Breast ultrasound has become an essential tool for the breast surgeon. Traditionally, however, it has not been a part of the general surgical curriculum, and many practicing surgeons are still struggling with how to incorporate breast ultrasound into their practice. This chapter will outline the steps to facilitate this transition.
The minimum requirements for a functional breast ultrasound machine are listed in Table 32-1. Fortunately, because of recent advances in software, solid-state circuitry, and probe technology, machines that are more sophisticated are now available, and a more suitable choice of features would include some of the additional features listed. The most important aspect of the machine itself is the probe, which ideally would be a multifrequency 8 to 14 MHz linear array probe (although a 7.5-10 MHz probe will also work well). Today, almost any unit that will accommodate this type of probe will include the other features required for high-quality scanning.
| Minimum Requirements |
|---|
| 7.5-MHz linear array probe |
| High-quality black and white monitor, > 10-in diagonal |
| Adjustable focal zone |
| Controls to modify scanning depth and TGC curve |
| Ability to document details of the scan, including patient name or identifier, date, time, location and orientation of the probe, MHz, and frames per second |
| Desirable Features |
| 8–14-MHz linear array probe |
| High-quality color monitor, > 14-in diagonal |
| Color and power Doppler |
| Available Useful Options (price-dependent) |
| Compound imaging |
| Harmonic imaging |
| 3-dimensional scanning |
Other requirements include a large, high-quality black and white display, or color display if color Doppler is available, and the ability to record information about the scan on the recorded image, including patient name and/or unique identifier, the date, the location of the scanned image as an icon or text, as well as other information about the mechanics of the scan (depth, Time-Gain Compensation settings probe MHz, and frame rate). Ideally, the machine would allow for digital storage of images in addition to the standard printer port for creation of small black and white glossy prints.
For most surgeons, the main criterion for deciding which machine to purchase is whether the unit needs to be portable. This is important because it is essential to have access to a suitable high-quality unit in the operating room. Although many hospitals have ultrasound equipment available for use in the operating room, the unit may be cumbersome to transport from the radiology department, or, if already available in the operating suite, may not have a suitable probe for breast scanning. The availability of intraoperative ultrasound is important not only for margin assessment and localization of nonpalpable lesions, but also because it provides an excellent venue to develop and to continue to improve ultrasound skills. The ability to visualize gross anatomic and pathologic findings minutes after performing a scan provides immediate feedback about interpretation of the study and can considerably shorten the learning curve for new users and improve skills of more experienced imagers.
Portability is also an important consideration for surgeons working in multiple office locations. In a small office or clinic, however, it is often easier to dedicate an exam room to ultrasound scanning than to move the scanner from room to room, because it is disruptive to patient flow and because of the other room modifications listed below. Fortunately, there is little, if any, significant difference in quality between the portable and fixed ultrasound machines available today. Figure 32-1 shows 2 state-of-the-art machines available today, which are comparable with regard to scanning features and quality and are in the same price range.1,2
The optimal location for an ultrasound machine in the breast clinic is almost always in the room where most breast patients are examined. There is a strong inclination to locate a newly acquired ultrasound machine in the “procedure room” where there already may be other equipment, such as suction or cautery. For breast ultrasound, however, this is not necessarily the best location because of the benefits of ready access to ultrasound scanning for evaluation of almost any breast problem. In most busy surgical practices, if the ultrasound equipment is not available for immediate scanning, the opportunity to perform the ultrasound is lost. Instead, it is better to make small modifications to a standard office examination room to make it suitable for diagnostic scanning as well as for most percutaneous ultrasound-guided procedures. Figure 32-2 shows how a stationary ultrasound unit can be located in a typical 10 × 12 ft examination room and still leave space for a console to perform percutaneous procedures.
Figure 32-2
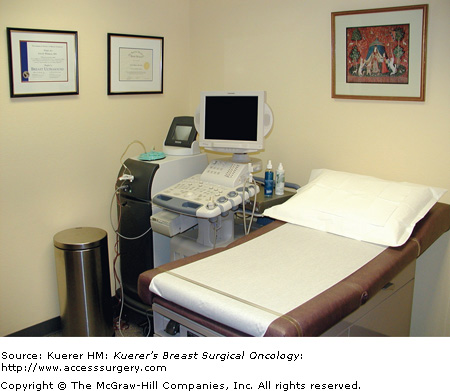
A standard 10 × 12 ft examination room will accommodate a fixed ultrasound machine and still have room for a console to perform vacuum-assisted biopsies or other percutaneous procedures. It is generally preferable to locate the ultrasound unit where most patients are examined and then make small modifications to accommodate the scanner and to perform percutaneous ultrasound-guided procedures. (Note the large wastebasket, which is useful if procedures are performed due to the large amount of disposable material generated.)
In addition to the ultrasound unit, which should include a small printer to record selected images from the scanning process, it is essential to have an x-ray view box in the room to be able to compare outside imaging studies with the real-time ultrasound scan. Also, because an increasing number of outside studies are available on CD-ROM instead of printed film, it is important to consider equipping the room with a computer with a CD/DVD drive and high-quality monitor. The ability to compare the live scan with outside studies (as well as your own prior imaging) is critical for accurate interpretation of the imaging and its correlation with the history and physical examination.
A gel warmer is an inexpensive addition that patients will greatly appreciate. Removing the gel after the scan is also an important and often overlooked issue—the doctor can easily rinse hands at the sink, whereas a patient will require soft paper or cloth wipes to remove the gel from the breast. Gowns or capes made from soft cloth, instead of the traditional paper, are a nice addition to the examination overall and can be used later by patients to help remove gel.
If you are planning to perform ultrasound-guided procedures, then the room should have adequate storage space for supplies. For convenience and safety, you must also ensure disposal and waste bins large enough to accommodate the supplies you will use. Figure 32-3 shows that a small work light installed over the sink is useful to help an assistant work when the room lights are dimmed and can double as a room “dimmer” if the room is not equipped with a rheostat to dim the lights for better viewing of the ultrasound image.