Skin-sparing mastectomy (SSM) has emerged as an oncologically safe approach to early-stage breast cancer and prophylactic mastectomies.1,2 This technique improves aesthetic outcomes by preserving the maximum amount of native anatomy including the inframammary fold, which improves the shape and position of the breast mound. The maximal amount of uninvolved skin is preserved, reducing or removing the need for a reconstructive skin paddle. The aesthetic results using this native envelope cannot be matched by any reconstructive technique.
With the advent of SSM, reconstructive efforts began to focus on optimizing incision placement and managing the residual skin envelope. Common approaches for SSM include the elliptical, periareolar, and periareolar with lateral extension skin patterns.3,4 These approaches do not address the specific reconstructive needs in a large, ptotic breast.
Skin-reduction mastectomy is the application of SSM technique in the setting of macromastia. The large breast poses a unique challenge to reconstruction.4 The residual envelope is ill-suited for implant or autologous reconstruction, and the accompanying ptosis does not result in an aesthetically pleasing breast. Mastectomy techniques which employ standard breast reduction patterns have been created to address this problem. The pattern is designed to correct the ptosis and shape the skin envelope. For unilateral reconstructions, this allows for improved symmetry with a contralateral reduction pattern. In bilateral reconstruction, the pattern improves the final shape of the breasts. When employed with nipple-sparing mastectomy, the pattern incorporates elevation of the nipple-areolar complex (NAC) into the design.
Toth and Lappert1 appreciated the benefit of preoperative reconstruction planning in SSM. He described skin reductions which excised full-thickness skin in the standard Wise pattern. Bostwick5 modified this technique to utilize the preserved skin by de-epithelializing the reduction pattern. The remaining adipofascial flap was secured to the pectoralis muscle to provide an additional layer of tissue under the mastectomy skin. Hammond et al6 further modified this technique to optimize the aesthetic benefits of complete implant coverage without the constriction of a lower pole muscle flap (Fig. 156-1A, B).
FIGURE 156-1
A. AP diagram of a Wise-pattern skin reduction closure. The lower adipofascial flap is secured to the pectoralis muscle to provide complete tissue expander coverage. B. Lateral diagram of a Wise-pattern skin reduction closure. The skin pattern is closed over the muscle-adipofascial flap and new nipple position created on the mastectomy skin flap.
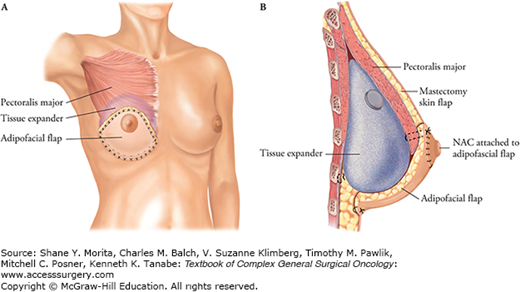
The Wise-pattern reductions involve closure in the standard inverted-T pattern, which has an increased risk of marginal necrosis at the “T” point. The de-epithelialized lower flap provides additional deep coverage in the event of marginal necrosis. Vertical reduction patterns have also been described and have the benefit of avoiding the “T” point, but they lack incorporation of the adipofascial flap.3,7,8
Skin-reduction mastectomy patterns need attention on the management of the skin envelope, while the inner breast mound may be reconstructed using any available technique. All varieties of implant-based and autologous reconstructions have been employed in conjunction with these patterns.3–12 Preservation of the NAC, when oncologically appropriate, may also be incorporated into the reduction pattern. The NAC may remain attached on the adipofascial flap or applied to the reduced skin flap as a graft.5,6
The techniques below will describe the application of skin reduction patterns in the setting of breast reconstruction. The same skin and adipofascial patterns can be utilized for either implant-based or autologous reconstruction.
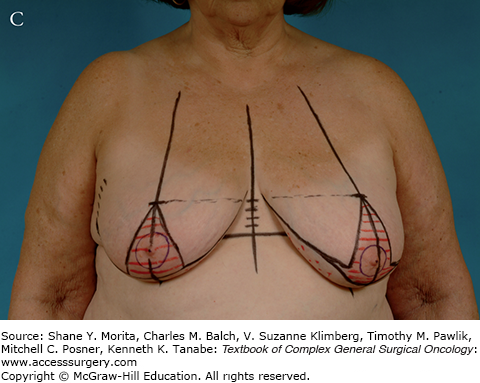
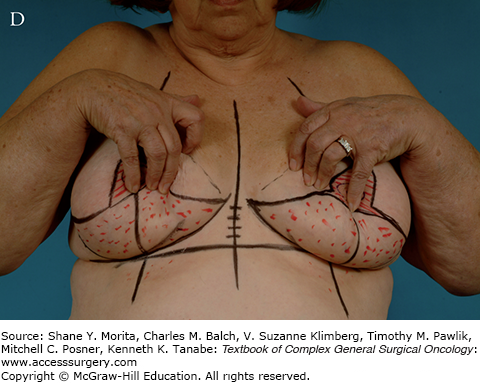
The patient is marked in the upright position. The midline and breast meridians are placed on the anterior chest wall and the curve of the inframammary fold is traced. Next, the level of the inframammary fold is marked across the width of the anterior chest. A point along the midline is marked at 4 cm above the inframammary fold. This is the estimated top of the new NAC position. This mark is drawn across the width of the chest, taking care to avoid distortion by the breast mounds as the line is transposed laterally. A Wise pattern is marked at the intersection of the new NAC position and the breast meridian. This pattern has vertical limbs of 8 to 9 cm in length and an angle such that the base also measures 8 to 9 cm in width. Medial and lateral limbs are drawn to connect the vertical limbs to the medial and lateral extents of the inframammary fold (Fig. 156-2A–D).
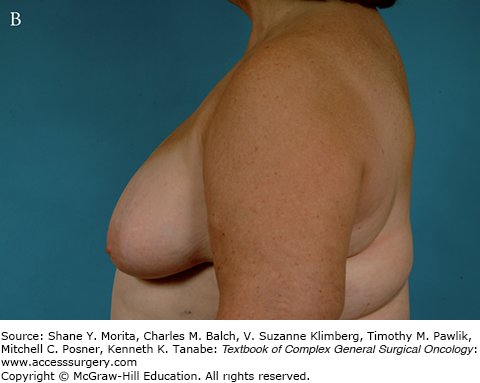
FIGURE 156-2
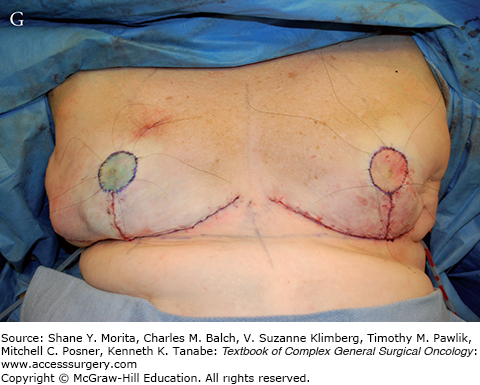
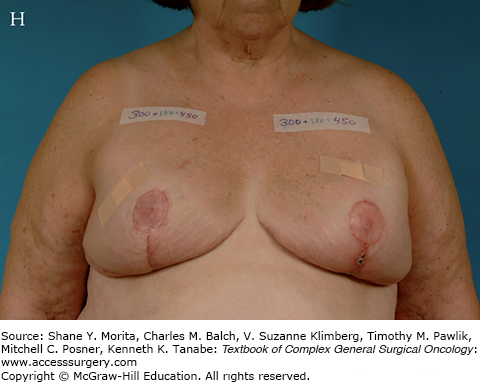
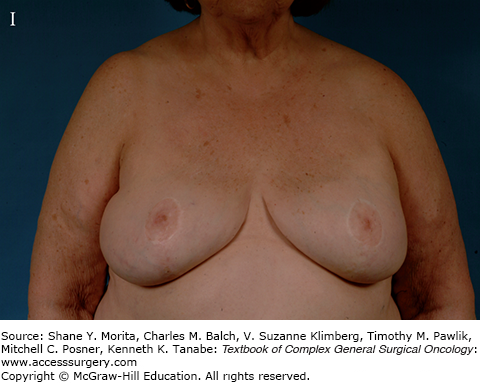
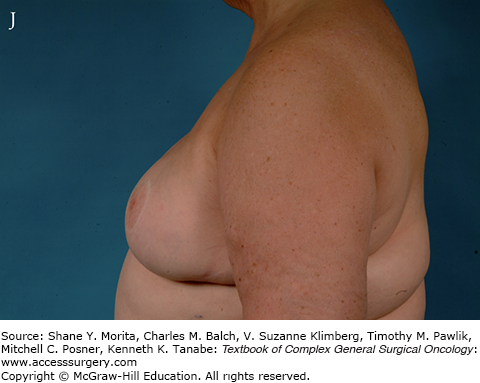
This patient was determined to be a candidate for bilateral nipple-sparing mastectomy. A, B. AP and lateral views of the patient demonstrate macromastia and ptosis, making her a candidate for skin-reduction mastectomy. C, D. The patient is marked preoperatively in the upright position with standard Wise pattern with 8-cm limbs. E. The tissue expander is in place under a de-epithelialized muscle-adipofascial flap. F. The skin will be closed in an inverted-T pattern. G. The new nipple positions are determined with the patient in a 90-degree upright position. The nipples are placed as full-thickness grafts and secured with bolsters. H. The tissue expanders are in place and serially filled to desired volume. I, J. AP and lateral views of the 2-year postoperative appearance after placement of 800cc smooth round silicone gel implants bilaterally. A successful reconstruction with lifting of the breast and NAC position has been achieved with good symmetry. The NAC grafts have survived completely.



At the time of the surgery, the adipofascial flap is meticulously de-epithelialized prior to mastectomy, preserving dermis throughout. This may be deferred until completion of mastectomy; however, it is more easily performed prior to removal of the underlying tissue. The NAC is marked under stretch at 40 to 44 mm and incised. The upper triangle and lower pole pattern are de-epithelialized, leaving a lower pole adipofascial flap. The mastectomy proceeds using wide access provided by the vertical and horizontal limbs of the de-epithelialized pattern. Upon completion of the mastectomy, the breast reconstruction is performed. For the cases detailed in Figs. 156-2 and 156-3, the reconstruction was performed with a tissue expander. The lateral and inferior-medial attachments of the pectoralis major muscle are released and the plane between the pectoralis major and minor is opened to the extent of the breast footprint. A prepared tissue expander is placed into the submuscular pocket. The pectoralis muscle is then draped over the expander and secured to the adipofascial flap for a total submuscular-subfascial pocket (Fig. 156-2E). Care is taken to avoid distortion of the inframammary fold when positioning the lower adipofascial flap over the expander. The skin is then closed in the inverted-T pattern over drain (Fig. 156-2F). The new NAC position is marked with the patient seated upright to 90 degrees. This is placed at the point of maximal projection of the breast, which is approximately 18 to 23 cm from the midclavicular point and keeping symmetry with the contralateral NAC in mind (Fig. 156-2G).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






