Minimally invasive breast biopsies are rapidly replacing open surgical biopsy. Percutaneous breast biopsy can be performed with several possible guidance technologies. Other chapters in this book describe techniques for ultrasound-guided minimally invasive biopsy of lesions detected with ultrasound, and for percutaneous biopsy of palpable breast lesions based upon palpation. Stereotactic breast biopsy is a minimally invasive technique for the sampling of nonpalpable breast lesions detected on mammography.1,2 If the lesion is only visualized on one imaging modality, that modality should be used for guidance during the biopsy procedure. In cases where the lesion is visualized by more than 1 imaging modality, the modality utilized for guiding the biopsy device should be the modality expected to afford the least complicated biopsy. Stereotactic breast biopsy technology was introduced into the United States by Dr. Kambiz Dowlat, a surgeon at Rush University Medical College, in the late 1980s (Fig. 29-1).3
This technology enables the surgeon to consistently obtain sufficient tissue for the pathologist to establish a diagnosis, as well as allowing for the determination of any relevant receptors in malignant lesions.4,5 In contrast to open surgical breast biopsy, stereotactic biopsy takes less time, needs only local anesthetic, requires only a minimal incision without the potential for significant parenchymal and skin scarring, and is more cost- effective. Following stereotactic biopsy, there is essentially no recovery period, and there is no breast deformity at the biopsy site. An additional advantage of stereotactic biopsy over traditional needle localization and open surgical biopsy is that stereotactic biopsy can be performed on a lesion seen in only one mammographic view, in contrast to traditional needle localization, which is only possible for a lesion seen in 2 orthogonal mammographic views. (It is possible to use stereotactic guidance for needle localization of a lesion seen in only 1 mammographic view.)
The term “stereotactic” comes from the same root as the terms “stereophonic” and “stereoscopic.” The word “stereophonic” refers to the presentation of sound from 2 speakers to create the illusion of 3-dimensional sound, and the word “stereoscopic” refers to the presentation of 2 images simultaneously to create the illusion of a 3-dimensional image. Stereotactic breast imaging involves taking 2 digital x-ray images of the breast from different angles and using a computer to analyze the information from these 2 images to reconstruct the location of a breast lesion in 3-dimensional space. The computer then uses the data to help the physician guide a needle to the precise location of the lesion in the breast.
The principle of stereotactic imaging can best be understood by analogy to human vision and depth perception. The basis of experiencing 3-dimensional vision is depth perception. Depth perception gives humans the ability to judge the distance to objects in the visual field. To experience depth perception requires vision in both eyes. The slight difference in the position of the 2 eyes results in a slightly different image being seen by each eye. The brain is able to synthesize these 2 different views into a 3-dimensional reconstruction of the visualized scene. A simple demonstration of the difference between the images seen by the right eye and the left eye is to hold up a finger 1 ft in front of your nose and rapidly alternate between closing the left eye and the right eye. The finger appears to jump from side to side, because its location in each eye’s visual field is different (parallax). Individuals who are blind in 1 eye lack 3-dimensional vision and are handicapped in judging depth or distance.
In stereotactic imaging,6,7 2 mammographic images of the breast are obtained 30 degrees apart (the x-ray tube is first rotated 15 degrees to the right of midline and then 15 degrees to the left of midline). The 2 images are viewed on a monitor, and the physician uses a cursor to select the target lesion on both images. The computer software performs a triangulation function using the selected points on the 2 images to determine the horizontal x, vertical y, and depth z coordinates of the lesion in 3-dimensional space. These coordinates are transmitted to the needle holder, which is moved to the exact position that will place the tip of the biopsy probe at the lesion.
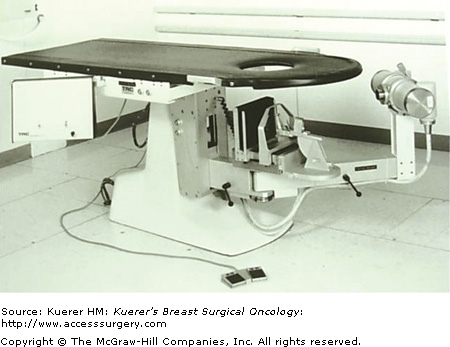
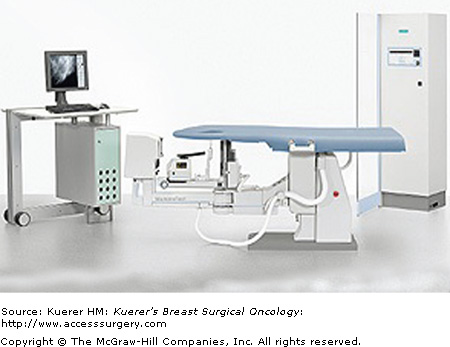
There are 2 targeting systems utilized in stereotactic biopsy equipment. Stereotactic equipment manufactured by Siemens utilizes a polar coordinate system (Fig. 29-2), and equipment manufactured by Hologic utilizes a Cartesian coordinate system (Fig. 29-3). The polar coordinate system defines a target by distances from a fixed point and angular distances from a reference line (Fig. 29-4). The depth of the targeted lesion is determined from the back compression plate. The horizontal and vertical axes are expressed in degrees while the depth of the lesion is in mm.
The Cartesian system defines the exact position of the target lesion in 3-dimensional space in millimeters in 3 axes that intersect at right angles: z (depth), x (horizontal), and y (vertical). The depth is determined from a reference point in front of the breast on the front compression plate (Fig. 29-5). The z-coordinate indicates the depth of the target lesion between the superficial skin surface and the deep skin surface on the opposite side of the compressed breast. A z-value of 0 indicates the level of a reference point on the compression plate in front of the breast (this is the plate constructed with the opening through which the biopsy is performed). The z-value corresponding to the level of the image receptor behind the breast will, by definition, equal the thickness of the compressed breast. For example, if the breast compresses to a thickness of 35 mm, the skin surface through which the biopsy needle enters will have a z-value of 0, and the opposite skin surface, against the image receptor, will have a z-value of 35; a point with a z-value of 45 lies beyond the breast in the image receptor. One should never attempt to biopsy any lesion with a calculated z-value greater that the compression thickness of the breast for 2 reasons. First, if a lesion is real, it cannot lie outside of the breast. Second, extending the biopsy device into the image receptor will damage both the biopsy probe and the back breast support.
Indications for stereotactic breast biopsy are suspicious microcalcifications and masses (or densities) seen on mammography but not identifiable on ultrasound. At many institutions percutaneous core needle biopsy has replaced open surgical biopsy of the breast in the majority of cases. In the future, minimally invasive core needle biopsy promises to become the standard of care for the biopsy of breast lesions.8
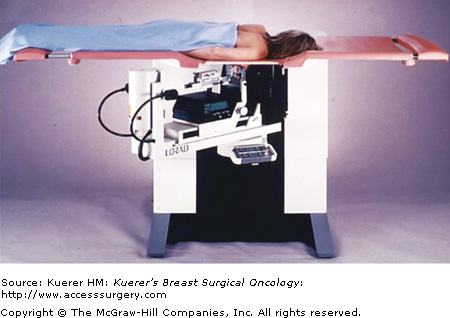
Contraindications for stereotactic biopsy include patient characteristics that make lying prone on the biopsy table for the duration of the procedure (about 45 minutes) impossible, medications that make needle biopsy dangerous, and factors related to individual breast geometry.
Contraindications related to the biopsy table are patient weight greater than the weight limit of the table (currently 300 lb); extreme kyphosis, making it impossible to position the breast deep enough through the hole in the biopsy table; and orthopnea, making it impossible for the patient to lie prone. These factors related to the biopsy table can be overcome by use of a stereotactic biopsy attachment that attaches to an upright mammography unit. These units are less popular than table-mounted dedicated sterotactic biopsy units, but they are less expensive, and are useful in settings where there is not sufficient room available to dedicate to a stereotactic biopsy table (Fig. 29-6).
Contraindications that make an intervention dangerous include bleeding diathesis and anticoagulants such as Plavix (clopidogrel bisulfate) and Coumadin (warfarin sodium). Careful planning for the procedure may include reversing a bleeding disorder, the temporary interruption of anticoagulants, or the substitution of short-acting anticoagulants.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree