Chapter Outline
Biohazard precautions 1
Procurement of venous blood 1
Capillary blood 3
Collection of capillary blood 3
Blood film preparation 3
Differences between capillary and venous blood 3
Sample homogeneity 4
Serum 4
Cold agglutinins 4
Anticoagulants 4
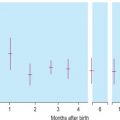
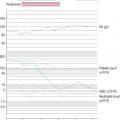
Effects of storage on the blood count 5
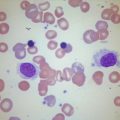
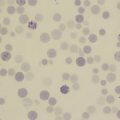
Effects of storage on blood cell morphology 5
Acknowledgement
The author wishes to acknowledge the contribution of previous authors of this chapter – the late Corrine Jury, Yutaka Nagai and the late Noriyuki Tatsumi – and of Gareth Ellis, who reviewed the content of this chapter.
Following an informed decision to analyse a blood sample, a specimen must be safely and correctly procured. It is essential to be aware that variation in this pre-analytical phase of the testing process can lead to errors in the analytical phase (see Box 1-1 ).
Pre-collection
- •
Urination within 30 min; food or water intake within 2 h
- •
Smoking
- •
Physical activity (including fast walking) within 20 min
- •
Stress
- •
Drugs or dietary supplement administration within 8 h
During collection
- •
Different times (diurnal variance)
- •
Posture: lying, standing or sitting
- •
Haemoconcentration from prolonged tourniquet pressure
- •
Excessive negative pressure when drawing blood into syringe
- •
Incorrect type of tube
- •
Capillary versus venous blood
Handling of specimen
- •
Insufficient or excess anticoagulant
- •
Inadequate mixing of blood with anticoagulant
- •
Error in patient and/or specimen identification
- •
Inadequate specimen storage conditions
- •
Delay in transit to laboratory
Venous blood is used for most examinations. Capillary blood samples may be satisfactory for some purposes but in general the use of capillary blood should be restricted to children and to some point-of-care screening tests.
Biohazard precautions
Laboratory policies must be in place to ensure that staff who collect blood samples and transfer them to the laboratory minimise the risk of infection from various pathogens during all aspects of specimen handling (see Chapter 24 ). Additional precautions should be taken when handling high-risk specimens (e.g. those from patients suspected of having a viral haemorrhagic fever). In this circumstance, the collection policy should stipulate the use of personal protective equipment, such as disposable gloves, body apron and protective eyewear. Care must be taken to prevent injuries, especially when handling and disposing of needles and lancets. Recommendations for standardising blood collection have been published. ,
Procurement of venous blood
Equipment
It is important to assemble a tray or prepare a workspace that has all the requirements for blood collection ( Box 1-2 ). The selection of needle diameter is a compromise between achieving adequate flow with minimal turbulence and minimising patient discomfort. A 19-gauge (19G) or 21G *
* The International Organisation for Standardisation has established a standard (ISO 7864), which relates the following diameters for the different gauges: 19G = 1.1 mm; 21G = 0.8 mm; 23G = 0.6 mm.
needle is suitable for most adults. A 23G needle is often selected for children. The shaft of the needle should be short (about 15 mm). It may be helpful to collect the blood by means of a winged needle (often referred to as a ‘butterfly’ ) connected to a length of plastic tubing that can be attached to the nozzle of the syringe or to a needle for entering the cap of an evacuated container (see Specimen Containers ).- •
Syringes and needles
- •
Tourniquet
- •
Specimen containers (tubes or evacuated tube system) – plain and with various anticoagulants
- •
Request form
- •
70% isopropanol swabs or 0.5% chlorhexidine
- •
Sterile gauze swabs
- •
Adhesive dressings
- •
Self-sealing plastic bags with a separate compartment for the request form
- •
Rack to hold specimens upright during process of filling (except when an evacuated tube system is used)
- •
Puncture-resistant disposal container
Specimen containers
Containers for testing whole blood are available commercially with dipotassium, tripotassium or disodium ethylenediaminetetra-acetic acid (EDTA) anticoagulant, and often have a mark to indicate the correct amount of blood to be added. Containers are also available containing trisodium citrate, heparin or acid–citrate–dextrose, as well as containers with no additive which are used when serum is required. Design requirements and other specifications for specimen collection containers have been described in a number of national and international standards (e.g., that of the International Council for Standardisation in Haematology ) and the European standard (EN 14820). There is no universal agreement regarding the colours used for identifying containers with different additives so phlebotomists should familiarise themselves with the colours used by their local suppliers.
Evacuated tube systems in common use consist of a glass or plastic tube under a defined vacuum, a needle and a needle holder, which secures the needle to the tube. The main advantage is that the cap can be pierced so that it is not necessary to remove it either to fill the tube or subsequently to withdraw samples for analysis, thus minimising the risk of aerosol discharge of the contents. An evacuated system is useful when multiple samples in different anticoagulants are required. The vacuum controls the amount of blood that enters the tube, ensuring an adequate volume for testing with the correct proportion of any anticoagulant.
Phlebotomy procedure
Staff undertaking this procedure should be adequately trained. The phlebotomist must check that the patient’s identity corresponds to the details on the request form and also ensure that the phlebotomy tray contains all the required specimen containers and other equipment necessary for the procedure.
A tourniquet should be applied just above the intended venepuncture site. Blood is best withdrawn from an antecubital vein or other visible veins of the forearm by means of either an evacuated tube or a syringe. It is recommended that the skin be cleaned with 70% alcohol (e.g., isopropanol) and allowed to dry spontaneously before being punctured. The tourniquet should be released as soon as the vein is punctured and blood begins to flow into the syringe or evacuated tube – delay in releasing the tourniquet leads to fluid shift and haemoconcentration as a result of venous blood stagnation. After the vein has been successfully punctured, the piston of the syringe should be withdrawn slowly with no attempt being made to withdraw blood faster than the vein is filling. Anticoagulated specimens must be mixed by inverting the container several times. The risk of unwanted haemolysis of the specimen can be minimised by using minimal tourniquet time, withdrawing blood carefully, using an appropriately sized needle, delivering the blood slowly into the receptacle and avoiding unnecessary agitation when mixing with the anticoagulant. Note that if blood is drawn too slowly or is inadequately mixed with the anticoagulant some coagulation may occur, rendering the sample unsuitable. After collection, containers must be firmly capped to minimise the risk of leakage.
If blood collection fails, it is important to remain calm, communicate with the patient and consider the possible causes. These include poor technique (e.g., passing the needle through the vein, or poor selection of veins), scarring of tissues and haematoma formation.
After obtaining the necessary specimens, remove the needle and press a sterile swab over the puncture site. Gentle pressure should be applied to the swab with the arm slightly elevated for a minute before checking that bleeding has completely ceased. Finally, the puncture site should be covered with a small adhesive dressing.
Obtaining blood from an indwelling line or catheter is an important potential source of error. It is common practice to flush indwelling lines with heparin, so they must be flushed free from heparin and the first 5 ml of blood must be discarded before any blood is collected for laboratory testing. If intravenous fluids are being transfused into an arm, blood should generally not be collected from that arm; however, if this is essential, the specimen should be obtained from below the intravenous infusion with the tourniquet being placed below the site of infusion.
Postphlebotomy procedure
It is essential that every specimen is labelled with adequate patient identification immediately after the samples have been obtained and at the patient’s bedside. The information should include, as a minimum, surname and forename or initials, hospital number or other unique identifying number, date of birth and date and time of specimen collection. Many centres have adopted automated patient identification using a bar code printed on a wrist or ankle band worn by the patient. If this type of system is used both the specimen label and the request form should be bar-coded with identical data, unless the sample is to be used for blood transfusion tests, in which case the label should be handwritten (see Chapter 22 ).
Specimens should be sent in individual plastic bags separated from the request forms to prevent contamination of the forms in the event of leakage. Samples and form should remain together until the request is registered in the laboratory reception area.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree