Soft Tissue Sarcomas
Carol D. Morris
Soft tissue sarcomas are malignant neoplasms that arise in nonepithelial extraskeletal tissue (e.g., fat, muscle, fibrous structures, etc.) of mesenchymal origin. They account for less than 1% of all cancers, with approximately 8,000 to 9,000 diagnosed annually in the United States. Benign soft tissue tumors outnumber malignant ones by a factor of at least 100. More than 50 histologic subtypes of soft tissue sarcoma are recognized (Table 12-1).
Soft tissue sarcomas can occur anywhere in the body, though the majority occur in the extremities (50% to 75%). Ten percent occur on the trunk. As with other malignancies, soft tissue sarcoma tends to occur in older individuals, with a median age of 65, although there are subtype-related variations in peak age. For example, embryonal rhabdomyosarcoma occurs almost exclusively in children (<10 years old), synovial sarcoma occurs in young adults (20 to 40 years old), and pleomorphic sarcoma and liposarcoma occur in older adults (>60 years old). Approximately 10% of patients have clinically detectable metastases at presentation, usually in the lung.
The management of soft tissue sarcoma requires a multidisciplinary approach that includes surgery, radiation therapy, and chemotherapy. Treatment plans are best coordinated and administered when possible by specialty centers with expertise in treating the disease. The overall 5-year survival for patients with soft tissue sarcoma is largely dependent on the stage of disease. This, in turn, is determined by a combination of factors that include the grade, size, and location of the tumor. Using the four-tiered staging system of the American Joint Committee on Cancer (AJCC), 5-year survival rates are approximately 90% for stage I, 70% for stage II, 50% for stage III, and 10% to 20% for stage IV.
This chapter will review the rationale and outcomes for the management of soft tissue sarcoma with current treatment paradigms. In addition, the clinical and histopathologic presentation of the more common soft tissue sarcomas likely to be encountered in practice and on examinations will be discussed.
Pathogenesis
The etiology of soft tissue sarcoma is largely unknown. While numerous genetic aberrations continue to be identified, the clinical significance of these is still being elucidated. The more consistent genetic findings are outlined in connection with individual tumor types.
Etiology
Largely unknown
Chemical carcinogens
Increased incidence reported after exposure to dioxins (herbicides)
Controversial
Radiation
Termed “post-radiation” or “radiation-induced” sarcoma
More common in women, reflecting the distribution of conditions for which radiation is widely used: breast cancer, genitourinary cancers
Risk increases with dose, with most patients having received at least 50 Gy.
Table 12-1 Who Classification of Malignant Soft Tissue Tumors
Adipocytic tumors
Atypical lipomatous tumor/well-differentiated liposarcoma
Dedifferentiated liposarcoma
Myxoid liposarcoma
Round cell liposarcoma
Pleomorphic liposarcoma
Mixed-type liposarcoma
Liposarcoma, not otherwise specified
Fibroblastic/myofibroblastic
Solitary fibrous tumor and hemangiopericytoma
Inflammatory myofibroblastic tumor
Low-grade myofibroblastic sarcoma
Myxoinflammatory fibroblastic sarcoma
Infantile fibrosarcoma
Adult fibrosarcoma
Myxofibrosarcoma
Low-grade fibromyxoid sarcoma
Hyalinizing spindle cell tumor
Sclerosing epithelioid fibrosarcoma
Fibrohistiocytic tumors
Undifferentiated pleomorphic sarcoma
Pleomorphic malignant fibrous histiocytoma (MFH)
Giant cell MFH
Inflammatory MFH
Not otherwise specified
Smooth muscle tumors
Leiomyosarcoma
Skeletal muscle tumors
Embryonal rhabdomyosarcoma (including spindle cell, botryoid, anaplastic)
Alveolar rhabdomyosarcoma (including solid, anaplastic)
Pleomorphic rhabdomyosarcoma
Vascular tumors
Retiform hemangioendothelioma
Papillary intralymphatic angioendothelioma
Composite hemangioendothelioma
Kaposi sarcoma
Epithelioid hemangioendothelioma
Angiosarcoma of soft tissue
Chondro-osseous tumors
Mesenchymal chondrosarcoma
Extraskeletal osteosarcoma
Tumors of peripheral nerves
Malignant peripheral nerve sheath tumor (MSNST)
Tumors of uncertain differentiation
Synovial sarcoma
Epithelioid sarcoma
Alveolar soft part sarcoma
Clear cell sarcoma of soft tissue
Extraskeletal myxoid chondrosarcoma (“chordoid” type)
Primitive neuroectodermal tumor/extraskeletal Ewing tumor
Desmoplastic small round cell tumor
Extrarenal rhabdoid tumor
Malignant mesenchymoma
Neoplasms with perivascular epithelioid cell differentiation (PEComa)
Clear cell myomelanocytic tumor
Intimal sarcoma
Median time between exposure and tumor development is ∼10 years.
More common in patients with germline mutations
Viral and immunological factors
Increased incidence of sarcomas in immunocompromised individuals
Immunodeficiency syndromes
Therapeutic immunosuppression associated with organ transplantation
Stewart-Treves syndrome: an acquired “regional” immunodeficiency of the edematous upper extremity in breast cancer patients following radical mastectomy associated with lymphangiosarcoma
Oncogenic viruses
Human herpes virus 8 associated with Kaposi sarcoma
Epstein-Barr virus associated with leiomyosarcomas
Genetic predisposition
Neurofibromatosis-1 associated with malignant peripheral nerve sheath tumors (MPNST)
Li-Fraumeni syndrome: germline mutation in p53 suppressor gene
Hereditary retinoblastoma: germline mutation of RB1 locus
Epidemiology
Approximately 8,700 new cases diagnosed annually in the United States
Annual incidence is 1.5 per 100,000 individuals
8 per 100,000 in individuals greater than 80 years old
Slight male predominance
No proven racial variation
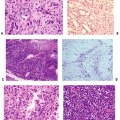
Classification
Soft tissue sarcomas are a highly heterogeneous group of tumors that are most commonly classified on a histological basis according to the tissue they most resemble. The most widely recognized classification system is that of the World Health Organization (WHO), which was first published in 1969 and most recently updated in 2002 (see Table 12-1).
Staging
Staging systems incorporate histological and clinical information for prognostic value.
The staging system used throughout this chapter is the AJCC staging system (Table 12-2).
75% of soft tissue sarcomas are high grade.
One third of soft tissue sarcomas are superficial and two thirds are deep.
Table 12-2 American Joint Committee on Cancer (Ajcc) Staging System for Soft Tissue Sarcoma | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||
Diagnosis
The diagnosis of soft tissue sarcoma is made with a combination of a good history and physical examination, appropriate radiology imaging, and biopsy.
The pertinent components of the history and physical examination as well as the clinical and radiologic features are detailed in Chapter 2.
Clinical Findings
Summary of clinical features and examination findings:
Most soft tissue sarcomas are painless.
Masses that are suspicious for sarcoma:
>5 cm regardless of location
Deep to fascia
Firm or fixed
Enlarging
Clinical features of tumors with advanced size
Distal edema
Nerve compression
Bladder symptoms (pelvic sarcomas)
Metastatic disease
10% of patients present with metastatic disease.
Lung is the most common metastatic site.
Bone (6%) and lymph node (3%) metastases are less common.
Radiologic Findings
Necessary imaging
Chest x-ray
Computed tomography (CT) of chest: preferred for detection of metastases
Magnetic resonance imaging (MRI) of primary site
CT with contrast substituted in patients with contraindication for MRI
CT often preferred for intra-abdominal tumors
Role of positron emission tomography (PET) scan unclear
Other Diagnostic Tests
Histologic analysis of tissue is required for staging and should be performed prior to initiating any treatment, with rare exceptions.
A good biopsy is the first step in a successful limb salvage operation.
Diagnostic tissue can be obtained by the following methods:
Needle
Fine-needle aspiration (FNA)
Core
Open incision
Open excisional
The advantages and disadvantages of each type of biopsy are discussed in Chapter 3, Biopsy of Musculoskeletal Tumors.
Diagnostic Tools
Numerous investigative tools are available to the pathologist to assist in the diagnosis of specific sarcoma subtypes (Tables 12-3 and 12-4).
Table 12-3 Common Immunohistochemistry Stains and Tissue Distribution | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Treatment
Soft tissue sarcoma is treated with an interdisciplinary approach that incorporates surgery, radiation, and chemotherapy. The details, rationale, and outcomes for each of these modalities are reviewed in Chapter 4, Treatment Principles. The following is a summary.
Surgery
Complete surgical excision is the main cornerstone of treatment.
Often curative for localized disease
Limb salvage is the preferred method.
Amputation is ultimately required in 5% to 10% of patients.
Radiation
Methods of delivery
External beam (pre-, post-, and intraoperation)
Brachytherapy
Table 12-4 CHROMOSOMAL TRANSLOCATIONS IN SOFT TISSUE SARCOMA
Tumor Type
Translocation
Involved Genes
Ewing/primitive neuroectodermal tumor
11;22
FLI1, EWS
Clear cell sarcoma
12;22
ATF1, EWS
Extraskeletal myxoid chondrosarcoma
9;22
CHN, EWS
Synovial sarcoma
X;18
SSX1 or SSX2, SYT
Myxoid liposarcoma
12;16
CHOP, TLS
Alveolar rhabdomyosarcoma
2;13
PAX3, FKHR
Alveolar soft part sarcoma
X;17
TFE3, ASPL
Dermatofibrosarcoma protuberans (DFSP)
17;22
COL1A1, PDGFB1
Typical dose ∼6,000 cGy
Primarily indicated for:
High-grade tumors (unless margins are very wide)
Intermediate-grade tumors with close margins
Large tumors
Recurrent disease
Improves local control by 20% to 35%
Chemotherapy
Indicated for patients at the highest risk of developing metastatic disease or patients with metastatic disease
Best administered in the setting of a clinical trial
Doxorubicin-based therapy is associated with a minimal improvement in overall survival (<10%).
Ifosfamide-based therapy is associated with moderately improved survival at intermediate follow-up; long-term results are unknown.
Results and Outcome
The outcome of patients with soft tissue sarcoma is multifactorial but largely dependent on the stage of disease. The overall survival for all patients with soft tissue sarcoma is approximately 70%. Using the four-tiered staging system of the AJCC, 5-year survival rates are approximately 90% for stage I, 70% for stage II, 50% for stage III, and 10% to 20% for stage IV.
Negative prognostic factors
Metastatic disease
High histologic grade
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree