Glandular Cell Abnormalities in Pap Tests
Ognjen Kosarac MD
Dina Mody MD
The Papanicolaou (Pap) smear/test is a screening test for cervical squamous cell carcinoma and its precursors. It is not and was never meant to be a screening test for endometrial cancer or its precursors. Based on published data, only about half of Pap smears/tests prior to the histologic diagnosis of endometrial cancers show any significant abnormal findings. However, endometrial carcinomas and hyperplasias may shed cells or bleed, and this may be picked up on a Pap test. Hence, every attempt should be made to identify these on Pap tests and report them using consistent terminology. The 2001 Bethesda System does just that, and the details follow below.
ENDOMETRIAL CELLS IN PAP TESTS
Benign-appearing endometrial glandular cells are seen in exfoliative gynecologic preparations obtained from premenopausal women during the first half of the menstrual cycle (cutoff day 10 to 14).1,2 A small association of benign endometrial cells with endometrial neoplasia has been found, according to some authors in the range of 1% to 11%.3,4,5 and 6 Because the endometrial carcinomas mostly occur in postmenopausal women, the presence of benign endometrial cells in Pap tests in those women warrants further follow-up. It is also known that the sensitivity of the Pap test for endometrial carcinoma is low.7 The most current reporting system, the 2001 Bethesda System, recommends reporting benign/normal endometrial cells in women aged 40 years or older.
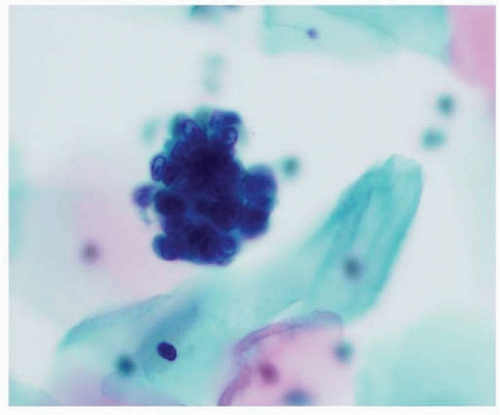
Exfoliated endometrial cells occur in ball-like clusters and rarely as single cells. Abraded endometrial cells and fragments from the lower uterine segment and stromal and histiocytic cells should not be reported because they are not associated with endometrial pathology. In the first half of the menstrual cycle, endometrial cells often have a double contour, with glandular cells surrounding a core of stromal cells (“exodus” pattern; Fig. 11-1). Endometrial cell nuclei are about the size of an intermediate cell nucleus and are either round or bean-shaped. The chromatin pattern may be difficult to discern in the cell groups, but nucleoli are usually inconspicuous, and nuclei may be degenerated. Cytoplasm is scant, basophilic, and occasionally vacuolated. Cell borders are ill defined, and the cells frequently appear to be packed together. The background is often bloody and may contain histiocytes and endometrial stromal cells. In liquid-based preparations, three-dimensional cell clusters are common, with the plane of focus often above the plane of the normal squamous cells (Fig. 11-2). Single cells may be more commonly seen, and the background is usually cleaner with less blood. Nuclear chromatin detail may be more easily discerned, and single-cell necrosis (apoptosis) is common within exfoliated cell groups.8
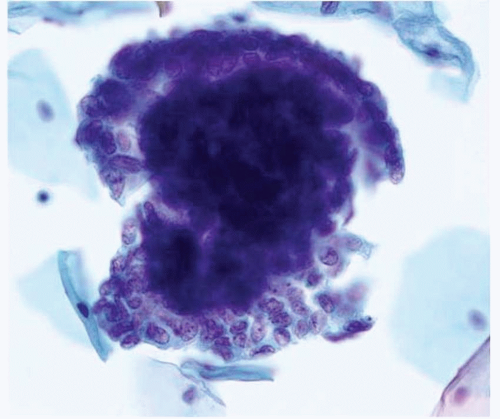 FIGURE 11-1: Exodus pattern. Three-dimensional group with central, dark endometrial cells surrounded by paler glandular cells. |
EPITHELIAL CELL ABNORMALITIES IN PAP TESTSGLANDULAR CELL TYPE
The glandular cell abnormalities on Pap tests are divided into endocervical, endometrial, or generic glandular cells if one cannot tell with certainty if the cells are endocervical or endometrial in origin. For the purposes of this chapter, only endometrial cell abnormalities will be discussed.
Atypical Endometrial Cells
Atypical endometrial cells generally occur in small groups, with 5 to 10 cells in each group (Fig. 11-3). In contrast to normal endometrial cells, nuclei are slightly enlarged with mild hyperchromasia and more prominent nucleoli. Cell borders are usually ill defined,
and cytoplasm may be vacuolated.8 Atypical cells may be associated with dysfunctional uterine bleeding, use of an intrauterine device, endometrial polyps, endometrial hyperplasia, or endometrial adenocarcinoma.9 Several studies addressed the incidence of atypical endometrial cells in cervicovaginal smears (Table 11-1).4,10,11,12,13,14,15,16,17 and 18 Cherkis et al.4 showed a prevalence rate of atypical endometrial cells of 1 in 1,700 from a screening pool of 300,000 smears, resulting in a frequency of 0.06%. Another study found atypical endometrial cells in 5 (6.2%) of 81 cervicovaginal smears with a diagnosis of atypical glandular cells of undetermined significance (AGUS), and 40% (2 of 5 cases) had a significant uterine lesion on follow-up.10 More recently, Chhieng et al.17 reported atypical endometrial cells in 5.25% of smears with a diagnosis of AGUS or in 0.03% of all smears. In their study, 31% of patients with histologic follow-up had a significant uterine lesion.
Saad et al.,18 in their study, demonstrated an AGUS rate of 0.34%, and 40% of patients with atypical glandular cells, favoring endometrial origin, had significant uterine lesions on histologic follow-up.
and cytoplasm may be vacuolated.8 Atypical cells may be associated with dysfunctional uterine bleeding, use of an intrauterine device, endometrial polyps, endometrial hyperplasia, or endometrial adenocarcinoma.9 Several studies addressed the incidence of atypical endometrial cells in cervicovaginal smears (Table 11-1).4,10,11,12,13,14,15,16,17 and 18 Cherkis et al.4 showed a prevalence rate of atypical endometrial cells of 1 in 1,700 from a screening pool of 300,000 smears, resulting in a frequency of 0.06%. Another study found atypical endometrial cells in 5 (6.2%) of 81 cervicovaginal smears with a diagnosis of atypical glandular cells of undetermined significance (AGUS), and 40% (2 of 5 cases) had a significant uterine lesion on follow-up.10 More recently, Chhieng et al.17 reported atypical endometrial cells in 5.25% of smears with a diagnosis of AGUS or in 0.03% of all smears. In their study, 31% of patients with histologic follow-up had a significant uterine lesion.
Saad et al.,18 in their study, demonstrated an AGUS rate of 0.34%, and 40% of patients with atypical glandular cells, favoring endometrial origin, had significant uterine lesions on histologic follow-up.
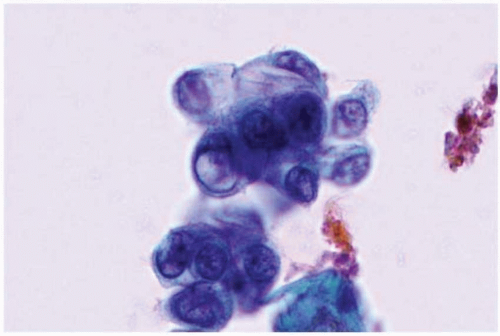 FIGURE 11-3: Atypical endometrial cells. Small clusters of cells with slightly enlarged nuclei, more prominent nucleoli, and occasionally vacuolated cytoplasm. |
Table 11-1 AGUS Reporting Rates and Follow-up with a Significant Uterine Lesion (%) | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|