Fig. 17.1
Shows single RCM images (500 × 500 μm) of the different layers of normal skin. Panel (a) illustrates the morphology of the stratum corneum with the presence of a variable refractive surface (white asterisk) separated by dark linear valleys (red lines) representing skin folds, (b) shows typical honeycomb pattern of the epidermis at the spinous cell layer with regular appearance of polygonal keratinocytes, (c) shows small bright pigmented cells appearing as typical cobblestone pattern at the suprapapillary plate (red arrows), and (d) illustrates RCM morphology at the dermoepidermal junction (DEJ) with the presence of bright ring-like structures of pigmented basal cells (dashed circle)
Skin Cancer
Since RCM was first used to image live human skin in 1995 [7], numerous scientific studies have been carried out mainly focusing in keratinocytic and more recently in melanocytic and other skin tumors.
Malignant Keratinocytic Tumors
Basal Cell Carcinoma (BCC)
Maybe due to the reason that basal cell carcinoma (BCC) constitutes the most frequent malignancy of the skin, this is the cutaneous condition that has been more extensively analyzed by RCM [8, 9]. General confocal features of BCC include dense structures formed by homogeneous tumor cells that present elongated monomorphic nuclei along the same axis of orientation (“nuclear polarization”) (Fig. 17.2b), which is often reflected as peripheral palisading when surrounding a tumor island in a perpendicular manner to the border (Fig. 17.2a, d). Frequently, a dark area, which is probably constituted by mucin depots surrounding the relatively refractive tumor aggregates, correlates with the “clefting” observed in traditional histology. Ulrich et al. reported 13 cases of nodular, nodulocystic, and superficial BCCs and found a good linear correlation between dark areas on RCM and thickness of peritumoral mucin [10]. Occasionally, the stroma reflectance is higher than the tumor islands, which are observed and consequently termed “dark silhouettes” (Fig. 17.2c). Also important are the frequently observed disarranged keratinocytes located above the tumor, probably caused by the chronic actinic damage that is usually associated to this type of tumor. The superficial dermal blood vessels are also affected, appearing numerous, dilated with the presence of intense leukocyte trafficking inside, and sometimes accompanied by a prominent perivascular inflammatory infiltrate [11, 12] (Fig. 17.2c). Besides, pigmented BCC presents highly refractive dendritic and granular structures inside the tumor islands correlating to dendritic melanocytes and melanosomes, respectively (Fig. 17.2d). Melanophages located in the stroma are frequently observed as bright and big, poorly demarcated structures [13, 14].
Fig. 17.2
Basal cell carcinoma. (a) Hyporefractile tumor islands of BCC (white asterisk) which are separated from the surrounding stroma by dark cleft-like spaces (yellow arrowhead). Within the tumor islands, peripheral palisading of the cells may be observed (red arrowhead). (b) Nuclear streaming and elongated and polarized basal keratinocytes (red arrowheads). (c) Dark silhouettes (white asterisk) and large caliber blood vessels (BV) with blood flow on in vivo examination. Within the BV single erythrocytes can be visualized (red arrow). (d) Tumor islands of médium refractility (white asterisk) surrounding by tumor stroma with collagen and inflammatory cells. Dendritic figures (red arrowhead) are seen
In 2004, a multicenter study was performed in a large cohort of patients to evaluate sensitivity and specificity of RCM for in vivo diagnosis of basal cell carcinoma [8]. Five major criteria were established: elongated monomorphic basaloid nuclei, polarization of these nuclei along the same axis of orientation, prominent inflammatory infiltrate, increased dermal vasculature, and pleoamorphism of the overlying epidermis. The presence of two or more criteria was found to be 100 % sensitive and 53.6 % specific for the diagnosis of BCC, while four or more RCM criteria presented 95.7 % specificity and 82.9 % of sensitivity. As expected, specificity was directly proportional to the number of criteria observed by RCM and inversely proportional to the sensitivity of the criteria in the diagnosis of BCC.
RCM has been employed in different studies that describe the main features of different histological subtypes of BCC which is important in order to determine the therapeutics and prognosis of the tumor [15]. Infiltrative BCC is visualized as ill-defined invading structures composed of very polarized cells that penetrate and deform the dermis, while nodular BCC reveals well-defined tumor islands with peripheral palisading surrounded by dark areas.
Squamous Neoplasia
Squamous neoplasia derives from epidermal keratinocytes and is among the most common cutaneous malignancies. RCM features of invasive squamous cell carcinoma (SCC) and actinic keratosis (AK) have been previously described and have good correlation with histopathology [16–18]. At the corneum layer, some amorphous, variably refractive structures can be observed (Fig. 17.3a), which correspond to the scales of the lesion. At this level, some nucleated polygonal cells can be visualized as sharply delineated cells with a refractive thin outline surrounding a dark nucleus, corresponding to the parakeratotic cells of the histology. At the granular and spinous layers, the typical honeycombed pattern is altered and formed by pleomorphic cells with irregular size and shape (Fig. 17.3b). When there is severe atypia, the honeycombed pattern is replaced by a completely disarranged epidermal pattern. Dyskeratotic cells in the granular and spinous layers can also be seen with confocal microscopy as sharply delineated round structures surrounding a dark oval space (nucleus). Another characteristic feature is observed inside the dermal papillary rings as round dark spaces with infrequent leukocyte trafficking inside (Fig. 17.3c). These spaces correspond to the typical dotted and glomerular vessels seen in dermoscopy of SC [19]. Confocal imaging of the upper dermal layer generally reveals extensive highly refractive reticulated thick fibers which correlates to the altered collagen that constitutes the solar elastosis commonly found in this malignancy (Fig. 17.3d). An increasing number and frequency of all these abnormal RCM features can be visualized along the spectrum of squamous neoplasia. A recent study by Ulrich et al. evaluated ten cases of Bowen’s disease (BD) by RCM and correlated the findings to routine histology [20]. The most prevalent features were stratum corneum disruption, atypical honeycomb pattern, presence of two types of targetoid cells, and round-to-oval dermal blood vessels. They also observed parakeratosis, inflammatory infiltrate, and multinucleated cells. The results of this study show that RCM can be used for rapid in vivo diagnosis of BD and its distinction from other non-melanocytic skin cancer and inflammatory simulators like psoriasis or eczema.
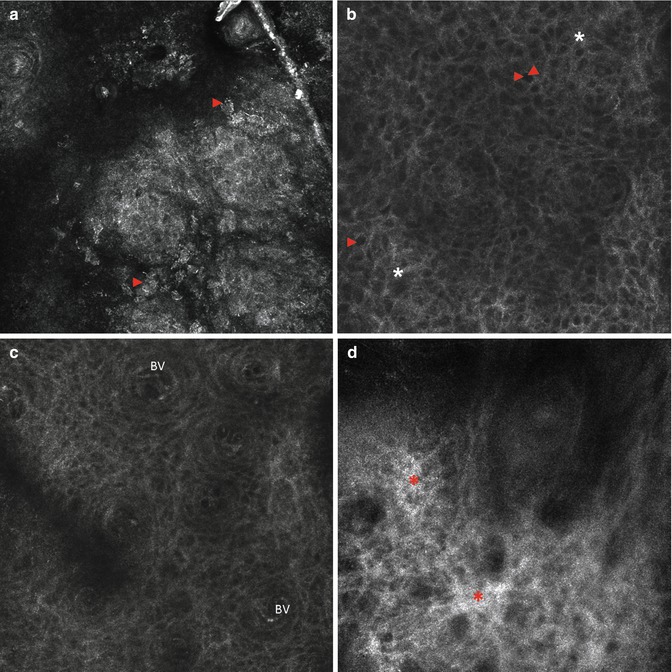
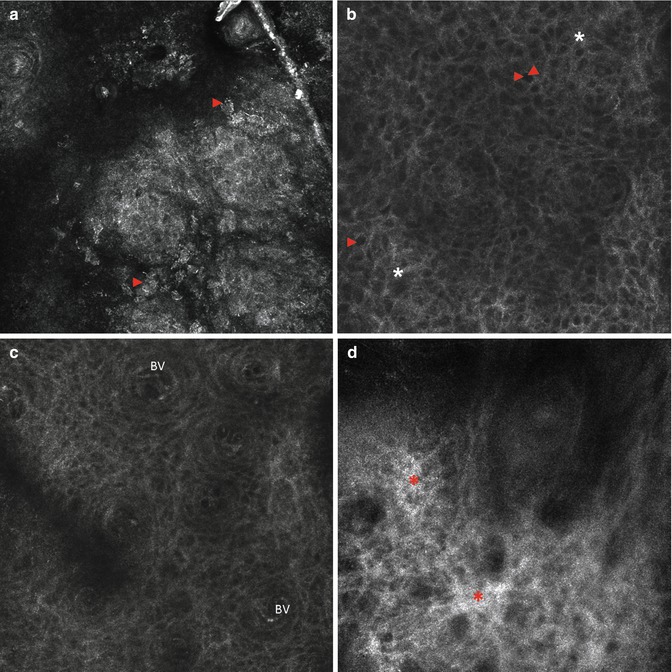
Fig. 17.3
Representative single RCM images (500 × 500 μm) of actinic keratoses. (a) Disruption of the stratum corneum with single detached keratinocytes (red arrowheads). (b) Atypical honeycomb pattern of granular-spinous layers with great variation of cells and nuclei (red arrowhead) as well as broadened and irregular cell borders (white asterisk). (c) Dilated blood vessels (BV) in the center of the dermal papillae. (d) Highly refractive reticulated thick fibers (red asterisks) which correlate to the altered collagen
The detection of dermal RCM features of AK, BD, and SCC may be limited by the presence of significant hyperkeratosis which sometimes worsens its optical resolution in deeper areas. To solve this problem, some chemical or physical methods can be previously applied to remove the scales.
Melanoma
Melanoma is a malignant proliferation of melanocytes in which prognosis is related to depth of dermal invasion. This skin cancer is curable if diagnosed and excised at early stages which explains the importance of an early diagnosis [21]. Clinical diagnosis of melanoma is based on the ABCD criteria, but the accuracy of this method is as low as 64 % [22]. To avoid unnecessary surgical biopsies, which are painful and time-consuming and leave scars, noninvasive techniques for improving clinical diagnostic accuracy are being developed such as dermoscopy, high-frequency ultrasound, optical coherence tomography, magnetic resonance imaging, and RCM [6]. For its ability to explore at cellular level resolution skin structures up to 200 μm in depth, horizontal imaging, and noninvasiveness, RCM may be understood as a natural link between dermoscopy and histopathology, especially useful for diagnosis of early melanomas.
In the recent years, a good correlation between confocal aspects and specific dermoscopic features, such as pigment network, peripheral streaks, or pigment globules, has been demonstrated as well as the correspondence of confocal mosaics at dermoepidermal junction and global dermoscopic patterns [23–25]. Atypical pigment network, characteristic of atypical nevi and melanoma, corresponds to “non-edged papillae,” while irregular pigment globules correspond to irregularly shaped clusters formed by atypical cells in melanomas or regular cytology in benign lesions. Pigment dots are clearly visualized by RCM as pagetoid melanocytes in melanoma that are easily distinguished from the melanin clumps typically found in common nevi [26]. Moreover, RCM is particularly useful for the interpretation of the bluish pigmentation and for differentiating the plump bright cells infiltrating the dermal papillae that correspond to melanophages from the malignant melanocytes that, singularly or in clusters, infiltrate the dermis in invasive melanomas [27, 28].
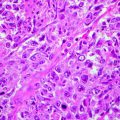
In a similar manner, the main histopathological features of melanoma have been identified with RCM showing high sensitivity and specificity values [5, 29]: altered epidermal architecture with pagetoid cells (Fig. 17.4a, b), ill-defined dermal papillae with cytological atypia at dermoepidermal junction (Fig. 17.4c), cerebriform clusters, and nucleated cells in superficial dermis (Fig. 17.4d). Furthermore, very high sensitivity and specificity values of some confocal aspects, such as melanocyte cytology, disarray of the architecture, and poorly defined keratinocyte cell borders, were identified by Gerger et al., comparing two preselected images per lesion from a database of 27 melanomas and 90 nevi, the majority of which corresponded to clearly benign lesions [30].
Fig. 17.4
Representative single RCM images (500 × 500 μm) of melanoma. (a) Presence of both dendritic (red arrowhead) and round (yellow arrowhead) pagetoid melanocytes in upper epidermal layers. (b) Complete disruption of the epidermal architecture resulting in a disarranged pattern. (c) Atypical melanocytes at the DEJ (yellow arrowheads) as well as in the dermal papillae containng blood vessels (BV). (d) Large dilated and elongated blood vessels (BV) in the upper dermis
At present, two different confocal diagnosis algorithms for melanoma have been developed. Based on 102 melanocytic lesions, six criteria were identified as independently correlated with a melanoma diagnosis, and a diagnostic algorithm was developed [31]. Two major criteria were scored 2 points, corresponding to the cytological atypia at basal cell layers and non-edged papillae at dermoepidermal junction. Four minor criteria, represented by the presence of roundish cells in superficial layers spreading upwards in a pagetoid fashion, pagetoid cells widespread throughout the lesion, cerebriform clusters in the papillary dermis, and nucleated cells within dermal papilla, were scored 1 point. Considering a threshold score equal to or greater than 3, 97.3 % sensitivity and 72.3 % specificity were obtained, whereas increasing the threshold, specificity can be increased with a consequent decrement of sensitivity. Recently, the validity of the algorithm was blindly tested on a larger population of equivocal melanocytic lesions, showing in a reproducible clinical setting a 92 % sensitivity and 70 % specificity [5]. Segura et al. developed a two-step method for the diagnosis of melanoma by RCM [32]. In a preliminary study, they evaluated 154 skin tumors, including 100 melanocytic and 54 non-melanocytic lesions, by RCM before their excision. They observed four confocal features that differentiated melanocytic from non-melanocytic lesions: cobblestone pattern of epidermal layers, pagetoid spread, mesh appearance of the dermoepidermal junction, and the presence of dermal nests. Within melanocytic lesions, the presence of roundish suprabasal cells and atypical nucleated cells in the dermis was associated with melanoma, and the presence of edged papillae and typical basal cells was associated with nevi. Furthermore, a recent study [33] tried to determine whether specific histological features in dysplastic nevi had reliable correlates on confocal microscopy and developed an in vivo microscopic grading system, which consists in a simplified algorithm to distinguish dysplastic nevi from melanoma and non-dysplastic nevi. Sixty melanocytic lesions with equivocal dermatoscopic aspects were analyzed by RCM and histopathology, and they found good correlation between their features. As observed by RCM, dysplastic nevi were characterized by a ringed pattern, in association with a meshwork pattern in a large proportion of cases, along with atypical junctional cells in the center of the lesion and irregular junctional nests with short interconnections. The simultaneous presence of cytological atypia and of atypical junctional nests (irregular, with short interconnections, and/or with nonhomogeneous cellularity) was consistent with histological dysplasia, whereas widespread pagetoid infiltration, widespread cytological atypia at the junction, and non-edged papillae suggested melanoma diagnosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree