Table 10-1 Comparison of “Old” and “New” Staging for Endometrial Carcinoma* | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Staging and Issues Related to Staging of Endometrial Carcinoma
Staging and Issues Related to Staging of Endometrial Carcinoma
Anna Sienko MD
The accurate evaluation of hysterectomy specimens resected for endometrial carcinoma is crucial for the accurate staging of the tumor. Tumor staging impacts patient care directly as the main basis for selection of treatment options and prognosis. The most important factors that have to be assessed by histologic examination, besides classification of tumor cell type and tumor nuclear grade, are the depth of tumor invasion of myometrium, involvement of the cervix, and lymphovascular space invasion.
In 2009, the staging system for endometrial carcinoma was revised on evidence-based data that showed that stage IA, grade 1 or 2, endometrial carcinoma and stage IB, grade 1 or 2, endometrial carcinoma had a similar 5-year survival rate. Based on these findings, the International Federation of Gynecology and Obstetrics (FIGO) committee recommended that these two stages be combined into the new stage IA, which now comprises only endometrial involvement by tumor and/or less than 50% of myometrial invasion, and stage IB, which has ≥50% of myometrial invasion (Table 10-1).1,2 The new staging also merged stage IIA and stage IIB (tumor limited to glandular epithelium of endocervix with no evidence of stromal invasion and invasion of endocervical stroma, respectively) into stage II (invasion of endocervical stroma without extension beyond the uterus). Therefore, endocervical glandular involvement in the new staging does not upstage the tumor to stage II. An additional change in the new staging system is that positive cytology of ascites or peritoneal washings is not included in the staging and does not alter the stage; however, the findings should be included in the pathology report.3 Issues concerning staging are discussed in this chapter.
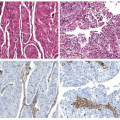
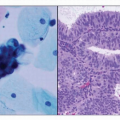
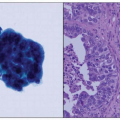
HISTOLOGY
One of the issues that arises in pathologic staging of resected specimens is related to histopathologic assessment of tumor grade and tumor cell type, with several grading systems that have been proposed including use of special stains.4 Generally, it has been accepted that in histologic grading of endometrial carcinomas, high nuclear grade that is inappropriate for the architectural grade raises the overall grade of a tumor to the next highest grade (e.g., architectural grade 2 with nuclear grade 3 results in an overall grade of 3). Serous carcinomas, clear cell carcinomas, and carcinosarcomas (Mixed Müllerian Tumor) are all considered high-risk tumors and considered to be grade 3. This topic is discussed in greater detail in Chapter 4.