Fifteen percent of women treated for breast cancer with total mastectomy receive immediate or early breast reconstruction.1,2 The percentage is higher in young women and those treated in tertiary care medical centers. Immediate breast reconstruction (IBR) has several advantages.3,4 It can prevent some of the negative psychological and emotional sequelae seen with mastectomy. The aesthetic results of immediate reconstruction are superior to those seen after delayed reconstruction. IBR also reduces hospital costs by reducing the number of procedures and length of hospitalization. IBR has the potential to impact the treatment of breast cancer. It could affect the delivery of adjuvant therapy and the detection and treatment of recurrent disease. Chemotherapy and radiation therapy could also impact the complication rates of reconstruction. The oncologic considerations of breast reconstruction are outlined in this chapter.
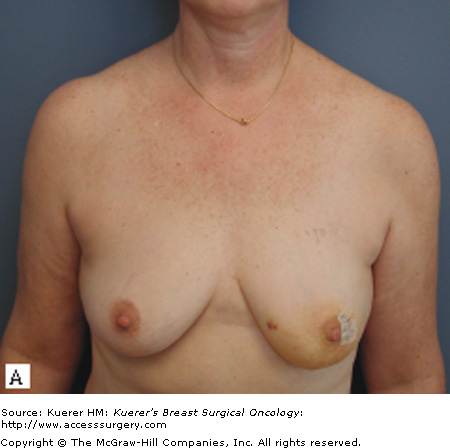
Skin sparing mastectomy (SSM) has markedly improved the aesthetic results of IBR (Fig. 74-1). Preservation of the native skin envelope and the inframammary fold reduces the amount of tissue necessary for reconstruction.5 Breast symmetry can often be achieved without operating on the contralateral breast, and the periareolar incisions are inconspicuous in clothes.
There have been concerns that the skin and inframammary fold preservation reduce the effectiveness of total mastectomy. Despite these concerns, there is a large body of evidence that the local recurrences (LRs) after SSM are comparable to non-SSM.6-8 Care must be taken, however, in patients with superficial cancers or diffuse ductal carcinoma in situ (DCIS) to assure adequate surgical margins. The follow-up of patients after SSM to detect LRs is discussed in the next section.
The role of postreconstruction imaging after the treatment of breast cancer remains controversial. There is a paucity of data that addresses the issue and there no established guidelines.9 The incidence of LR of breast cancer is related to tumor stage. Most LRs after total mastectomy are in the skin and subcutaneous tissue and are readily detected by physical examination.10 A flap or implant could potentially delay the discovery of chest wall recurrences.
Systemic relapse is not inevitable following LR, especially after the treatment of DCIS.11,12 This argues that early detection of LRs may have a potential survival impact. All forms of mastectomy leave residual breast tissue. The differences are in terms of the microscopic breast tissue left behind in the skin and inframammary fold, which are largely preserved after SSM. Torresan et al evaluated residual glandular tissue in the skin flaps that would have been preserved after SSM.13 They found that 60% contained residual glandular tissue, and it correlated with skin flap thickness.
The completeness of mastectomy is important in the treatment of DCIS because most cases of recurrence represent unexcised residual disease. Several authors have reported LR of DCIS treated by SSM and IBR.11,14,15 They found that the majority of LRs were invasive carcinomas. This suggests that postreconstruction mammography can have a role in the early detection of recurrences prior to the development of invasive carcinoma. Physical examination of implant reconstruction is relatively easy. There is minimal soft tissue covering the implant except along the inframammary fold and in the axillary tail. Deep chest wall recurrences are extremely unlikely because the implants are placed in the submuscular plane. Conventional mammographic evaluation has limited utility because the implants obscure soft tissue visualization. Magnetic resonance imaging (MRI), which has been used extensively to evaluate the integrity of silicone gel implants, may have a role in the selective surveillance after implant reconstruction.16-19
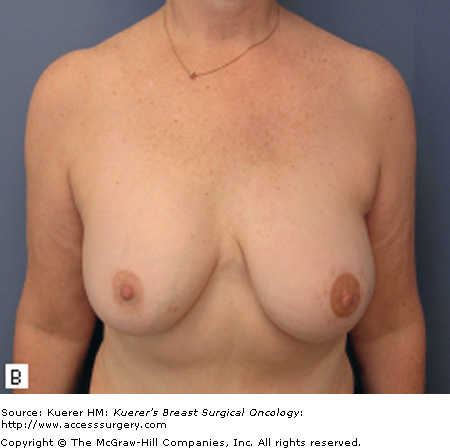
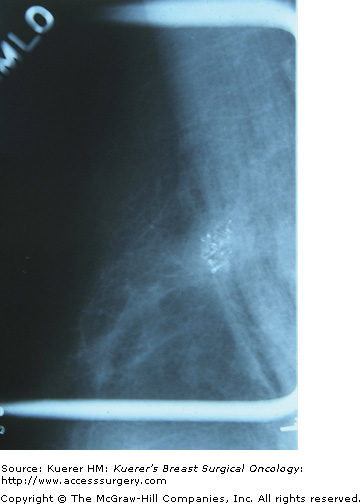
The sensitivity of physical examination of autologous reconstruction is lower than that seen with implant reconstruction. Deep chest wall recurrences often avoid detection until symptoms develop. Autologous reconstruction causes less impairment of mammographic tissue visualization.20 Benign mammographic findings after transverse rectus abdominis musculocutaneous (TRAM) flap reconstruction include fat necrosis, lipid cysts, calcifications, lymph nodes, and epidermal inclusion cysts (Fig. 74-2).21 Breast cancer recurrences in autologous tissue reconstruction are mammographically similar to that of primary tumors (Fig. 74-3).22,23 Proponents of surveillance mammography believe that screening breast cancer patients with autologous reconstructions can detect nonpalpable recurrences before clinical examination.
Helvie et al evaluated surveillance mammography in 113 patients after TRAM flap reconstruction.24 Six patients underwent biopsy for suspicious mammographic findings, and 2 LRs were detected. Two patients in the study group went on to develop recurrences that were detected by physical examination. There was one false-negative mammogram resulting in a sensitivity of 67% and specificity of 98% for surveillance mammography after TRAM flap reconstruction.
There is a paucity of data regarding the efficacy of MRI of the breast following autogenous breast reconstruction.25,26 Breast MRI has been shown to clearly delineate autogenous flaps from residual mammary adipose tissue. The absence of contrast medium uptake during breast MRI precludes recurrent carcinoma to a high probability. Fat necrosis in a TRAM flap will show early postoperative contrast enhancement, but this resolves within 6 to 12 months. Rieber et al evaluated MRI of the breast in the follow-up of 41e patients who had undergone autogenous tissue breast reconstruction.27 MRI was able to distinguish flaps from surrounding residual breast tissue in all cases. It excluded disease recurrence in 4 patients with suspicious mammographic or sonographic findings. It returned false-positive findings in 3 cases.
The potential indications for postreconstruction imaging include patients with close surgical margins and patients with diffuse DCIS treated by SSM. Its routine use after autologous reconstruction after SSM for invasive carcinoma warrants further study. The low detection rate and specificity does not justify the routine use of MRI in the follow-up of patients postreconstruction. MRI is most useful in patients with abnormal findings on physical examination or mammography and ultrasound. It is also helpful to delineate the extent of local disease recurrence.
There are concerns that IBR may delay the administration of adjuvant chemotherapy. A survey of 376 consultant breast surgeons in the United Kingdom and Ireland found that the majority (57%) preferred delayed reconstruction because of these concerns.28 Breast reconstruction does have a high complication rate especially in patients who are obese, smoke tobacco, or have a history of chest wall irradiation. Alderman et al performed a multi-institutional study of complication rates after tissue expander or TRAM flap reconstruction.29 They reported a 52% complication rate, with major complications occurring in 30% of patients.
It seems logical that the high complication rate of IBR could potentially delay the administration of adjuvant therapy. Studies comparing onset of chemotherapy after IBR and control group treated with mastectomy alone have failed to show significant differences.30-32 Wound complications after IBR must be treated aggressively to remove necrotic, potentially infected tissue. Patients with clean, open wounds can receive chemotherapy with minimal compromise in wound healing. These patients must be followed closely to detect early signs of infection.
Patients with locally advanced, stage III breast cancer are generally treated with chemotherapy followed by total mastectomy and adjuvant radiation. The 5-year survival is 50% to 80%, and patients with a poor response to chemotherapy have an especially bad prognosis. It may be preferable to delay reconstruction until after mastectomy and adjuvant radiation in these patients. This avoids the potential problems with radiation delivery and the adverse effects of postmastectomy radiation therapy on immediate reconstruction. These issues are discussed in detail in another chapter.
Neoadjuvant chemotherapy has not been shown to increase the complication rate of IBR. Deutsch et al reported a 55% complication rate in 31 patients after immediate TRAM flap reconstruction who received neoadjuvant chemotherapy.33 Six percent had a delay in resumption of chemotherapy because of complications. Sultan et al found a 14% complication rate in 21 patients who received neoadjuvant chemotherapy and underwent IBR.34 The mean interval between surgery and resumption of chemotherapy was 19 days, and there was no delay in any patients.
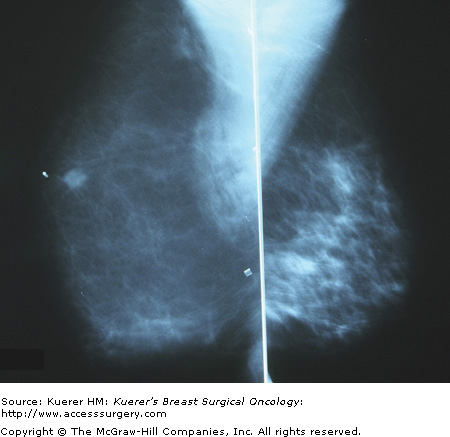
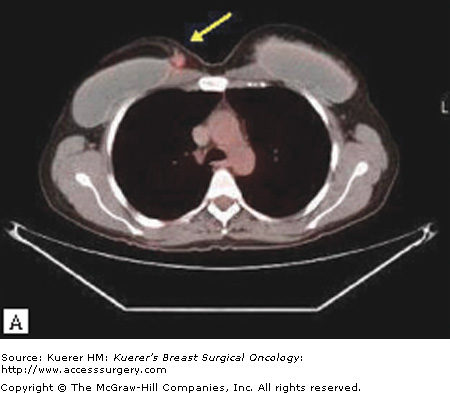
Surgical options following LR after breast reconstruction depend on the location and number of metastatic deposits and previous treatment. Imaging of the reconstructed breast and body scans are necessary to delineate the extent of tumor involvement (Fig. 74-4). Isolated LRs can be treated with removal of as much reconstructed tissue as necessary to achieve negative margins. Adjuvant chest wall radiation is usually administered (Fig. 74-5).