Chapter Outline
Tests for the acute-phase response 93
Whole blood viscosity 97
Heterophile antibodies in serum: diagnosis of infectious mononucleosis 97
Screening tests for infectious mononucleosis 97
Demonstration of lupus erythematosus cells 98
Erythropoietin 98
Autonomous in vitro erythropoiesis 99
Thrombopoietin 99
Haematological tests in sports medicine 99
Red cell parameters 100
Whole blood viscosity and erythrocyte sedimentation rate 100
Erythropoietin 100
Principles of detection of microorganisms 100
Examination of blood films for parasites 100
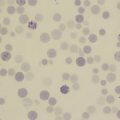
Microscopic diagnosis of malaria 101
Rapid diagnostic tests for malaria 102
Leishmaniasis 106
Diagnosis of leishmaniasis in the haematology laboratory 108
Trypanosomiasis 108
African trypanosomiasis 108
American trypanosomiasis 108
Diagnosis of trypanosomiasis in the haematology laboratory 108
Filariasis and loiasis 109
Diagnosis of filariasis in the haematology laboratory 110
Babesiosis 110
Ehrlichiosis and anaplasmosis 110
Tests for the acute-phase response
Inflammatory response to tissue injury (i.e. the acute-phase response) includes alteration in serum protein concentration, especially increases in fibrinogen, haptoglobin, caeruloplasmin, immunoglobulins (Ig) and C-reactive protein (CRP), and a decrease in albumin. The changes occur in acute infection, during active phases of chronic inflammation, with malignancy, in acute tissue damage (e.g. following acute myocardial infarction) and with physical injury. Measurement of the acute-phase response is a helpful indicator of the presence and extent of inflammation or tissue damage, and of the response to treatment. The usual tests for detecting an acute-phase response are estimation of CRP and measurement of the erythrocyte sedimentation rate (ESR); some studies have suggested that plasma viscosity is also a useful indicator, but there is debate about the relative value of these tests. ,
Kits that are sensitive and precise are available for CRP assay; small increases in serum levels of CRP can often be detected before any clinical features become apparent, whereas as a tissue-damaging process resolves, the serum level rapidly decreases to within the normal range (< 5 mg/l). The ESR is slower to respond to changes in acute disease activity and it is insensitive to small changes in disease activity. It is less specific than CRP because it is also influenced by immunoglobulins (which are not acute-phase reactants) and by anaemia. Moreover, because the rate of change of ESR is slower than that of CRP, it rarely reflects the current disease activity and clinical state of the patient as closely as the CRP concentration. The ESR is a useful screening test, and the conventional manual ESR method is simple, cheap and independent of a power supply, thus making it suitable for point-of-care (near-patient) testing. It is recommended that, in clinical practice, the two tests should be carried out in tandem. Because a CRP assay is a biochemical test usually performed in the clinical chemistry laboratory, it will not be discussed further here.
Erythrocyte sedimentation rate
The method for measuring the ESR recommended by the International Council for Standardisation in Haematology (ICSH) and also by various national authorities is based on that of Westergren, who developed the test in 1921 for studying patients with pulmonary tuberculosis. The ESR is the measurement of the sedimentation of red cells in diluted blood after standing for 1 h in an open-ended glass tube of 30 cm length mounted vertically on a stand.
Conventional Westergren method
The recommended tube is a straight glass or rigid transparent plastic tube 30 cm in length and no less than 2.55 mm in diameter. The bore must be uniform to within 5% throughout. A scale graduated in mm extends over the lower 20 cm. The tube must be clean and dry and kept free from dust. If reusable, before being reused it should be thoroughly washed in tap water and then rinsed with deionised or distilled water and allowed to dry. Specially made racks with adjustable levelling screws are available for holding the sedimentation tubes firmly in an exactly vertical position. The rack must be constructed so that there will be no leakage of the blood from the tube. It is conventional to set up sedimentation rate tests at room temperature (18–25 °C). Sedimentation is normally accelerated as the temperature increases, and if the test is to be carried out at a higher ambient temperature, a normal range should be established for that temperature. Exceptionally, when high thermal amplitude cold agglutinins are present, sedimentation becomes noticeably less rapid as the temperature is increased toward 37 °C.
Method
The method described below, originally described by the ICSH and now adopted by the Clinical and Laboratory Standards Institute (CLSI) as its approved method, is intended to provide a reference method for verifying the reliability of any modification of the test.
Either collect venous blood in ethylenediaminetetra-acetic acid (EDTA) and dilute a sample accurately in the proportion of 1 volume of citrate to 4 volumes of blood, or collect the blood directly into citrate diluent. For the diluent, prepare a solution of 109 mmol/l trisodium citrate (32 g/l Na 3 C 6 H 5 O 7 •2H 2 O). Filter through a Micropore filter (0.22 mm) into a sterile bottle. It can be stored for several months at 4 °C but must be discarded if it becomes turbid through the growth of mould.
The test should be carried out on the diluted sample within 4 h of collecting the blood, although a delay of up to 6 h is permissible provided that the blood is kept at 4 °C. EDTA-anticoagulated blood can be used up to 24 h if the specimen is kept at 4 °C, provided that 1 volume of 109 mmol/l (32 g/l) trisodium citrate is added to 4 volumes of blood immediately before the test is performed.
Mix the blood sample thoroughly and draw it up into the Westergren tube to the 200 mm mark by means of a teat or a mechanical device; mouth suction should never be used. Place the tube exactly vertical and leave undisturbed for exactly 60 min, free from vibrations and draughts and not exposed to direct sunlight. Read the height of the clear plasma above the upper limit of the column of sedimenting cells to the nearest 1 mm. The result is expressed as ESR = X mm in 1 h. A poor delineation of the upper layer of red cells sometimes occurs, especially when there is a high reticulocyte count.
Range in health
The mean values and the upper limit for 95% of normal adults are given in Table 6-1 . There is a progressive increase with age, but it is difficult to define a strictly healthy population for determining normal values in individuals older than 70 years. In the newborn, the ESR is usually low. In childhood and adolescence, it is the same as for normal men with no differences between boys and girls. It is increased in pregnancy, especially in the later stages, and can be independent of anaemia; this is due to the physiological effect of an increase in the plasma volume causing haemodilution.
| Age Range (Years) | ESR Mean (mm in 1 h) |
|---|---|
| 10–19 | 8 |
| 20–29 | 10.8 |
| 30–39 | 10.4 |
| 40–49 | 13.6 |
| 50–59 | 14.2 |
| 60–69 | 16 |
| 70–79 | 16.5 |
| 80–91 | 15.8 |
| Pregnancy | |
| Early gestation | 48 (62 if anaemic) |
| Later gestation | 70 (95 if anaemic) |
In the newborn, the ESR has been reported to be 0–2 mm in 1 h, increasing to 4 mm in 1 h at 1 week, up to 17 mm in 1 h by day 14, and then to 10–20 mm in 1 h for both girls and boys, until puberty. However, as the samples in infants were obtained by the capillary method, results are not directly comparable to the Westergren method.
Modified methods
Length of tube
The overall length of the tube is not a critical dimension for the test provided that it fits firmly in an appropriate holding device. The tube must, however, be long enough to ensure that packing of the cells does not start before the test has been completed.
Plastic tubes
A number of plastic materials (e.g. polypropylene and polycarbonate) are recommended as substitutes for glass in Westergren tubes. However, not all plastics have similar properties, and it must be demonstrated that the ESR with the chosen tubes is reproducible and not affected by the plastic.
Disposable glass tubes
Disposable glass tubes should be supplied clean and dry and ready for use. It is necessary to show that neither the tube material nor the manufacturer’s cleaning process affects the ESR.
Capillary method
Short tubes of narrower bore than that of the standard tube are available, mainly for tests on infants. These are, however, no longer in general use, and it is necessary to establish normal ranges or a correction factor to convert results to an approximation of ESR by the Westergren method.
Test duration
Sedimentation is measured after aggregation has occurred and before the cells start to pack, usually at 18–24 min. From the rate during this time period the sedimentation that would have occurred at 60 min is derived and converted to the conventional ESR equivalent by an algorithm.
Sloping tube
Red cells sediment more quickly when streaming down the wall of a sloped tube. This phenomenon has been incorporated into automated systems in which the end-point is read after 20 min with the tube held at an angle of 18° from the vertical. Incorporating a low-speed centrifugation step (approximately 800 rpm) in this automated method reduces the end-point time further. These methods have been shown to give results comparable to the conventional method.
Anticoagulant
EDTA-anticoagulated blood can be used without citrate dilution, at least if packed cell volume (PCV) is below 0.36 l/l or haemoglobin concentration (Hb) is below 110 g/l; less precise results are obtained when the PCV is higher. Because of the biohazard risk of blood contamination inherent in using open-ended tubes, it is now recommended that, where possible, a closed system be used in routine practice. Manual methods are available that avoid transfer of the blood into the sedimentation tube. Automated closed systems use blood collected in special evacuated tubes containing blood anticoagulated with either citrate or EDTA. A sample is taken up through a pierceable cap and then automatically diluted in the system if this is required.
Whenever a different method or tube is planned, a preliminary test should be carried out to check precision and to compare results with those obtained by the CLSI standardised method described earlier.
Evaluation of a new routine method
For the evaluation of a new ESR method the test should be carried out on at least 60 samples. These samples could be collected separately from the same subjects in accordance with specified requirements (e.g. undiluted EDTA samples or directly into tubes containing citrate). The samples should come from patients with a wide variety of diseases (as well as from normal subjects) to cover the range of ESR from 15 to 105 mm, with approximately the same number of samples in each quartile. If any test fails to give a clear-cut plasma erythrocyte interface in either the test system or the standardised test, the pair of values should be eliminated from the data.
Any new method may be considered to be satisfactory if 95% of results differ consistently by no more than 5%. However, because the ESR may be affected by several uncontrolled variables, the reference method cannot be used to adjust the measurements that are obtained. Thus if the new method gives disparate readings, it will be necessary to establish a normal range specifically for the method.
Quality control
The standardised method can be used as a quality-control procedure for routine tests or, alternatively, stabilised whole blood preparations can be used for the daily control of automated systems (e.g. ESR-Chex, www.streck.com ). Three or four specimens of EDTA blood kept at 4 °C will also serve as a control on the following day.
Another control procedure is to calculate the daily cumulative mean, which is relatively stable when at least 100 specimens are tested each day in a consistent setting (see Chapter 25 ). A coefficient of variation of < 15% between daily sets appears to be a satisfactory index for monitoring instrument performance.
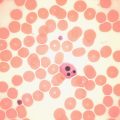
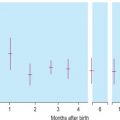
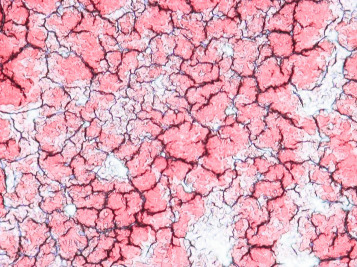
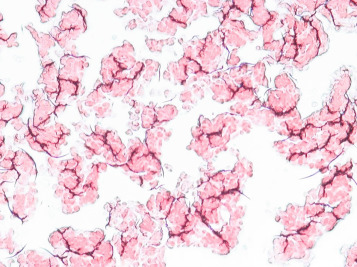
Semiquantitative slide method
Enhanced red cell adhesion/aggregation can be demonstrated by allowing a drop of citrated blood to dry on a slide. An estimate of the amount of cell aggregation on the film by image analysis provides a semiquantitative measure of the acute-phase response that appears to correlate with the ESR. Based on this principle, serial microscopic images of red cells aggregating on a glass slide taken every 30 s for 5 min can distinguish a normal ESR from a high value ( Figs. 6-1 and 6-2 ). The images demonstrate greater spacing of cells in blood with higher ESR values compared with blood with lower ESR values.
Mechanism of erythrocyte sedimentation
The rate of fall of the red cells is influenced by a number of interacting factors. It depends on the difference in specific gravity between red cells and plasma, but it is influenced very greatly by the extent to which the red cells form rouleaux, since these sediment more rapidly than single cells. Other factors that affect sedimentation include the ratio of red cells to plasma (i.e. the PCV), the plasma viscosity, the verticality (or otherwise) of the sedimentation tube, the bore of the tube and the dilution (if any) of the blood.
The rouleaux formation and the red cell clumping that are associated with the increased ESR mainly reflect the concentrations of fibrinogen and other acute-phase proteins (e.g. haptoglobin, caeruloplasmin, α 1 -acid glycoprotein, α 1 -antitrypsin, and CRP). Rouleaux formation is also enhanced by the immunoglobulins and is retarded by albumin. Defibrinated blood normally sediments extremely slowly (i.e. not more than 1 mm in 1 h) unless the serum globulin concentration is increased or there is an unusually high globulin:albumin ratio.
Anaemia, by altering the ratio of red cells to plasma, encourages rouleaux formation and accelerates sedimentation. In anaemia, cellular factors may also affect sedimentation. Thus, in iron deficiency anaemia, a reduction in the intrinsic ability of red cells to sediment may compensate for the accelerating effect of an increased proportion of plasma.
Sedimentation can be observed to take place in three stages: a preliminary stage of at least a few minutes during which time rouleaux occur and aggregates form; then a period in which the sinking of the aggregates takes place at a constant speed; and finally, a phase during which the rate of sedimentation slows as the aggregated cells pack at the bottom of the tube. It is obvious that the longer the tube used, the longer the second period can last and the greater the sedimentation rate may appear to be.
Although ESR is a nonspecific phenomenon, its measurement is clinically useful in disorders associated with an increased production of acute-phase proteins. In rheumatoid arthritis or tuberculosis it provides an index of progress of the disease, and it is of considerable value in the diagnosis of temporal arteritis and polymyalgia rheumatica. It is often used if multiple myeloma is suspected, but when the myeloma is nonsecretory or light chain type, a normal ESR does not exclude this diagnosis.
An elevated ESR occurs as an early feature in myocardial infarction. Although a normal ESR cannot be taken to exclude the presence of organic disease, the vast majority of acute or chronic infections and most neoplastic and degenerative diseases are associated with changes in the plasma proteins that lead to an acceleration of sedimentation. An increased ESR in subjects who are human immunodeficiency virus (HIV) seropositive seems to be an early predictive marker of progression toward acquired immune deficiency syndrome (AIDS). The ESR is less helpful in countries where chronic diseases are rife; however, one study has shown that very high ESRs (higher than 100 mm/h) have a specificity of 0.99 and a positive predictive value of 0.9 for an acute or chronic infection. The ESR is influenced by age, stage of the menstrual cycle and medications taken (corticosteroids, oral contraceptives). It is especially low (0-1 mm) in polycythaemia, hypofibrinogenaemia and congestive cardiac failure and when there are abnormalities of the red cells such as poikilocytosis, spherocytosis or sickle cells. In cases of performance-enhancing drug intake by athletes (discussed below) the ESR values are generally lower than the usual value for the individual and as a result of the increase in Hb (i.e. the effect of secondary polycythaemia).
Plasma viscosity
The ESR and plasma viscosity generally increase in parallel. Plasma viscosity is, however, primarily dependent on the concentration of plasma proteins, especially fibrinogen, and it is not affected by anaemia. Changes in the ESR may lag behind changes in plasma viscosity by 24–48 h, and viscosity seems to reflect the clinical severity of disease more closely than does the ESR.
There are several types of viscometers, including rotational and capillary types that are suitable for routine use, and, as for ESR methods, automated closed-tube methods are available. The main use of plasma viscosity is in the investigation of individuals with suspected hyperviscosity, myeloma and macroglobulinaemia. In conjunction with the ESR and CRP, the plasma viscosity can be used as a marker of inflammation. The viscosity test should be carried out as described in the instruction manual for the particular instrument used.
Reference values
Each laboratory should establish its own reference values for plasma viscosity. As a general guide, ICSH has recorded that with the Harkness capillary viscometer normal plasma has a viscosity of 1.16 to 1.33 mPa/s (if expressed in poise [P], 1 cP = 1 mPa/s) at 37 °C and 1.50 to 1.72 mPa/s at 25 °C. Plasma viscosity is lower in the newborn (0.98 to 1.25 mPa/s at 37 °C), increasing to adult values by the third year; it is slightly higher in old age. There are no significant differences in plasma viscosity between men and women or in pregnancy. It is remarkably constant in health, with little or no diurnal variation, and it is not affected by exercise. A change of only 0.03 to 0.05 mPa/s is thus likely to be clinically significant.
Whole blood viscosity
The viscosity of whole blood reflects its rheological properties; it is influenced by PCV, plasma viscosity, red cell aggregation and red cell deformability. It is especially sensitive to PCV, with which it is closely correlated. The clinical interpretation of its measurement must also take into account the interaction of the red cells with blood vessels, which greatly influences blood flow in vivo.
Guidelines for measuring blood viscosity and red cell deformability by standardised methods have been published. Rotational and capillary viscometers are suitable for measuring blood viscosity; deformability can be measured by recording the rate at which red cells in suspension pass through a filter with pores 3–5 mm in diameter.
Heterophile antibodies in serum: diagnosis of infectious mononucleosis
Infectious mononucleosis (IM) is caused by the Epstein–Barr virus. The immune response that develops in response to virus-infected cells includes not only antibodies to viral antigens but also characteristic heterophile antibodies. Before the nature of this reaction was understood, Paul and Bunnell demonstrated the antibodies as agglutinins directed against sheep red cells. They are, in fact, not specific for sheep red cells but also react with horse and ox, but not human, red cells. They are IgM globulins, which are immunologically related to, but distinct from, antibodies that occur in response to the Forssman antigens. The latter are widely spread in animal tissue; they occur at low titre in healthy individuals and at high titre in serum sickness and in some leukaemias and lymphomas. , In these non-IM conditions, the antibody can be absorbed out by guinea pig cells. Thus, for the diagnosis of IM, it is necessary to demonstrate that the antibody present has the characteristics of the Paul–Bunnell antibody (i.e. it is absorbed by ox red cells but not by guinea pig kidney). This is the basis of the absorption tests for IM (e.g. ‘Monospot’ test, www.meridianbioscience.com/diagnostic-products/mononucleosis/monospot/monospot-latex.aspx ). Immunofluorescent antibody tests have been developed to distinguish the IgM antibody, which occurs at high titre in the early phase of IM and diminishes during convalescence, from the IgG antibody, which persists at high titre for years after infection , and which also occurs in the non-IM infections. ,
Screening tests for infectious mononucleosis
The reagents for IM screening are available commercially in diagnostic kits from several manufacturers. Guinea pig cells can also be manufactured locally as described in previous editions. Some kits are based on agglutination of stabilised horse red cells or antigen-coated latex particles to which IM antibody binds. An extensive evaluation of 14 slide tests for the UK Medical Devices Agency (MDA) showed them to have a sensitivity between 0.87 and 1.00 and a specificity of 0.97 to 1.00, with an overall accuracy in the order of 91% to 100%. False-positive reactions have been reported in malaria, toxoplasmosis, and cytomegalovirus infection; autoimmune diseases; and even occasionally without any apparent underlying disease. , False-negative reactions occur if the test is carried out before the level of heterophile antibody has increased or conversely when it has decreased. False-negative reactions may also occur in the very young and the very old. In the UK MDA study the best performance was obtained with the Clearview IM test (Alere Ltd, Stockport, UK, www.alere.com/en/home/product-details/clearview-mono-au.html?c=AU ), which uses latex-labelled bovine erythrocyte glycoprotein. IM heterophile antibody binds to this to form a complex that presents as a band in the result window ( Fig. 6-3 ). The test can be performed with diluted whole blood as well as with plasma or serum.

Screening tests are also available based on enzyme-linked immunosorbent assay (ELISA) and immunochromatographic assay. These tests are more elaborate than the slide screening test described earlier, but they are less likely to give a false result.
Clinical value
Tests for the heterophile antibody are useful for diagnosis. Antibodies are often present as early as the 4th to 6th day of the disease and are almost always found by the 21st day. They disappear as a rule within 4–5 months. There is no unanimity as to how frequently negative reactions are found in ‘true’ IM. Occasionally, the characteristic antibodies develop very late in the course of the disease, perhaps weeks or even months after the patient becomes ill. It is also known that a positive reaction may be transient and that the antibodies may be present at such low titres that they may be missed or may produce anomalous agglutination reactions when associated with the naturally occurring antibody at similar titres. For all of these reasons, it is difficult to state categorically that any particular patient has not or will not produce antibodies. Antibodies specific for Epstein–Barr virus have been demonstrated in the serum of 86% of patients with clinical and/or haematological features of IM.
There is no substantial evidence that sera containing agglutinins in high concentration giving the typical reactions of IM are found in diseases unless there is coexisting IM. In particular, the heterophile antibody titres in lymphomas are similar to those found in unselected patients not suffering from IM.
Demonstration of lupus erythematosus cells
Antinuclear antibodies, or antinuclear factors (ANFs), occur in the serum in a wide range of autoimmune disorders, including systemic lupus erythematosus (SLE). Descriptions of the LE cell test, which has now been superseded by immunological tests, can be found in earlier editions of this book.
Erythropoietin
Erythropoietin regulates red cell production. It is a heat-stable glycoprotein with a molecular weight of about 34 kDa. It is produced mainly in the kidney. Only a small quantity is demonstrable in normal plasma or urine.
A pure form of human erythropoietin from recombinant deoxyribonucleic acid (DNA) (recombinant human erythropoietin, r-HuEpo) is available for diagnostic assay methods by ELISA, enzyme immunoassay and radioimmune assay. Commercial kits are available that are reliable and sensitive, although there is some intermethod variability. Results are expressed in international units (iu) by reference to a World Health Organisation (WHO) standard. This was originally a urinary extract, and a preparation is available with a potency of 10 iu per ampoule. The present standard has been established for r-HuEpo with a potency of 86 iu per ampoule.
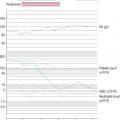
Reference range
The normal reference range in plasma or serum varies considerably according to the method of assay. For the ELISA method used by the UK supraregional service, the normal range is 9.1 to 30.8 iu/l. With test kits, in the steady state without anaemia, it is usually given as 5 to 25 iu/l or slightly higher. In normal children, the levels are the same as those in adults, except for infants younger than 2 months when the levels are lower.
There is a diurnal variation, with the highest values at night. In pregnancy, erythropoietin concentration increases with gestation.
Significance
Increased levels of erythropoietin are found in the plasma (or serum) in various anaemias, and there is normally an inverse relationship between haemoglobin and erythropoietin. In thalassaemia, erythropoietin is lower than in iron deficiency with the same degree of anaemia, but there is a close inverse correlation with the red cell count. In renal disease, there is a progressive decline in the erythropoietin response to anaemia, and in end-stage renal failure the concentration is normal or even lower than normal despite increasing anaemia. In renal patients receiving dialysis, erythropoietin treatment may cause functional iron deficiency.
Some impairment of production of erythropoietin may occur in association with neoplasms and chronic inflammatory diseases. Increased concentrations of erythropoietin occur in secondary polycythaemia as a result of respiratory and cardiac disease; in the presence of abnormal haemoglobins with high oxygen affinity; and in association with carcinoma of the kidney and other erythropoietin-secreting tumours such as hepatoma, uterine fibroma and ovarian carcinoma.
In primary polycythaemia (‘polycythaemia vera’), the plasma erythropoietin level is usually lower than normal even when the Hb has been reduced by venesection. , In secondary polycythaemia, the level of erythropoietin is never below normal. An assay is particularly useful in patients with erythrocytosis of undetermined cause; low erythropoietin has a specificity of 0.92 with moderate sensitivity for diagnosing primary polycythaemia. However, in such cases there may be an intermittent increase in erythropoietin secretion. Thus determining its level in a single sample of plasma may be misleading. Low levels have been found in one-third of cases of primary (essential) thrombocythaemia, especially when Hb is at a high normal level.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree