“The incidence of melanoma is increasing faster than any other cancer. The status of the regional nodal basin remains the most important prognostic factor. Sentinel lymph node biopsy (SLNB) is recommended for staging in patients diagnosed with intermediate-thickness melanoma (1.01–4.0 mm). SLNB is considered somewhat controversial, especially when used to stage thin (1 mm), thick (>4 mm), or desmoplastic melanoma. This article reviews the current literature regarding SLNB in thin, intermediate, thick, and desmoplastic melanoma. Data supporting the use of newer radiopharmaceuticals in sentinel lymph node mapping along with newer imaging modalities are also reviewed.”
Key points
- •
More than 76,000 cases of melanoma were diagnosed in 2013, with most of those cases being thin melanoma (≤1.0 mm).
- •
The standard of care in staging the regional nodal basin in patients with intermediate-thickness melanoma (1.01–4.0 mm) is sentinel lymph node biopsy.
- •
Thin melanomas (0.76–1.0 mm) as well as thick melanomas (>4.0 mm) should be considered for a sentinel lymph node biopsy.
- •
The addition of newer radiocolloids and single-photon emission computed tomography lymphoscintigraphy may help improve the accuracy of finding sentinel lymph nodes.
The incidence of melanoma is increasing faster than any other cancer, with an estimated lifetime risk of 1 in 53. In the United States in 2013, more than 76,690 cases of invasive melanoma were diagnosed with an estimated 9480 deaths from the disease. The most common site of melanoma metastasis involves the regional nodal basin and the status of the sentinel lymph node (SLN) has been for decades, and still remains, the most important prognostic factor in the diagnosis of melanoma. SLN biopsy (SLNB) has been to shown to be highly accurate with low morbidity and is currently recommended to be performed for staging in patients diagnosed with an intermediate-thickness melanoma (1.01–4.0 mm), as summarized in Table 1 . SLNB has been the subject of controversy, especially when used to stage thin (≤1 mm), thick (>4 mm), or desmoplastic melanomas (DM). This article reviews the current literature regarding the use of SLNB in thin, intermediate, and thick melanoma, and in DM. Data supporting the use of newer radiopharmaceuticals and colorimetric agents in SLN mapping, along with newer imaging modalities to identify SLNs, are also reviewed.
| Melanoma Thickness (mm) | NCCN Recommendations Regarding SLNB |
|---|---|
| Melanoma in situ | Not recommended |
| <0.76 | Not recommended |
| 0.76–1.0 (no ulceration and mitotic rate <1/mm 2 ) | Considered |
| 0.76–1.0 (ulcerated or mitotic rate ≥1/mm 2 ) | Discussed and offered |
| ≥1.0–4.0 | Discussed and offered |
Randomized trials of sentinel lymph node biopsy in melanoma
The role of SLNB in melanoma has been evaluated by several large, prospective, randomized trials. The Multicenter Selective Lymphadenectomy Trial (MSLT-I) was a prospective, randomized trial designed with the goal of determining whether SLNB provided a survival benefit to patients with primary melanoma. The Sunbelt Melanoma Trial, another prospective, randomized trial, was also designed to evaluate survival after SLNB, as well as the benefit of adjuvant interferon (IFN) alfa-2b toward overall survival (OS) or disease-free survival (DFS). The Multicenter Selective Lymphadenectomy Trial II (MSLT-II), which has reached its accrual goal in 2014 and is currently in the follow-up stage, was designed to determine whether a completion lymph node dissection (CLND) of the affected nodal basin was necessary after detection of a positive SLNB, with the intent to determine whether CLND has any benefit in regional control or OS.
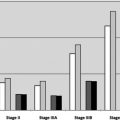
MSLT-I began patient accrual in 1994 and reached its target of 2001 patients in March of 2002. The final analysis was published in early 2014. The patients were randomly assigned to either undergo wide local excision (WLE) alone with observation of the nodal basin or WLE with SLNB and immediate CLND if there was a positive SLN. The trial evaluated 1347 patients with intermediate-thickness melanomas (1.2–3.5 mm). Final analysis showed no difference between the SLN and observation groups with respect to melanoma-specific survival (MSS) at 10 years (81.4% and 78.3%; hazard ratio [HR], 0.84; P = .18). Improvement in 10-year DFS of 71.3% versus 64.7% (HR, 0.76; P = .01) in favor of the SLN group was reported. Patients who had SLN metastasis had worse outcomes than those who were SLN negative, with a 10-year MSS of 62.1% versus 85.1% for SLN positive versus negative, respectively (HR, 3.09; P <.001). On multivariate analysis, the investigators reported that SLN status was the strongest predictor of recurrence or death from melanoma. Patients with SLN metastasis who received immediate CLND were compared with those in the observation group who failed in the nodal basin with clinically obvious disease, with distant DFS being significantly improved in favor of the SLN-positive group (54.8% vs 35.6%; HR, 0.62; P = .02). Of those with nodal metastasis, the 10-year MSS was significantly improved in favor of the those with a positive SLN versus those who failed clinically in the nodal basin in the observation group (62.1% vs 41.5%; HR, 0.56; P = .006). The MSLT-I trial concluded that the use of SLNB in intermediate-thickness melanoma is not only feasible; it improves DFS and decreases the risk of nodal recurrence and distant metastasis. MSS was significantly improved in those with SLN metastasis compared with those observed with clinical nodal failure, supporting that detection of nodal metastases at an occult stage via SLNB is beneficial.
The Sunbelt Melanoma Trial is a multicenter prospective randomized trial to evaluate the role of high-dose IFN-α2b or observation (no adjuvant therapy) in patients who had a CLND after a positive SLNB. The trial also evaluated the impact of reverse transcription polymerase chain reaction (RT-PCR)–positive SLNs that were initially negative by standard histology and immunohistochemistry (IHC), and then found to be positive on RT-PCR for tyrosinase and at least 1 other marker (MART-1, gp 100, or MAGE-3). Those patients who were SLNB positive by RT-PCR were randomized to observation, CLND, or CLND plus IFN-α. The final analysis included 774 patients with a median follow-up of 64 months. The patients who were randomized to IFN groups received treatments for a total of 52 weeks. Primary end points of the study were OS and DFS. No statistical significant difference was seen in OS (HR, 1.07; P = .79) or DFS (HR, 0.82; P = .46) in patients randomized to either IFN or observation. No statistical significant benefit was reported among those found to be positive by RT-PCR analysis treated with CLND, CLND plus IFN-α, or observation. This study concluded that there was no additional benefit for the addition of IFN-α after undergoing a CLND for SLN-positive disease detected by hematoxylin and eosin or IHC, and in those patients in whom SLN disease was detected by RT-PCR there was no benefit to CLND or CLND plus IFN.
Although the current standard of care is to perform a CLND for patients with a positive SLN, only about 15% to 18% of completion lymphadenectomy specimens after SLNB contain additional nodes with metastatic disease (ie, nonsentinel nodes). MSLT-II was designed to determine whether CLND is necessary in patients with a positive SLN. The primary outcome of MSLT-II is MSS. The secondary outcomes are OS; DFS; prognostic accuracy of histopathology; molecular and immunologic markers; and quality of life. The study commenced in December 2004 and has just reached its accrual goal of 1925 patients (in early 2014). Patients with a positive SLNB are randomly assigned either to undergo immediate CLND or observation with high-resolution ultrasonography every 4 months for 2 years; every 6 months for years 3, 4, and 5; and yearly thereafter.
Randomized trials of sentinel lymph node biopsy in melanoma
The role of SLNB in melanoma has been evaluated by several large, prospective, randomized trials. The Multicenter Selective Lymphadenectomy Trial (MSLT-I) was a prospective, randomized trial designed with the goal of determining whether SLNB provided a survival benefit to patients with primary melanoma. The Sunbelt Melanoma Trial, another prospective, randomized trial, was also designed to evaluate survival after SLNB, as well as the benefit of adjuvant interferon (IFN) alfa-2b toward overall survival (OS) or disease-free survival (DFS). The Multicenter Selective Lymphadenectomy Trial II (MSLT-II), which has reached its accrual goal in 2014 and is currently in the follow-up stage, was designed to determine whether a completion lymph node dissection (CLND) of the affected nodal basin was necessary after detection of a positive SLNB, with the intent to determine whether CLND has any benefit in regional control or OS.
MSLT-I began patient accrual in 1994 and reached its target of 2001 patients in March of 2002. The final analysis was published in early 2014. The patients were randomly assigned to either undergo wide local excision (WLE) alone with observation of the nodal basin or WLE with SLNB and immediate CLND if there was a positive SLN. The trial evaluated 1347 patients with intermediate-thickness melanomas (1.2–3.5 mm). Final analysis showed no difference between the SLN and observation groups with respect to melanoma-specific survival (MSS) at 10 years (81.4% and 78.3%; hazard ratio [HR], 0.84; P = .18). Improvement in 10-year DFS of 71.3% versus 64.7% (HR, 0.76; P = .01) in favor of the SLN group was reported. Patients who had SLN metastasis had worse outcomes than those who were SLN negative, with a 10-year MSS of 62.1% versus 85.1% for SLN positive versus negative, respectively (HR, 3.09; P <.001). On multivariate analysis, the investigators reported that SLN status was the strongest predictor of recurrence or death from melanoma. Patients with SLN metastasis who received immediate CLND were compared with those in the observation group who failed in the nodal basin with clinically obvious disease, with distant DFS being significantly improved in favor of the SLN-positive group (54.8% vs 35.6%; HR, 0.62; P = .02). Of those with nodal metastasis, the 10-year MSS was significantly improved in favor of the those with a positive SLN versus those who failed clinically in the nodal basin in the observation group (62.1% vs 41.5%; HR, 0.56; P = .006). The MSLT-I trial concluded that the use of SLNB in intermediate-thickness melanoma is not only feasible; it improves DFS and decreases the risk of nodal recurrence and distant metastasis. MSS was significantly improved in those with SLN metastasis compared with those observed with clinical nodal failure, supporting that detection of nodal metastases at an occult stage via SLNB is beneficial.
The Sunbelt Melanoma Trial is a multicenter prospective randomized trial to evaluate the role of high-dose IFN-α2b or observation (no adjuvant therapy) in patients who had a CLND after a positive SLNB. The trial also evaluated the impact of reverse transcription polymerase chain reaction (RT-PCR)–positive SLNs that were initially negative by standard histology and immunohistochemistry (IHC), and then found to be positive on RT-PCR for tyrosinase and at least 1 other marker (MART-1, gp 100, or MAGE-3). Those patients who were SLNB positive by RT-PCR were randomized to observation, CLND, or CLND plus IFN-α. The final analysis included 774 patients with a median follow-up of 64 months. The patients who were randomized to IFN groups received treatments for a total of 52 weeks. Primary end points of the study were OS and DFS. No statistical significant difference was seen in OS (HR, 1.07; P = .79) or DFS (HR, 0.82; P = .46) in patients randomized to either IFN or observation. No statistical significant benefit was reported among those found to be positive by RT-PCR analysis treated with CLND, CLND plus IFN-α, or observation. This study concluded that there was no additional benefit for the addition of IFN-α after undergoing a CLND for SLN-positive disease detected by hematoxylin and eosin or IHC, and in those patients in whom SLN disease was detected by RT-PCR there was no benefit to CLND or CLND plus IFN.
Although the current standard of care is to perform a CLND for patients with a positive SLN, only about 15% to 18% of completion lymphadenectomy specimens after SLNB contain additional nodes with metastatic disease (ie, nonsentinel nodes). MSLT-II was designed to determine whether CLND is necessary in patients with a positive SLN. The primary outcome of MSLT-II is MSS. The secondary outcomes are OS; DFS; prognostic accuracy of histopathology; molecular and immunologic markers; and quality of life. The study commenced in December 2004 and has just reached its accrual goal of 1925 patients (in early 2014). Patients with a positive SLNB are randomly assigned either to undergo immediate CLND or observation with high-resolution ultrasonography every 4 months for 2 years; every 6 months for years 3, 4, and 5; and yearly thereafter.
Complications associated with sentinel lymph node biopsy
The use of SLNB has supplanted the use of elective CLND and become the standard of care around the world in patients with primary, localized melanomas. CLND can be associated with increased morbidity with the most common complications being wound infection, seroma/hematoma, lymphedema, pain, and numbness. The incidence of these complications is significantly higher in CLND compared with SLNB. This difference has been addressed in several trials, including MSLT-I and The Sunbelt Melanoma Trial. In MSLT-I, complications occurred in 10.1% of patients undergoing just SLNB, compared with 37.2% with the addition of CLND. The Sunbelt Melanoma Trial also compared SLNB and SLNB plus CLND and showed higher rates of wound infection (1.1% vs 7.0%), lymphedema (0.7% vs 11.7%), and seroma/hematoma (2.3% vs 5.9%) with SLNB plus CLND. There have been reports of allergic reactions after the use blue dye, especially isosulfan blue dye. MSLT-I reported only a 0.2% incidence of allergic reaction to isosulfan blue dye when used for SLNB. In general, SLNB is a safe procedure that yields accurate results for patients diagnosed with early-stage melanoma.
Management of thin melanoma
No consensus in the literature exists on whether to perform SLNB in patients with thin melanoma (≤1 mm). The American Society of Clinical Oncology and Society of Surgical Oncology (ASCO/SSO), along with the National Comprehensive Cancer Network (NCCN), recommend consideration of SLNB in certain patients with thin melanomas, not routine use as recommended in patients with intermediate-thickness melanomas (see Table 1 ). Some clinicians argue against SLNB in thin melanoma because of the reported low rate of nodal metastases (<5%), whereas others report a higher than 5% incidence of nodal metastasis in thin melanomas.
Kesmodel and colleagues conducted a retrospective single-institution review of 181 patients with thin melanomas (≤1 mm) over an 8-year period. Univariate and multivariate logistic regression analysis was performed to identify clinical and histopathologic variables in thin melanoma associated with an increased risk for SLN positivity. Age, sex, anatomic location, mitotic rate (MR), thickness, Clark level, and ulceration were examined. MR and Clark level were further defined as 0 or more than 0 mitoses and level II/III or IV/V, respectively. The overall reported SLN positivity rate was 5% for the sample cohort analyzed. Both MR ( P =.011) and tumor thickness (≥0.76 mm) ( P = .033) were significant for SLN positivity on univariate analysis. On multiple regression analysis, only MR remained significant. The investigators concluded that MR was a predictor of SLN metastasis in thin melanoma and could be used to help determine which patients with thin melanomas (≤1 mm) should undergo SLNB and are at higher risk for SLN metastases.
More recently, Han and colleagues assessed 271 patients with thin melanomas to determine factors predictive of nodal metastasis. Clinicopathologic factors that were evaluated included age, Breslow thickness, Clark level, regression, ulceration, MR, positive deep biopsy sample margin, vertical growth phase (VGP), tumor-infiltrating lymphocytes (TILs), and the American Joint Committee on Cancer (AJCC) T classification. The overall median Breslow thickness was 0.85 mm (range, 0.3–1.0 mm; P = nonsignificant). Of the 271 patients, 22 (8.1%) had a positive SLN. Melanomas were also classified as either T1a or T1b. Five percent of T1a melanomas (no ulceration, and MR<1/mm 2 ) had positive SLNs, whereas 13% of patients with T1b melanomas (ulcerated and/or MR ≥1/mm 2 ) had a positive SLN. Multiple logistic regression analysis showed that ulceration significantly correlated with SLN metastasis ( P <.05) and MR greater than or equal to 1/mm 2 significantly correlated with any nodal metastasis ( P <.05) including recurrent regional nodal disease. Age, Clark level, regression, positive deep biopsy sample margin, TIL, and VGP were not significant predictors of either clinically positive nodal disease or SLN metastasis. SLN metastasis was seen in 8.4% of all thin melanomas greater than or equal to 0.76 mm, whereas 6.1% of those less than 0.76 mm had a positive SLN (both SLN-positive patients in the <0.76 mm group had T1b melanomas). From these results the investigators concluded that it is justifiable to consider and perform SLNB in patients with tumors greater than or equal to 0.76 mm. The investigators concluded that, in the absence of ulceration, there is no clear indication for SLNB in melanomas less than 0.76 mm.
The same group followed up with a larger retrospective review of a multi-institutional database of 1250 patients with thin melanoma (≤1 mm) from 1994 to 2012 to determine which clinicopathologic factors increase the risk of SLN metastasis in patients with thin melanomas. Clinicopathologic factors analyzed in this study were Breslow thickness, Clark level, ulceration, MR, regression, VGP, lymphovascular invasion, and TILs. Median follow-up was 2.6 years. On univariate analysis, Breslow thickness, Clark level, ulceration, and MR were significantly different between SLN-positive and SLN-negative groups. On multiple logistic regression analysis, Breslow thickness greater than or equal to 0.75 mm ( P = .03), Clark level greater than or equal to IV ( P = .05), and ulceration ( P = .01) predicted SLN metastasis. The overall risk was 5.2%, but it increased to 6.3% in tumors greater than or equal to 0.75 mm. Although varying values of MR have been reported in several studies to be predictive of SLN metastasis, an MR of greater than or equal to 1.0/mm 2 did not predict SLN metastasis in melanoma in this study ( P = .98). Of all SLN-positive patients, 86.2% had a thickness greater than or equal to 0.75 mm. Of those patients with a melanoma greater than or equal to 0.75 mm and a positive SLN, more than 90% were ulcerated and/or Clark level greater than or equal to IV. The investigators showed that using only ulceration or Clark level greater than or equal to IV potentially misses 81.7% and 31.6% of SLN-positive patients. They concluded that a 5% risk of metastasis should be used as a threshold for performing SLNB, and this threshold was met in patients with melanomas of greater than or equal to 0.75 mm. Although SLN positivity has been reported in patients with melanomas less than 0.5 mm, none were positive in this study and only 2.5% of those patients with primary melanomas between 0.5 and 0.75 mm had a positive SLN.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree