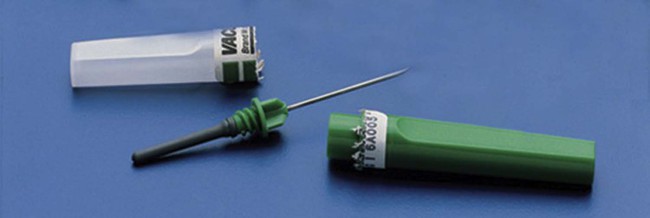
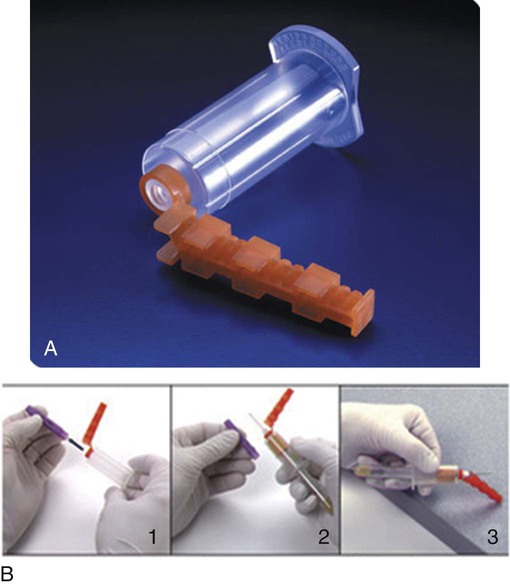
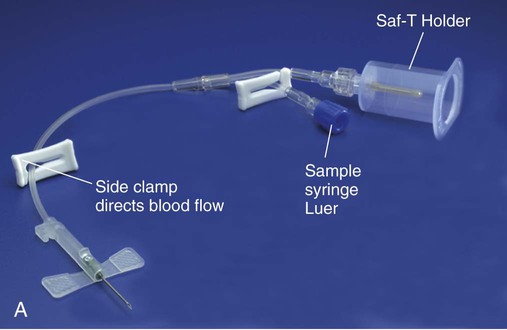
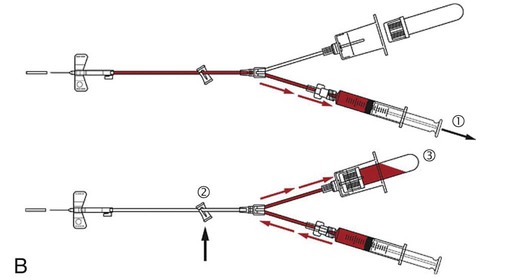
After completion of this chapter, the reader will be able to: 1. Describe the application of standard precautions to the collection of blood samples. 2. List collection equipment used for venipuncture and skin puncture. 3. Correlate tube stopper color with additive, if any, and explain the purpose of the additive and use of that tube type in the laboratory. 4. Discuss selection of a vein for venipuncture and name the vein that is preferred in most instances. 5. List in order the steps recommended by the Clinical and Laboratory Standards Institute for venipuncture in adults, including recommended order of collection for tubes with various additives. 6. Discuss complications encountered in blood collection and proper response of the phlebotomist. 7. Explain appropriate use of skin puncture equipment and procedure to be followed, including venipuncture sites for infants, children, and adults. 8. Discuss essentials of quality assurance in specimen collection. 9. List reasons for specimen rejection. 10. Given the description of a specimen and its collection, determine specimen acceptability. 11. Recognize deviations from the recommended venipuncture practice in a written scenario and describe corrective procedures. 12. Name the most important step in the venipuncture procedure. 13. List reasons for inability to obtain a blood specimen. 14. Summarize legal issues that need to be considered in specimen acquisition. Standard precautions must be followed in the collection of blood, and all specimens must be treated as potentially infectious for bloodborne pathogens (e.g., hepatitis B virus, hepatitis C virus, and human immunodeficiency virus [HIV]). Regulations of the Occupational Health and Safety Administration (OSHA) that took effect on March 6, 1992, outlined in detail what must be done to protect healthcare workers from exposure to bloodborne pathogens, such as the pathogens that cause hepatitis C, hepatitis B, hepatitis D, syphilis, malaria, and HIV infection.1 Bloodborne pathogens may enter the body via an accidental injury by a sharp object, such as a contaminated needle, a scalpel, broken glass, or anything else that can pierce the skin. Cuts, skin areas with dermatitis, abrasions, and mucous membranes of the mouth, eyes, and nose may provide a portal of entry. Indirect transmission can occur when a person touches a contaminated surface or object and then touches the mouth, eyes, nose, or nonintact skin without washing the hands. Hepatitis B virus can survive on inanimate or dried surfaces at room temperature for at least 1 week.2 Handwashing is the most important practice to prevent the spread of infectious diseases. The phlebotomist should wash his or her hands with a nonabrasive soap and running water between patients and every time gloves are removed. If handwashing facilities are unavailable, an antiseptic hand cleanser or an antiseptic towelette may be used as a temporary measure. Gloves are essential protective equipment and must be worn when venipunctures are performed. When gloves are removed, it is important that no substances from the soiled gloves come in contact with the hands. Glove removal is covered in detail in Chapter 2. Contaminated sharps and infectious wastes should be placed in designated puncture-resistant containers. The red or red-orange biohazard sign (see Figure 2-2) indicates that a container holds potentially infectious materials. Biohazard containers should be easily accessible and should not be overfilled. Certain physiologic factors specific to the patient may affect results of laboratory testing. These factors include posture (supine or erect), diurnal rhythms (day or night), exercise, stress, diet (fasting or not), and smoking (Box 3-1).3–5 It is important that the phlebotomist adhere to requests for specimens to be drawn at a specific time and record the time of collection. Although there are several manufacturers of evacuated tubes in the United States all follow a universal color code in which the stopper color indicates the type of additive contained in the tube. Figure 3-1 provides a summary of collection tube types. Sterile needles come in a variety of lengths and gauges (bore or opening size). Needles are made to be screwed into the evacuated tube holder or to be attached to the tips of syringes. Evacuated tube needles are double pointed and have a long, narrow, pointed end that punctures the patient’s skin and is covered by a plastic cap, and a short beveled point at the other end that punctures the rubber stopper of the evacuated tube and is covered by a rubber sleeve. The rubber sleeve prevents blood from dripping into the holder when tubes are changed (Figure 3-2). On syringes, “single-sample” needles are used. The end of the needle that is inserted into the vein has a point with a slanted side (bevel), which must be facing up when the needle is inserted. Needle tips should be examined for burrs or bends before a venipuncture is performed. Gauge numbers are related inversely to the bore size: the smaller the gauge number, the larger the bore. Needle gauges for drawing blood range from 20 gauge to 25 gauge. The most common needle size for adult venipuncture is 21 gauge with a length of 1 inch. The advantage of using a 1-inch needle is that it provides better control. Several new needles and holders have been designed to comply with the revised Occupational Exposure to Bloodborne Pathogens Standard (effective April 18, 2001) and its requirement for implementation of safer medical devices. These needle holders have safety features to prevent the possibility of needle sticks. Needle holders are made to fit a specific manufacturer’s needles and tubes and, for best results, should not be interchanged. The holders are disposable and must be discarded after a single use with the needle still attached as per OSHA requirements.6 Examples of these needles and holders are the following: 1. The Vacutainer Eclipse Blood Collection System (Becton, Dickinson and Company, Franklin Lakes, N.J.) allows single-handed activation after the venipuncture is performed by pushing the safety shield forward with the thumb until an audible click is heard. The Becton Dickinson Eclipse needle should be used with a single-use tube holder. After the safety shield is activated, the entire assembly should be discarded intact into the sharps container. 2. The Jelco multisample blood collection needle used with the Venipuncture Needle-Pro Device (Smiths Medical ASD, Norwell, Mass.) allows the Needle-Pro sheath to be snapped over the needle by pushing it against a flat, firm surface after the venipuncture is completed. The entire device is disposed of into the sharps container (Figure 3-3). 3. Greiner Bio-One (Monroe, N.C.) offers the VACUETTE QUICKSHIELD, which has a sheath that locks into place after use, and the QUICKSHIELD Complete PLUS, a system that incorporates a holder with the VACUETTE Visio PLUS multisample needle attached. The flash window in the needle hub indicates when a successful venipuncture has been achieved (Figure 3-4). A butterfly is an intravenous device that consists of a short needle and a thin tube with attached plastic wings (Figure 3-5). The butterfly can be connected to evacuated tube holders, syringes, or blood culture bottles with the use of special adapters. Butterflies are useful in collecting specimens from children or other patients from whom it is difficult to draw blood. Butterflies now come with resheathing devices to minimize the risk of needle stick injury (e.g., MONOJECT ANGEL WING Blood Collection [Covidien, Mansfield, Mass.], Vacutainer brand SAFETY-LOK and Vacutainer Push Button Blood Collection Set [Becton Dickinson], and VACUETTE Safety Blood Collection Set [Greiner Bio-One]). Syringes consist of a barrel that is graduated in milliliters and a plunger. Syringe needles have a point at one end and an open hub at the other end that attaches to the barrel. Syringes come with different types of needle attachments and in different sizes. It is important to attach the needle securely to the syringe to prevent air from entering the system. Syringes may be useful in drawing blood from pediatric, geriatric, or other patients with tiny, fragile, or “rolling” veins that would not be able to withstand the vacuum pressure from evacuated tubes. With a syringe, the amount of pressure exerted is controlled by the phlebotomist. Syringes may also be used with winged infusion sets. If only one tube of blood is needed, the syringe needle is shielded, removed, and discarded in a sharps container, and a syringe blood transfer device (Becton Dickinson) or Saf-T Holder with male Luer adapter (Smiths Medical ASD) is attached to the syringe and a vacuum tube is inserted into the transfer device. The blood is transferred from the syringe into the tube using the tube’s vacuum (Figure 3-6).
Specimen Collection*
Safety
Physiologic Factors Affecting Test Results
Venipuncture
Collection Equipment for Venipuncture
Tourniquet
Collection Tubes
Needles
Needle Holders
Winged Infusion Sets (Butterflies)
Syringes
Specimen Collection