Fig. 14.1
Giant non-involuting congenital hemangioma in the thigh with functional gait impairment. Excision by lenticular incision and linear closure technique (a). Postoperative results (b)
5.
6.
IH of the nose producing secondary cartilage deformity
7.
Large IH in the lip producing facial disfigurement, speech impairment, and feeding difficulties [9]
8.
Ulcerated and bleeding IH nonresponsive to medical and/or laser treatment
Thanks to the introduction of medical treatment with propranolol for critical IH, nowadays the bleeding control during surgery for early IH excision has been much easier. Surgery for excision of exuberant fibrofatty tissue and correction of contour deformities can now be performed during early infancy after the 6 month of medical treatment with propranolol, optimizing the cosmetic final result and minimizing the psychological side effects of stigmatization.
Techniques
The main purpose of surgery for the removal of IH, regardless of their life cycle phase (proliferative or involutive), is to optimize the final cosmetic result [10]. When approaching large hemangiomas in the proliferating phase, intraoperative bleeding control is the main challenge for the surgeon: a few surgical tricks can be employed in order to minimize intraoperative bleeding.
Two different surgical techniques for partial or total excision of a critical hemangioma which meet this challenge can be used:
The first one is the traditional method used for the removal of skin masses with a lenticular-shaped incision and linear closure: this technique is proposed for lesions larger than 3.0 cm in diameter at the base. The skin incision must be oriented with the axis of the relaxed skin tension lines and must be drawn along the border between affected tissue and normal skin [15, 16].
Intraoperative blood losses can be conspicuous for patient’s age and weight.
In order to minimize bleeding by reducing the lesion vascular supply, a technique of hemostatic “squeezing” at the tumor’s base can be employed for removal of the most voluminous tumors.
A special clamp was designed. This was manufactured in such a way that it can be disassembled into two parts by removing a screw which acts as a hinge (Fig. 14.2). Reinsertion of the screw enables reassembly of the two parts as a clamp. The two parts of this disassembled clamp are blindly inserted under the skin through a small skin incision adjacent to the hemangioma and passed in the subcutaneous tissue on opposite sides of the mass. The two parts are then reassembled after insertion of the screw, and the clamp is closed underneath the hemangioma base thus compressing its blood supply (Fig. 14.3).
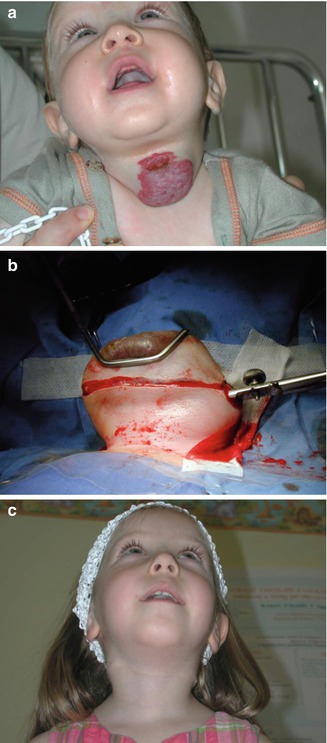
Fig. 14.2
A homemade special clamp that can be disassembled in two parts by removing a screw that acts as a hinge
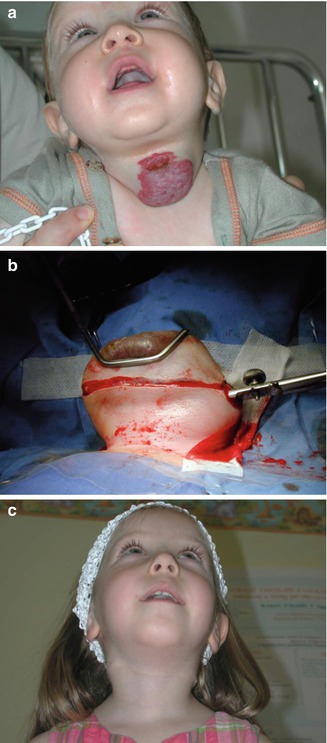
Fig. 14.3
Lenticular incision and linear closure technique for excision of a large cervical hemangioma in a 9-month-old girl (a). An original clamp with de-joined branches is blindly inserted under the skin for hemostatic squeezing at the base of the vascular tumor (b). Follow-up control 6 months after surgery (c)
In order to make the clamp’s blind insertion easier and reduce vascularity, a variable volume of epinephrine solution in normal saline (0.1 % dilution) is injected within the subcutaneous tissue underlying the hemangioma and circumferentially around the lesion [5].
Detachment of the vascular tumor from the deep plans and the surrounding tissues is then obtained using monopolar diathermy. After resection, the clamp is released and complete bleeding control is accomplished using bipolar diathermy on the residual afferent vessels which normally present a radial distribution.
Linear closure by side to side approximation of the wound edges is finally obtained: intradermal absorbable running suture is tailored to close the skin. Sometimes it is necessary to lengthen the skin incision along its main axis up to 1/3 of its original size from each end in order to avoid “dog ears” at the wound extremities.
The “round-block technique,” described by Mulliken et al. [17] and more recently adopted by the authors, is indicated for excision of smaller lesions, sized less than 30 mm in diameter.
The advantages of using the purse–string closure technique for removal of localized hemangiomas consist of minimizing the subsequent scar length (up to 50 % shorter compared with results obtained from the traditional linear closure technique) and minimizing the adjacent structure distortion, since tension is equally applied along multiple radial lines with a symmetrical concentric distribution pattern rather than along a main axis perpendicular to the linear wound.
In our experience preliminary hydrostatic undermining by saline injection is always useful before performing a circular skin incision in order to detach the vascular tumor from the deep plans and the surrounding tissues and to encourage a symmetrical distortion of adjacent structures by concentric distribution of tension lines.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







