silent epidemic” [22]. The slow progression and lack of symptoms in the early stages of disease preclude seeking medical attention and preventative care. As such, reported prevalence reflects an underestimate of the number of cases because it does not account for undiagnosed cases. Population studies estimate that 30–50% of diabetes cases are as yet unrecognized, even in the most advanced countries [4,17]. Also, almost half of all newly diagnosed cases will have already developed diabetes-related complications in the form of nerve, eye, kidney, and/or vascular diseases [23,27,28]. Target organ damage of this nature can be life-threatening and/or seriously disabling [29].
The traditional socioeconomic gradient associated with chronic diseases may itself be transitioning. As the world’s urban population size begins to outnumber those living in rural areas, many developing economies face enormous challenges related to the growth of peri-urban slums and squatter settlements, the disparities in provision of basic amenities and lack of adequate sanitation and nourishment. Further challenges include subsequent exposure to contemporary dietary choices, tobacco use and mechanization of transport with consequent growth in the incidence of NCDs. Thus, the paradigm is shifting globally towards the inverse relationship found in established market economies where the greatest burdens of NCDs are felt by the least well-off segments of the population [30–35]. In India for example, Ramachandran et al. [36] demonstrated that although family history and prevalence of glycemic abnormalities in high-income groups were double those of low-income groups, the reverse was true for smoking, alcohol consumption, prevalence of co-morbid cardiovascular risks and occurrence of complications (macrovascular disease, cataracts, proteinuria and neuropathy). Recent prevalence and trend data show greater disease susceptibility in lower socioeconomic groups in India [37,38], mimicking patterns in wealthier nations [39–42]. As this chapter progresses, it will become evident that the countries with the greatest burdens of disease are also those least equipped to manage the growing epidemics.
Major burdens
The burden of any disease, including diabetes, can be described by its health-related impacts: the morbidity and mortality caused, and the social and economic costs to individuals, families, communities and national economies (Box 5.1). Evaluation of resources utilized or lost, be they human, social, monetary or infrastructural, and placing objective “values” on them may be inherently partial to the perspective taken. The term “value” may be used to describe the measured and/or perceived net worth of resources consumed or lost because of illness and/or infirmity which is the mode used in this chapter. Economists use this term to express the net benefit derived from an investment in health care in proportion to the amount of resources used [43].
Acute and chronic disease complications
The patterns of major health-related burdens of diabetes vary by the type of disease. T2DM accounts for 90–95% of all cases worldwide. Both T1DM and T2DM, the two most common forms, may be associated with acute and chronic metabolic consequences, but the frequency of events varies according to the underlying pathophysiology and level of glycemic control.
Acute fluctuations in serum glucose may rapidly spiral into emergency situations, with potentially fatal repercussions if untreated. Episodes of severe acute hyperglycemia (e.g. diabetic ketoacidosis [DKA] and hyperosmolar hyperglycemic syndrome) or, conversely, severe hypoglycemia, most often require immediate medical management. Longer term follow-up is then intended to promote better blood glucose regulation and avoidance of precipitants of diabetic emergencies (e.g. infection, noncompliance with treatments, missing meals, alcohol abuse). Apart from atypical variants such as ketosis-prone T2DM in African subjects [11], the vast majority of acute complications occur in patients with T1DM, while approximately 10–12% occur in subjects with T2DM. When treated properly, the mortality from acute hyperglycemic episodes such as DKA is extremely low (e.g. DKA mortality in Taiwan, USA and Denmark were estimated to occur in 0.67–4.0% of cases) [44,45]. In contrast, in some African countries, mortality from DKA can be as high as 25–33% [46], although the incidence of these complications from LMIC settings is limited [47]. Individual patient (e.g. age, additional co-morbidities) and resource (e.g. hospital facilities, experience of staff) characteristics may also modify the outcomes. In underresourced settings for example, complex, cumulative and interconnected barriers (poor accessibility, inadequate therapeutic instruments and medication, and insufficient numbers of trained staff) result in poor glycemic control and higher risk of mortality [48]. As such, early life mortality in patients with T1DM in low-resource settings is commonplace. The post-diagnosis life expectancy in some regions of Africa is just 1 year [49].
- Health seeking and utilization (frequency and costs)
- Disease events and/or ill health
- Morbidity (physical and psychosocial)
- Mortality
- Disability
- Alteration of social roles or family structure
- Caregiver or “intangible” burdens
- Direct medical expenditure
- Ancillary expenses of health seeking and care
- Indirect costs (losses in productivity)
Apart from glucose dysregulation, both T1DM and T2DM are associated with damaging effects on tissues, with eventual progression to devastating complications. Diabetes increases the risk of macrovascular diseases (cardiovascular diseases [CVD], which comprise coronary heart disease and cerebrovascular disease or “stroke,” and peripheral vascular disease [PVD]), microvascular diseases (retinopathy and nephropathy), neuropathies, and the consequences that stem from these (e.g. congestive heart failure, diabetic foot). These complications are associated with considerable morbidity, reduced quality of life, disability, premature mortality and high economic costs.
In addition, T2DM is associated with the “metabolic syndrome,” a collection of cardiovascular risk factors (abdominal obesity, hyperinsulinemia, hypertension, dyslipidemia, proinflammatory and procoagulant states). It is believed that these biochemical and inflammatory derangements are intimately linked, possibly by a central mediating factor. In Latin America, it is estimated that 53–69% of people with diabetes have abnormal serum lipid subfractions, and 34–67% have hypertension [17]. As such, these factors increase the likelihood of developing additional risks, and with each added risk, predispose one to an exponentially increasing risk of atherosclerotic vascular disease events and mortality [50].
Moreover, T2DM has a distinctive association with coronary heart disease (CHD). Those with diabetes have a two-to fourfold higher risk of developing CHD than people without diabetes [51]. More significantly, however, the age- and sex-adjusted cardiovascular mortality risk in patients with diabetes is equivalent to that of individuals without diabetes who have had a previous myocardial infarction (MI) [50,52,53]. Precursors common to both T2DM and CVD (insulin resistance, visceral adiposity and excess inflammation) [54–58], and a complex mix of mechanistic processes such as oxidative stress, enhanced atherogenecity of cholesterol particles, abnormal vascular reactivity, augmented hemostatic activation and renal dysfunction, cumulatively confer this elevated risk of CHD [59]. As such, simply controlling glucose has not been found to reduce CVD events and mortality in large randomized controlled trials at least in the short term [60–62]. The implications therefore are that individualized comprehensive multifactorial risk management, involving the treatment of all co-morbidities, has been advocated for people with T2DM [63,64], adding to the burdens placed on patients, providers and health systems.
Diabetes also increases the risk of renal dysfunction. In Africa, it is estimated that within 5–10 years following diagnosis, 32–57% of people with diabetes will have developed microalbuminuria [48,65]. Also, diabetes is the primary cause in approximately 45% of patients with end-stage renal disease (ESRD) requiring dialysis or transplantation in the USA [66,67]. Meanwhile, approximately one in four persons with diabetes have some visual impairment, and 5% of all cases of blindness globally are caused by diabetes [68]. Particularly in the case of retinopathy and nephropathy, duration of disease, age, glycemic control and blood pressure control have all been found to be prominent modifying factors of disease onset, progression and outcomes.
Neuropathies are also common consequences of diabetes. One-third of Sri Lankan people with diabetes surveyed had lower extremity sensory loss putting them at risk of ulceration [69], while a similar proportion of people with diabetes in African countries were found to have either neuropathy or compromised peripheral vascular circulation [70,71]. The combination of neuropathy, increased susceptibility to infection, poor wound healing and poor distal circulation increases the risk of lower extremity amputation 15- to 40-fold [67,72].
The most significant repercussion of the asymptomatic early natural history of the diabetes and low community awareness is that subclinical disease results in progressive tissue injury. Microvascular and macrovascular complications cause morbidity, greater health-seeking and increased mortality risk in all regions of the world [23,27,73].
Health utilization patterns
Health seeking and health utilization behaviors are influenced by a number of individual, provider and system level factors. In the case of diabetes, ill health and morbidity as well as preventative care motives result in incrementally more health service utilization. In Costa Rica, for example, people with diabetes made 55% more medical visits than those without diabetes, and German patients with diabetes averaged 31 yearly consultations with general practitioners (GPs) and/or specialists [74,75]. In Sweden and Italy, approximately half of diabetes-related consultations were at hospital outpatient departments or dedicated diabetes centers, respectively, and the remainder were with GPs [76,77]. In Latin America, diabetes accounts for an estimated 35 million medical visits annually [74].
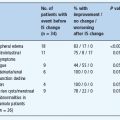
Various studies have shown that having diabetes doubles one’s risk of hospitalization compared to not having diabetes, and this risk is amplified by the development of diabetes-related complications. The presence of poor peripheral circulation increases the risk of hospitalization by 70%, while CVD increases this risk by 310% [67]. The Cost of Diabetes in Europe Type II Study (CODE-2) reported 13% of people with T2DM were hospitalized (with an average stay of 23 days) over the 6-month study follow-up, while Germany’s Cost of Diabetes Mellitus (CoDiM) study reported that 28.8% of people with diabetes had at least one hospital admission in 2001 [75]. Although studies from most regions of the world report late-stage macrovascular or microvascular complications as the leading cause of diabetes-related hospitalizations, lower income settings such as Ethiopia confront a greater proportion (almost two-thirds) of admissions in the form of acute episodes of dysglycemia.
Health care infrastructure and financing have strong impacts on health seeking and utilization. In India, estimates suggest that 85–95% of all health care costs are borne by individuals and their families from household income [78–81]. In Latin America, 4060% of diabetes expenses are derived from out-of-pocket payments. A survey in Jamaica showed that 57% of the sample reported financial difficulties as a result of illness, and of these, half disclosed that they had avoided therapy because of economic constraints [74]. Financial limitations to accessing treatment are not confined to LMICs, as illustrated by 19% of elderly Americans revealing curtailed purchases of diabetes medications as a result of costs [82,83].
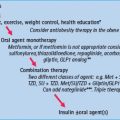
When one considers that the average number of medications used by people with diabetes in India is 3.5 [79], the cost implications are substantial. These drugs include antihypertensives, lipid-lowering, antidepressant medications and aspirin in addition to glucose-lowering drugs). The use of oral hypoglycemics increases health expenditure by 40% compared to the general population, while regular insulin use is a further twofold greater expense. As such, data from Germany show that use of insulin with or without oral agents increases total costs 3.1–3.4 times [75,84].
Increased health seeking and utilization in people with diabetes and associated complications result in greater medical costs incurred, compared to the general non-diabetic population.
Disability
Aside from the medical or biologic dysfunction caused by disease, there are implications of ill health for individual and interactive functioning in society. This concept of “disability” is distinctive from simple biomedical models of disease and signifies that psychosocial illness or physical deviations from generally accepted norms of anatomical structure or physiologic function may impair one’s ability to perform domestic and occupational activities, and assume societal roles. As a result, diabetes may inhibit one’s general utility and ability to integrate fully in society.
Diabetes can lead to disability through a variety of ways. Excluding the medical aspects of diabetes-related complications that directly restrict bodily function, diabetes may be considered a “hidden” disability, whereby the individual concerned is hampered from routine activities, but displays no physical manifestation of this illness. For example, children with diabetes may be unable to participate in all activities their contemporaries are engaged in and may suffer wrongful discrimination. Adults in the workplace may have lower work performance by virtue of any number of symptoms (impaired fine motor skills and concentration, grogginess, urinary frequency) [85] or even decline in cognitive functioning [86–88]. Those requiring insulin may be limited additionally by highly structured activities of daily living (the requirement of meticulous glucose monitoring, insulin administration, timed eating), recurrent hospitalizations, hyperglycemic and hypoglycemic episodes, and by regular preventative or therapeutic medical visits.
Indeed, the physical manifestations of diabetes become more significant with the development of complications. As such, visual impairment, restricted mobility (from shortness of breath, chest pain or even amputation) and general ill health (ranging from increased susceptibility to infection all the way to uremia related to irreversible renal dysfunction) are all considerable impediments to productive work and engagement in socially valuable activity. Cross-sectional studies in the USA have demonstrated that elevated glycated haemoglobin (HbA1c) is associated with a higher likelihood of missing work, greater hours absent [89] and reduced at-work efficiency [85].
Depending on the health status of the individual and severity of disease, disability can be temporary or permanent. There is limited country-specific data on the permanent disability resulting from diabetes, although diabetes is the leading cause of adult-onset blindness, non-traumatic amputations and irreversible kidney failure worldwide [22]. Data from Chile showed that 8% of people with diabetes had some form of permanent disability [74].
Less tangible, but no less severe, are the psychosocial burdens that may accompany diabetes and affect functioning [90,91]. In a health maintenance organization cohort of 1642 people with diabetes, 12% were unemployed, 7% of those employed had missed more than 5 working days in the previous month and 4% of employed subjects reported difficulties with completing work tasks. Of those with any form of work disability inducing absence and/or poor productivity, over half had minor and/or major signs and symptoms of depression [92].
The complexity of disability as a limitation of individual and societal function is in quantifying this shortcoming. There are several methods that have been used which factor in age, education and occupation, but most have at least some imperfection because of the necessity of making judgments about the value of activities. This is especially difficult where there are cultural and ideological dissimilarities between the evaluator and the population being appraised.
Mortality
Ascertaining the global mortality attributable to diabetes is no easy task. Most mortality statistics rely on documented causes of death and do not acknowledge the roles of glucose dysregulation in underlying mortality associated with CVD and renal diseases. Danaei et al. [29] have therefore argued that evaluating actual diabetes-related mortality should take into account that diabetes contributes to 21% of CHD and 13% of stroke mortality worldwide. The World Health Organization (WHO) incorporated these sentiments into calculating that diabetes is the fifth leading cause of death worldwide in 2000 [93]. The International Diabetes Federation’s most recent Diabetes Atlas approximates that diabetes is responsible for 6.8% of total global mortality (4 million deaths) annually [22,94]. In addition, the mortality attributable to diabetes would be even higher if deaths related to IGT were also included. This diabetes precursor independently increases the risk of mortality, and has a prevalence of 15–40% in adults [6].
Altogether, diabetes is associated with premature mortality, shortening life expectancy by approximately 7–15 years [95,96]. In developed countries, CVDs account for an overwhelming 65–75% of deaths in people with diabetes [97,98]. In low-resource settings, infections and acute metabolic emergencies are still the prevailing causes of death in people with diabetes [11,12,65,99]. ESRD also carries inexorably high mortality, mainly because of inaccessibility (physical and financial) of treatment (dialysis and/or transplantation) in most LMICs [11]. As a result, globally, CVD and nephropathy are the most prominent fatal endpoints, and occurrence is analogous to duration of disease in that early life survival and long-standing diabetes increase susceptibility to succumbing from these illnesses [27].
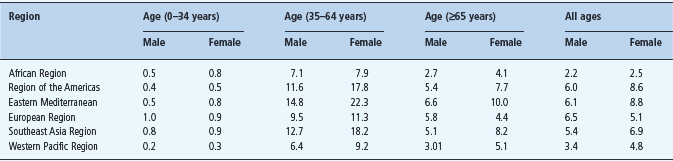
There is regional variation in the global distribution of diabetes-related mortality. Estimates for the percentages of deaths attributable to diabetes by region are shown in Table 5.1. Although the proportion of deaths in LMICs is lower than in more developed countries, the absolute numbers of deaths, by virtue of larger population size, outnumber those in economically developed countries. South Asia is currently reported to have the highest absolute number of diabetes-related deaths annually [100]. Also, there is a noticeably greater proportion of deaths in younger age groups in LMICs, resulting in higher loss of life years, and affecting the economically active subpopulations in these countries.
Table 5.1 Estimated percentage of deaths attributed to diabetes by age and World Health Organization (WHO) region. All fi gures are presented as male/female percentages. Adapted from Roglic et al. [93].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree