(1)
Department of Pathology Beckley Veterans Medical Center (West Virginia), McGuire Veterans Medical Center, Virginia Commonwealth University, Richmond, VA, USA
Key Morphological Features of Low-Grade Fibromyxoid Sarcoma
Alternating fibrous and myxoid areas
Random or whorled growth pattern (Figs. 2.1 and 2.2)
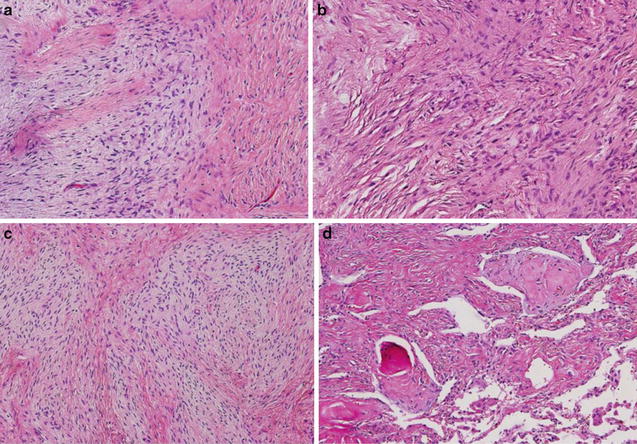
Fig. 2.1
Fibromyxoid sarcoma showing alternating fibrous and myxoid areas (American Journal of Surgical Pathology, Wolters Kluwer/Lippincott Williams & Wilkins, 2011 with permission)
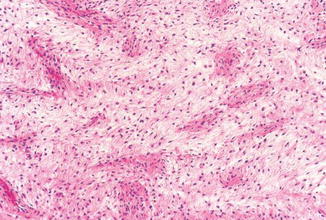
Fig. 2.2
Fibromyxoid sarcoma with random or whorled growth pattern and perivascular condensation (Enzinger & Weiss’s Soft Tissue Tumors, Elsevier/Saunders, 2008 with permission)
Discussion
Typically the tumor presents as well-circum-scribed masses even though microscopic infiltration into the adjacent tissue is frequently present. Many cases of low-grade fibromyxoid sarcoma are located in the skeletal muscles indicating a possible derivation from the fibroblasts in the muscle associated fascia. As discussed in the skin and kidney sections, fibroblast heterogeneity is likely to a universal phenomenon as each tissue or organ has its unique mechanical and functional needs [1, 2].
In fact, the tumor is composed of bland spindle cells with low mitotic figures and no necrosis. The spindle cells are arranged in an alternating fibrous and myxoid pattern. The fibrous areas resemble the distribution of normal fibroblasts in the normal endomysium, whereas the myxoid areas correspond to the spaces occupied by muscle fibers in a muscle bundle. Ultrastructurally, the tumor cells show perineurial and myofibroblastic differentiation [3, 4]. Many cases are positive for EMA and cytokeratins [5, 6].
Differential Diagnosis
Myxoid Neurofibroma and Perineuroma
Myxoid neurofibroma cells are more spindly and wavy. The tumor cells are diffusely S100 positive. Perineuriomas typically lack myxoid areas, and the tumor cells are diffusely SMA positive.
Nodular Fasciitis
Nodular fasciitis is characterized by tissue culture fibroblasts, cleftlike spaces, and extravasation of red blood cells as well as a rapid clinical course.
Myxofibrosarcoma, Malignant Peripheral Nerve Sheath Tumor
Myxofibrosarcomas typically occur in the subcutaneous tissue in the old. The cells are more atypical and present in a uniform myxoid stroma.
Malignant peripheral nerve sheath tumor cells are more elongated and wavy. They are arranged in hypercellular fascicles and sheets.
Myxoma, Myxoid Liposarcoma, and Spindle Cell Liposarcoma
Myxomas lack the alternating fibrous and myxoid pattern as well as plexiform vessels. Myxoid and spindle cell liposarcomas have lipoblasts and lipoid background.
Myxoid DFSP
Dermatofibrosarcoma protuberans presents in superficial locations and contains storiform arrangement of spindle cells which show CD34 positivity.
Key Morphological Features of Myxofibrosarcoma
Multinodular pattern of spindle or stellate cells
Diffuse Myxoid stroma with curvilinear vessels (Figs. 2.3, 2.4, and 2.5)
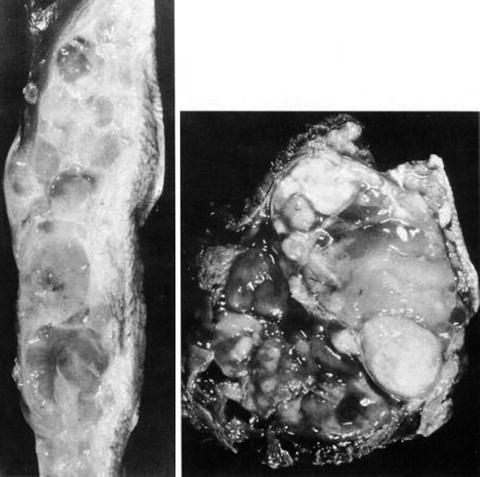
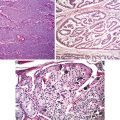
Fig. 2.3
Myxofibrosarcoma. Multinodular growth pattern (Enzinger & Weiss’s Soft Tissue Tumors, Elsevier/Saunders, 2008; American Journal of Surgical Pathology, Wolters Kluwer/Lippincott Williams & Wilkins, 1996 with permission)
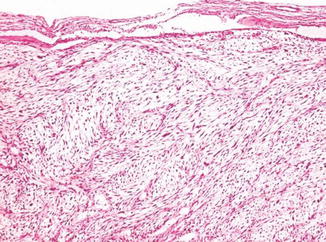
Fig. 2.4
Myxofibrosarcoma. Bland spindle or stellate cells (Enzinger & Weiss’s Soft Tissue Tumors, Elsevier/Saunders, 2008 with permission)
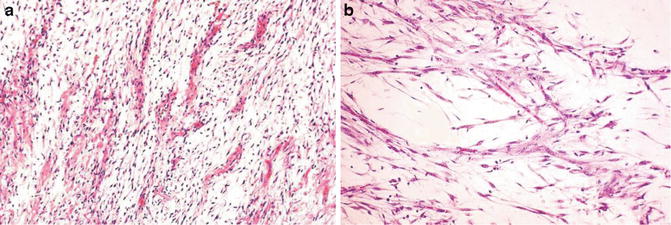
Fig. 2.5
Myxofibrosarcoma. Curvilinear vessels with perivascular condensation of tumor cells and myxoid stroma (Enzinger & Weiss’s Soft Tissue Tumors, Elsevier/Saunders, 2008 with permission)
Discussion
Myxofibrosarcomas typically present in the subcutaneous tissue in the extremities of the elderly and manifest as vague nodules composed of spindle cells distributed in a myxoid stroma. In this myxoid background, elongated curvilinear capillaries are prominent. The tumor cells are frequently CD34 positive and show tendency to perivascular condensation. It is thus indicated that the tumor cells are probably related to the vascular adventitial cells [7, 8]. At ultrastructural level, myofibroblastic differentiation is evident [6].
Differential Diagnosis
Nodular Fasciitis
Nodular fasciitis has tissue culture-like fibroblastic and myofibroblastic proliferation. Although mitotic figures are readily evident, there is no cytological atypia. In addition, there are slitlike spaces, extravasation of red blood cells, and keloid-like collage bundles.
Myxoid Liposarcoma
The tumor cells are more ovoid and the capillaries are more developed in myxoid liposarcoma. The tumor is usually deep seated and contains characteristic lipoblasts.
Myxoma, Nerve Sheath Myxoma, Myxoid Chondrosarcoma
Myxomas show less cellular atypia and mitotic activity and lack typical curvilinear vessels and perivascular condensation.
Myxoid chondrosarcomas also lack curvilinear capillaries. The tumor cells are round. The stroma is more chondroid with prominent hemorrhage.
Fibromyxoid Sarcoma
See differential diagnosis for fibromyxoid sarcoma.
Key Morphological Feature of Dermatofibrosarcoma Protuberans
Monomorphic slender cells in a storiform pattern
Diffuse infiltrative border (Figs. 2.6 and 2.7)
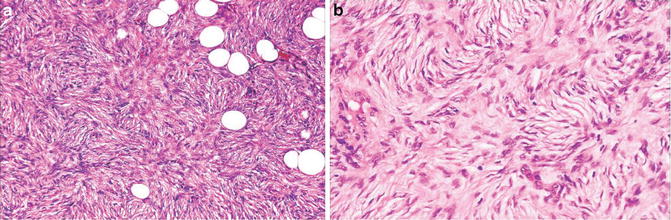
Fig. 2.6
Dermatofibrosarcoma protuberans. Monomorphic spindle cells in a storiform pattern (Enzinger & Weiss’s Soft Tissue Tumors, Elsevier/Saunders, 2008 with permission)
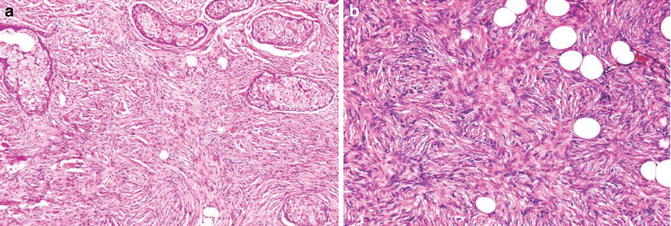
Fig. 2.7
Dermatofibrosarcoma protuberans. Infiltrative pattern (Enzinger & Weiss’s Soft Tissue Tumors, Elsevier/Saunders, 2008 with permission)
Discussion
Whereas benign fibrohistiocytoma is related to the XIII- and CD10-positive dermal fibroblasts, dermatofibrosarcoma protuberans is derived from the CD34-positive dermal fibroblasts which manifest perineurial differentiation. The characteristic cartwheel (storiform) arrangement of tumor cells probably reflects the inherent cellular property to form a 3D mesh-like immunological barrier for the dermis.
Also included in the intermediate malignancy category of fibrohistiocytic tumors are angiomatoid fibrohistiocytoma and plexiform histiocytoma [9, 10]. The former actually represents a tumor of the lymph node stromal cell with characteristic cystic areas and chronic inflammatory infiltration. The intimate relationship between the fibroblasts and histiocytic cells in plexiform histiocytoma is different from that seen in most of other fibrohistiocytomas. Instead of having an admixture of both cellular components, the tumor is featured by nodules of histiocytic cells surrounded by fibroblastic fascicles.
Differential Diagnosis
Benign Fibrohistiocytoma
Typical benign fibrohistiocytomas are composed of admixed fibroblasts and xanthoma-like histiocytes with entrapped collagen and hemosiderin. This admixture indicates a unique relationship between these two phenotypic different cell types (through differentiation or attraction). The fibroblastic component is arranged in short, crisscrossing short fascicules. Multinucleated cells, chronic inflammatory cells, as well as cystic hemorrhage and associated changes are common features. Tentacular extensions can be seen at deep margin, but is focal.
Deep fibrohistiocytomas, however, are more cellular. Not only can they manifest a focal storiform pattern; there are also increased mitotic activities (up to 10/10HPF), a zone of necrosis, and even fat infiltration. In this case, immunostaining for factor XIII, CD10, and CD34 is very helpful in making the distinction.
Neurofibroma
The diffuse form of neurofibroma usually has areas showing neural differentiation. It lacks a storiform growth pattern, an infiltrative border, as well as high cellularity, mitotic index.
Key Morphological Features of Desmoid-Type Fibromatosis
Bland-looking spindle cells in longitudinal fascicles in a nodular growth pattern
Infiltrative border (Figs. 2.8 and 2.9)
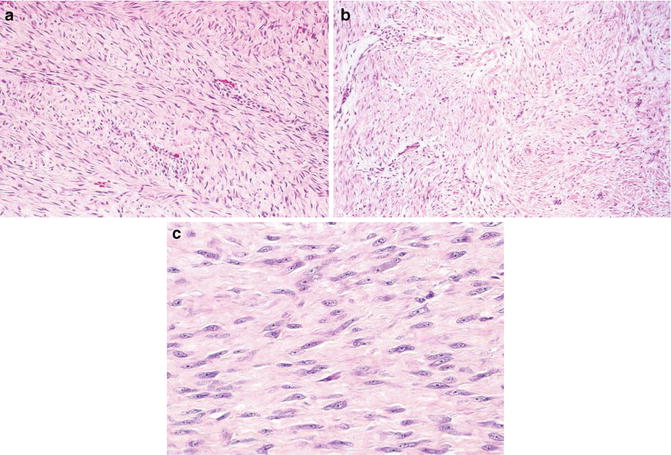
Fig. 2.8
Fibromatosis. Bland spindle cells in longitudinal fascicles (Enzinger & Weiss’s Soft Tissue Tumors, Elsevier/Saunders, 2008 with permission)
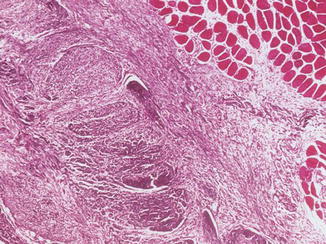
Fig. 2.9
Fibromatosis. Infiltrative border (Enzinger & Weiss’s Soft Tissue Tumors, Elsevier/Saunders, 2008 with permission)
Discussion
Deep fibromatosis has characteristic somatic beta-catenin or adenomatous polyposis coli (HPC) mutations which allow intranuclear accumulation of beta-catenin with resultant cell proliferation [11]. This important feature can be diagnostically useful.
Deep fibromatosis appears to be a tumor of the fibroblasts in the deep fascia. The typical long sweeping fascicules are composed of bland fibroblasts and are less cellular with less defined cell borders than the V-shaped fascicules characteristic of fibrosarcoma. These differences are probably a reflection of the different mechanical stresses in which fascia and tendons are programmed to withstand. Deep fascia tissue binds the muscle tissue with the adjacent tissue, and in doing so, it diffuses mechanical stress over a large area. Long sweeping fascicules are more suitable than herringbone-like structures for this purpose. The main function of a tendon is to concentrate the force generated by skeletal muscle tissue and transmit it to the bone. A V-shaped pattern seems to suit the purpose.
Differential Diagnosis
Reactive Fibroblastic/Myofibroblastic Lesions
The reactive lesions have less regularity in the arrangement of spindle cells and lack an infiltrative border. Frequently, they show focal hemorrhage and hemosiderin deposition.
Fibrosarcoma
Fibrosarcoma has become a rare diagnosis and one of exclusion. Typically it is composed of uniform spindle cells in a distinctive herringbone pattern. The nuclei are hyperchromatic with frequent overlapping.
Solitary Fibrous Tumor
Solitary fibrous tumor has the classical patternless pattern and high cellularity as well as hemangiopericytoma-like areas. The tumor cells are CD34 positive.
Desmoplastic Fibroma of Bone
Radiological information indicating the location in a bone is most helpful as it shares the morphological features with fibromatosis.
Morphological Features of Well-Differentiated Rhabdomyosarcoma
Diffuse spindle cell lesion
Presence of rhabdomyoblasts (Figs. 2.10 and 2.11)
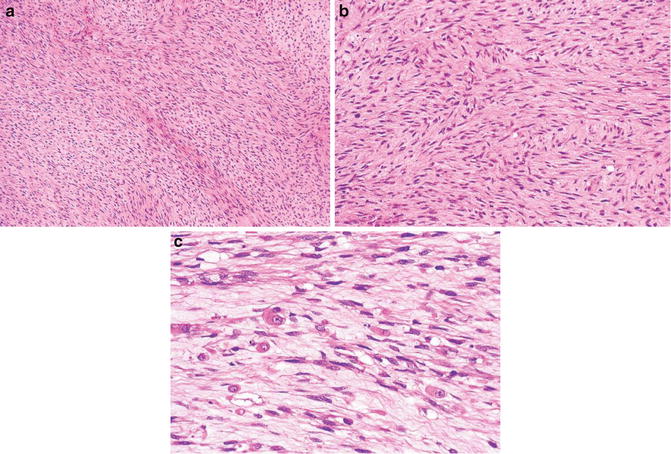
Fig. 2.10
Rhabdomyosarcoma. Spindle cells (a, b). Rhabdoblasts (c) (Enzinger & Weiss’s Soft Tissue Tumors, Elsevier/Saunders, 2008 with permission)
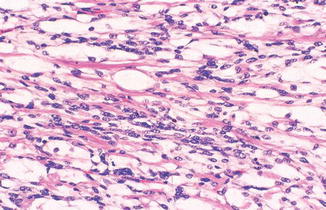
Fig. 2.11
Rhabdomyosarcoma. Rhabdoblasts (Enzinger & Weiss’s Soft Tissue Tumors, Elsevier/Saunders, 2008 with permission)
Discussion
Primarily a pediatric sarcoma, rhabdomyosarcomas are far more common than rhabdomyomas. One unique feature of the sarcoma is that it often arises at sites where skeletal muscle is not a normal component or only scant.
In an analogy to lipogenesis, rhabdomyogenesis is a complex multistage process during which dramatic metamorphogenesis occurs. Stuck at various differentiation stages as a result of botched execution of the metamorphogenic drama. Low-grade rhabdomyosarcoma includes the spindle cell and botryoid variants which bear resemblance to late-stage fetal myoblasts [12, 13].
In low-grade rhabdomyosarcoma (to some extent, embryonal variant also), identification of rhabdomyoblasts constitutes the most important aspect of making the diagnosis. There is a wide range of morphological variations for rhabdomyoblasts which might reflect the dramatic metamorphism in rhabdomyogenesis [14, 15]. Typically, they are spindle to plump cells with eosinophilic cytoplasm, cigar-shaped nuclei, and prominent nucleoli. Cross striations can be present, but is not required. Other shapes include ribbonlike, tadpole, racquet, spider, and broken straw.
Benign mimickers of rhabdomyoblasts are legion. They include macrophages, squamous cells, crystal-containing cells, and rhabdoid cells. Sometimes, immunostainings might be needed to ascertain the cell nature. To avoid confusing apoptotic cells for rhabdoblasts, the cell nuclei should be viable. To avoid calling entrapped muscle cells as rhabdoblasts, attention to the striation and nuclear feature offers help. In rhabdomyoblasts, the striation usually traverses only part of the cell which contains moderate to severe atypical nuclei with prominent nucleoli.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree