Sentinel Lymphadenectomy
CRITICAL ELEMENTS
Identification of All Sentinel Nodes
Technique for Injecting Localizing Tracer or Dye
Preincision Evaluation of Drainage Pattern
Node Removal Technique to Limit Seroma Formation
1. IDENTIFICATION OF ALL SENTINEL NODES
Recommendation: All sentinel nodes must be identified, removed, and subjected to pathologic analysis to ensure that sentinel lymph node mapping and sentinel lymphadenectomy provide accurate information for breast cancer staging. Sentinel nodes are defined by the presence of a tracer (radioactive tracer and/or colored dye) that has been previously injected into the affected breast or by the presence of a dominant palpable lymph node identified by the operating surgeon.
Type of Data: Randomized multicenter prospective trials.
Strength of Recommendation: The group strongly endorses this recommendation based on strong evidence.
Rationale
The original definition of a sentinel lymph node was “the first draining lymph node on the direct pathway from the primary tumor site.”1 According to the sentinel node hypothesis, tumor cells migrate from a primary tumor focus to the first draining lymph node(s) before involving distal lymph nodes. Sentinel lymph nodes are variably located but are usually within the level I or II axilla near the lateral thoracic vein.2,3 The median number of sentinel nodes removed during a sentinel lymphadenectomy is between two and three; in the two largest randomized clinical trials comparing sentinel
lymphadenectomy to axillary node dissection, the mean numbers of sentinel nodes removed per procedure were 2.8 in the National Surgical Adjuvant Breast and Bowel Project B32 trial3 and 2.2 in the ALMANAC (Axillary Lymphatic Mapping Against Nodal Axillary Clearance) trial.4 For cases in which only one sentinel lymph node is removed, the reported false negative rate of the procedure is greater than 10%, potentially leading to the assignment of lower than actual disease stages to some breast cancers.5
lymphadenectomy to axillary node dissection, the mean numbers of sentinel nodes removed per procedure were 2.8 in the National Surgical Adjuvant Breast and Bowel Project B32 trial3 and 2.2 in the ALMANAC (Axillary Lymphatic Mapping Against Nodal Axillary Clearance) trial.4 For cases in which only one sentinel lymph node is removed, the reported false negative rate of the procedure is greater than 10%, potentially leading to the assignment of lower than actual disease stages to some breast cancers.5
Identification Using a Radioactive Tracer
Most commonly technetium sulfur colloid is injected in the breast an hour prior to the planned sentinel node biopsy, but the tracer can be injected the day before if more convenient. After the patient is under general anesthesia, a handheld gamma detection probe is held over the axilla to identify the area of greatest radioactivity. A 3- to 6-cm incision is then made near the area of greatest radioactivity within the region at the base of the axillary hairline. The clavipectoral fascia is opened to the level I axilla, and the area around the lateral thoracic vein and second intercostobrachial nerve is evaluated using the gamma detection probe. The first sentinel node is the node with the highest absolute radioactivity count. The nodes are excised using clip, tie, or sealing device closure of the indwelling lymphatics and vessels, and blunt dissection of the surrounding fat is performed to prevent the removal of multiple nonsentinel nodes. After the first sentinel node is excised, its ex vivo highest or 10-second radioactive count is obtained and recorded, and the radioactivity of the axillary basin is reassessed. All nodes whose radioactive count is at least 10% that of the most radioactive node are considered sentinel nodes and are removed in a similar fashion, and ex vivo radioactive counts are recorded for each node. Confirmation of an elevated ex vivo count of the node ensures that it is indeed a hot node and not that the count was falsely elevated in vivo due to scatter from the primary injection in the breast.
Identification Using Vital Blue (or Colored) Dye
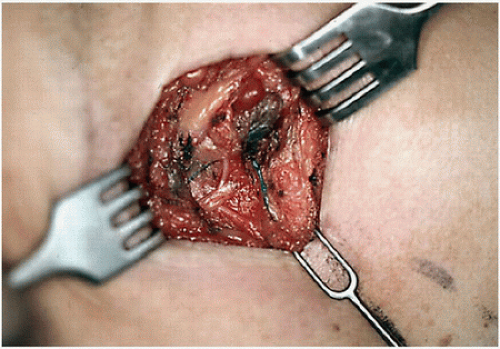
For sentinel node identification with a blue dye, isosulfan or methylene blue are most commonly used. The dye is injected in the breast and massaged; subsequently, the axilla is incised and opened as described for sentinel node identification with a radioactive tracer. Blunt dissection is performed to identify the dye-filled lymphatic tract. This tract is then followed proximally and distally until a blue-stained sentinel node is identified (Fig. 4-1). If more than one dye-filled lymphatic tract is identified, each is followed until a blue node is identified. Blue-stained sentinel nodes are removed in a fashion similar to that used to remove sentinel nodes identified using a radioactive tracer. Another colored tracer in current use is indocyanine green; in cases in which this tracer is used, all nodes with fluorescent tracer uptake must be identified.
Identification Using a Dual-Tracer Approach
The majority of sentinel lymphadenectomy procedures utilize a dual-tracer technique.6 If both a radioactive tracer and blue dye have been injected, nodes that are
radioactive and/or stained blue are considered sentinel nodes. All blue-stained nodes should be assessed with a gamma detection probe for radioactivity, and all radioactive nodes that are removed should be assessed for the presence of blue dye. Some nodes may only be identified by one modality, as studies show that the procedure is the most accurate when dual tracer technique is utilized.6
radioactive and/or stained blue are considered sentinel nodes. All blue-stained nodes should be assessed with a gamma detection probe for radioactivity, and all radioactive nodes that are removed should be assessed for the presence of blue dye. Some nodes may only be identified by one modality, as studies show that the procedure is the most accurate when dual tracer technique is utilized.6
Identification Using Palpation of the Axilla
As a component of sentinel lymphadenectomy, careful palpation of the level I and II axilla is essential to guiding the complete removal of all sentinel nodes. Nodes that feel abnormal on palpation should be categorized as sentinel nodes and removed regardless of whether they are radioactive or stained blue.7
2. TECHNIQUE FOR INJECTING LOCALIZING TRACER OR DYE
Recommendation: The site of localizing tracer or dye injection within the affected breast and/or subareolar plexus does not influence the identification of the axillary sentinel node(s).
Type of Data: Multiple single institutional series, small prospective randomized study, and systematic review.
Strength of Recommendation: Consensus of the group is that the evidence is strong.
Rationale
Over the past 15 years, several different techniques and combinations of techniques have been employed for the injection of radioactive tracer and/or dye for sentinel node identification. Pesek et al5 published the most comprehensive and systematic
review of injection techniques for sentinel node identification. They concluded that of the seven different techniques and combinations of techniques they studied, including peritumoral (intraparenchymal) injection, sub- or (peri)areolar injection (Figs. 4-2 and 4-3), subdermal but nonintratumoral injection, intratumoral injection, peritumoral/subareolar injection, peritumoral/subdermal injection, and subareolar/subdermal injection, none had a significantly lower false negative rate than another; therefore, they could not justify recommending one technique over another.5 A multicenter prospective randomized study found that, compared with peritumoral injection
of a radioactive tracer and blue dye, periareolar injection of a tracer and dye had a higher sentinel lymph node detection rate and higher within-node dye-tracer concordance.7 One small study investigating radioactive tracer injection in both subareolar and peritumoral locations in individual patients (27 patients total) noted no difference in the number of axillary sentinel nodes identified using subareolar or peritumoral radioactive tracer injection; however, the study did find that peritumoral injection resulted in the localization of extra-axillary drainage sites (e.g., internal mammary [IM] nodes, paraclavicular nodes).8,9 If extra-axillary sites are of interest, the radioactive tracer should be injected peritumorally. In developing quality metrics for sentinel node mapping (other than false negative rate, which requires a full axillary node dissection), Quan et al6 did not include the tracer or dye injection site as one of the quality indicators because they found no data supporting one injection location over another. The findings of these studies demonstrate that no specific injection site ensures the lowest false negative rate and highest sentinel node identification rate. However, surgeons should monitor their performance of dye and radioactive tracer injection to ensure that the injection sites they use result in the identification of all sentinel nodes, an average number of removed sentinel nodes greater than 1.9, and a sentinel node positivity rate of 20% to 30%.6
review of injection techniques for sentinel node identification. They concluded that of the seven different techniques and combinations of techniques they studied, including peritumoral (intraparenchymal) injection, sub- or (peri)areolar injection (Figs. 4-2 and 4-3), subdermal but nonintratumoral injection, intratumoral injection, peritumoral/subareolar injection, peritumoral/subdermal injection, and subareolar/subdermal injection, none had a significantly lower false negative rate than another; therefore, they could not justify recommending one technique over another.5 A multicenter prospective randomized study found that, compared with peritumoral injection
of a radioactive tracer and blue dye, periareolar injection of a tracer and dye had a higher sentinel lymph node detection rate and higher within-node dye-tracer concordance.7 One small study investigating radioactive tracer injection in both subareolar and peritumoral locations in individual patients (27 patients total) noted no difference in the number of axillary sentinel nodes identified using subareolar or peritumoral radioactive tracer injection; however, the study did find that peritumoral injection resulted in the localization of extra-axillary drainage sites (e.g., internal mammary [IM] nodes, paraclavicular nodes).8,9 If extra-axillary sites are of interest, the radioactive tracer should be injected peritumorally. In developing quality metrics for sentinel node mapping (other than false negative rate, which requires a full axillary node dissection), Quan et al6 did not include the tracer or dye injection site as one of the quality indicators because they found no data supporting one injection location over another. The findings of these studies demonstrate that no specific injection site ensures the lowest false negative rate and highest sentinel node identification rate. However, surgeons should monitor their performance of dye and radioactive tracer injection to ensure that the injection sites they use result in the identification of all sentinel nodes, an average number of removed sentinel nodes greater than 1.9, and a sentinel node positivity rate of 20% to 30%.6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree