Fig. 34.1
Teledermatology actors
Primary (or patient-initiated or patient-supplied) TD encompasses communication between the patient and the GP or dermatologist. Primary TD has scarcely been researched thus far. Self-monitoring and patient empowerment are mentioned as important reasons for primary TD in acne or psoriasis patients [8–11]. Primary TD may be used to improve outpatient clinic triage for patients that the GP has already referred to the dermatologist for a face-to-face consultation [12].
In secondary TD, the GP or the homecare nurse communicates with the dermatologist. Secondary TD may be one of the most evolved telemedicine services so far, having been subject of research since 1995 [13, 14]. Research has shown secondary TD to be diagnostically accurate and reliable in many implementations [15, 16]. Recent studies showed that secondary TD is implemented in regular healthcare systems with reimbursement for the actors, is more efficient compared to conventional care, and is more cost-effective [17, 18].
Tertiary TD facilitates communication among dermatologists. Tertiary TD cases with a more specialized character are presented to get an expert opinion from a specialized (often academic) dermatologist; also tertiary TD often has an educational character [19].
Mode of Delivery
Two main technologies are used for the delivery of information and care in TD. The most common is store-and-forward (SAF), asynchronous data transfer in which photos and videos are created, sent, and assessed at the actors’ time of convenience independent of the actors’ location. Another less popular mode is real-time (RT), synchronous data transfer in which photos but more often video streams are created, sent, and assessed at a time all actors are available independent of the actors’ location. Lastly there is a hybrid mode where SAF and RT are used simultaneous.
Capturing Technology
Teledermatology has been made possible through the introduction of consumer digital (video) cameras. As store-and-forward is the main delivery mode of choice, video camera equipment is not discussed in this chapter [20]. In the late 1990s and early 2000s, the costs of digital camera equipment posed a barrier for the use of TD, and the quality of different cameras continued to be a critical topic of discussion. With the current hardware, these issues are off the table. Any off-the-shelf digital camera can produce an image of more than sufficient quality for TD. This day, the quality of the image is highly dependent, not on the camera but on the skills of the photographer. It is recommended, when practicing TD, to take an introductory course in taking (clinical) pictures.
High-quality dermoscopic images can be acquired when a dermoscope is attached to a digital camera. The assessment of dermoscopic images through TD is called teledermoscopy and is used for screening and management of skin cancer. Its advantages and risks are described in the next section.
The development of digital cameras in mobile phones brought a new capturing device to TD. Pilot studies show mobile phone TD to be feasible [21–25] and to contribute to mobility and self-management [8, 26]. Recently, mobile phone TD used as a skin cancer screening tool has shown promising results in a number of pilot studies [27–30].
Purpose
The most common purpose for TD is consultation: to get an advice from an expert on diagnosis, management, or both, with the underlying goal to avoid physical referral, or to obtain a second opinion.
Triage is the second use of TD and overlaps with consultation, as the result of a consultation improves a patient’s triage by either avoiding physical referral or accelerating referral. When used to prevent a referral, TD can reduce physical referrals up to 74 %. When a second opinion is obtained, 16% of these patients will have an accelerated physical referral, hence improving quality of care [18]. TD is also used as a triage tool in skin cancer screening [31, 32] and in outpatient clinic triage [12].
Monitoring, a third purpose of TD, is used for and by patients with chronic disorders such as psoriasis patients on systemic treatment and patients with open wounds. Pilot studies show that monitoring can optimize treatment, improve compliance, and improve empowerment of the patient’s responsibility [11, 33, 34]. Monitoring of patients with chronic wounds via TD can offer a better quality of life and gives potential to cost-effective long-term wound care [35, 36].
Teledermatology is also used in education programs. Online discussion groups and Internet fora are used as a stage to present interesting cases as continuing medical education for colleagues [19]. There are resident training programs developed that incorporate TD in their courses [37]. Lastly, there is a huge passive learning experience found in GPs practicing TD and gaining knowledge from the answers provided by the dermatologists [18].
Finally there is the purpose of cost reduction that has so far been subordinate to aforementioned purposes, as availability and quality of care are the first priority. Nevertheless, cost reduction is a very important motivator of all telemedicine implementations. Only after cost-effectiveness has been proven in TD, it can grow into a fully implemented practice of care delivery. Due to the many variables and different perspectives, it has proven difficult to design complete cost analysis in telemedicine [38]. Recent studies however indicate that teledermatology is cost-effective under the right conditions and can save healthcare costs up to 18 % [17, 18, 39].
Satisfaction and Acceptance
Although reliable validated methods to assess satisfaction of patients and referring and consulting clinicians do not yet exist in telemedicine research, there are still a number of publications with, be it mostly anecdotal, results on the subject.
Main positive results on patient satisfaction display high rates of acceptance, confidence, and favoritism of TD (76–93 %) [40–45]. Concerns with TD were mainly expressed as “not seeing a dermatologist in-person” but were post by a lower percentage of the population (30–40 %) [40, 41, 45].
Clinicians are generally satisfied with TD and acceptance is high, but express concerns on time consumption and complex or faulty software [40, 43, 46]. As one would expect, most clinicians who are using teledermatology are front-runners who embrace innovative techniques and tend to be more positive. Indeed, studies by Collins et al. and Bowns et al., in which participation for dermatologists was not voluntary, showed not all clinicians embrace this new method as easily with satisfaction rates as low as 20 % [40, 46].
Teledermoscopy
Teledermoscopy is the obvious result of combining digitalized dermoscopic images with the technology provided by teledermatology (Fig. 34.2). The concept of teledermoscopy had already been developed as early as 1999 [47]. A major concern with teledermoscopy has always been its diagnostic accuracy and reliability, even more so than with regular teledermatology. The main reason, the relative high mortality risk found in melanoma skin cancer, warrants this caution. Still, the use of dermoscopy by trained dermoscopists increases diagnostic accuracy for pigmented and nonpigmented skin lesions, especially in melanoma [48, 49]. Many papers have been published reporting on the diagnostic accuracy [27, 28, 31, 32, 47, 50–56] and diagnostic reliability [32, 57–60] of teledermoscopy for (non) pigmented skin lesions. Several recent studies have reported high diagnostic accuracy of teledermoscopy (Cohen’s kappa 0.74–0.95), comparable with diagnostic accuracy found in face-to-face dermoscopic examination. Diagnostic reliability studies reported moderate to good concordance between observers (Cohen’s kappa 0.44–0.93). The diagnostic accuracy of teledermoscopy is mostly dependent on the observer’s level of experience [55] and the quality of the provided images.
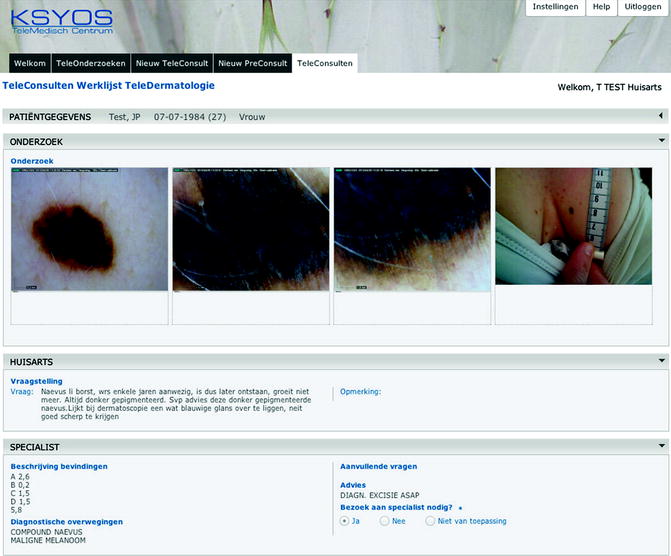
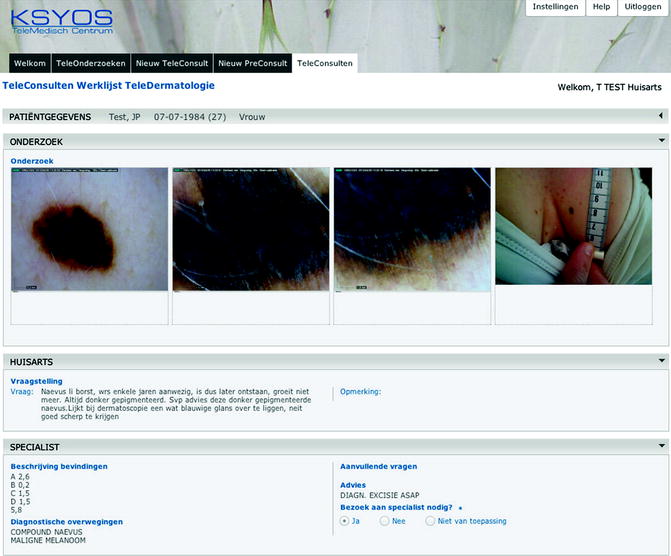
Fig. 34.2
A teledermoscopy consultation
As teledermoscopy is mostly used for the purpose of triage in skin cancer screening programs, it is perhaps of more importance to look at the management plan accuracy. Several studies have showed that, although agreement on a diagnostic level is sometimes moderate (possibly due to differences in terminology and classification), management plan agreement is high and equal to face-to-face consultation [31, 32, 56]. A recent study by Lim et al. reported on the first completely implemented and reimbursed teledermoscopy triage service [61]. Instead of a live visit, patients could be referred to a commercially run virtual lesion clinic (VLC). Results showed 88% prevented referrals to the dermatologist and faster detection and treatment of skin cancer patients in the patient group that was treated through the VLC.
Two risk factors must be addressed when practicing teledermoscopy. Its accuracy can be significantly lowered when diagnosis is performed by inexperienced teledermoscopists or when the dermoscopic photography is of a non-gradable quality. A study by Piccolo et al. showed an accuracy of kappa 0.69–0.87 with experienced dermatologists and an accuracy of kappa 0.40–0.56 with less experienced dermatologists [55]. Preliminary results from a study performed by the authors in the Netherlands showed a diagnostic accuracy of 29 % compared to in vivo diagnosis where the photographs were classified as non-gradable by two independent dermatologists (n = 7 patients) and an accuracy of 79 % where the photographs were classified as gradable (n = 24 patients). Photographs were taken by general practitioners during regular practice with a DermLite II Pro (3Gen, USA) attached to a Cybershot DSC-W560 digital camera (SONY, Japan).
Training is of vital importance for the referring and consulting actors in TD and even more so in teledermoscopy, both on how to capture a (dermoscopic) photo that is gradable and on the grading methods. Repetition and experience is key in obtaining and maintaining these skills.
From Pilot to Practice
Teledermatology services have started up all over the world, in most cases as part of a research program. Results are positive more often than not, but TD services have predominantly remained in the pilot setting [20]. Over the last 5 years however, in several countries, TD services have fully matured. In the USA, 36 active services have been identified with an annual median consult volume per service of 309 (range, 5–6,500) and all with a sustainable method of reimbursement [62]. In the Netherlands TD is practiced by the majority of Dutch GPs and dermatologists [18]. The consult volume is still increasing yearly, with over 30,000 teleconsultations performed in 2011 and its reimbursement integrated in the national health insurance plan. New Zealand has a successful melanoma screening service with clinics for dermoscopic photography across the country receiving over 20,000 patients per year [61].
The common factor in many of these success stories is the cooperation of both scientific institutes and commercial companies. This combination proves to be a driving force in the evolution of TD. The authors have described this route in a model called Health Management Practice, in which private and public parties and independent knowledge institutes jointly develop and study telemedicine tools and their outcomes and drive introduction in regular care [63].
Health Management Practice Model
Telemedicine Development
Technology and new healthcare processes lead to an integrated telemedicine service including software, hardware, infrastructure, hosting, education, and management meeting (national) requirements of safety, security, connectivity, and user-friendliness.
Health Management Research
Independent research aims to collect evidence that the use of telemedicine services increases efficiency leading to increased production volume and better quality of care at equal or lower costs.
Health Management Implementation
Telemedicine stakeholders – manufacturers, users, policy makers, and health insurers – should all be actively involved in the design of practice and reimbursement models. When significant reductions in costs on a macro-level have been proven, the next step is to create a healthy business case to support the complete telemedicine service. In order to assure successful implementation in regular care, active support and marketing from all stakeholders should take place.
Conclusion
Telemedicine is a potentially strong instrument to keep healthcare accessible and affordable in the future. Since its introduction in 1995, teledermatology has proven itself a highly successful healthcare delivery method in rural as well as in overpopulated areas for a number of different purposes, resulting in healthcare that can be more efficient and has higher quality and lower costs. Teledermoscopy is an exciting new method that can greatly improve triage of patients with skin cancer when implemented under the right conditions. Several mature teledermatology services with sustainable reimbursement models have developed in the last 5 years and more are on the way. Still, the success of teledermatology highly depends on the people who choose to adopt, use, and promote it and their determination to change the way healthcare is delivered.
Glossary
Teledermatology
delivery of dermatologic care through information and communication technology.
Teledermoscopy
digital dermoscopic lesion images (with or without clinical images) are transmitted electronically to a specialist for examination.
Telemedicine
delivery of healthcare and sharing of medical knowledge by use of information and communication technology.
References
1.
Strode SW, Gustke S, Allen A. Technical and clinical progress in telemedicine. JAMA. 1999;281:1066–8.PubMedCrossRef
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree