Section VI Chemotherapy of Hematologic Malignancies Chemotherapy for Childhood Leukemia
Barbara A. Gruner
The dramatic improvement in outcome for children with acute lymphoblastic leukemia (ALL) has been one of the great success stories in medicine over the last 50 years. ALL is the most common childhood malignancy with an annual incidence of 32 per 1,000,000 in people under 19 years. It represents over one-fourth of all childhood cancers and three-quarters of childhood leukemias. The 5-year survival rates for ALL in people under 19 years have improved from 54.1% in the mid-1970s to 85.9% in the mid-20005.1 This improvement has been the result of more uniform disease classification, development of risk-based therapy, better understanding of ALL biology, and the use of more effective agents and treatments from cooperative group clinical trials.
CLASSIFICATION AND RISK ASSESSMENT
In 1993, standardized risk criteria for precursor-B cell ALL were established at a workshop sponsored by the Cancer Therapy Evaluation Program (CTEP) of the National Cancer Institute (NCI). Based on the data from the Children’s Cancer Group (CCG), the Pediatric Oncology Group (POG), St. Jude Children’s Research Hospital (St. Jude), and Dana-Farber Cancer Institute (Dana-Farber), risk groups were determined by patient age and WBC count at diagnosis. Children between 1 and 9.99 years with a WBC count <50,000 defined the standard-risk group, and children 10 years and older or children of any age with a WBC count ≥50,000 defined the high-risk group.2 The risk classification described above applies to precursor B-cell ALL and not to T-cell ALL or mature B-cell ALL. At the 1993 workshop, the participants could not agree on whether T-cell ALL risk groups should be assessed by age and WBC count because the participants approached T-cell disease differently. St. Jude and POG treated T-cell ALL as a separate disease while CCG and Dana-Farber treated both immunophenotypes on the same protocols, although T-cell ALL patients were classified as high-risk on the Dana-Farber protocols.2 The outcomes for patients with T-cell ALL at that time were similar among the different treatments. When the Children’s Oncology Group (COG) analyzed the results from recent POG and CCG trials, they demonstrated that the outcome of T-cell ALL patients treated on POG trials was better for lower risk age and WBC count3 and equivalent for the higher risk group.4 By the mid-1990s, patients with mature B-cell ALL were treated like patients with advanced stage Burkitt lymphoma, which resulted in improved outcome.5,6 Additional clinical and laboratory data that further refined the risk groups for precursor B-cell ALL included the presence or absence of CNS leukemia or testicular disease, cytogenetic analysis, and response to induction therapy2,7
Patients with extramedullary disease were considered a higher risk subgroup because of a greater disease burden. In addition, the blood-brain or blood-testicle barrier protected leukemia in the CNS or testes. Disease in these sanctuary sites required more aggressive treatment, including radiation therapy8 Patients whose cytogenetic analysis showed the presence of trisomies 4, 10 and 179 or TEL-AML fusion10 were considered a low-risk subgroup due to their better treatment response. Children with MLL rearrangement, commonly associated with infant ALL, were considered a high-risk subgroup because these rearrangements were associated with high-risk features such as high WBC count or slow response to induction therapy.11 Those patients with the Philadelphia chromosome (t-(9;22), Ph+), commonly associated with adult ALL, were considered to be the highest risk group because of their poor outcome regardless of age or WBC count.12,13
CURRENT THERAPY FOR PRECURSOR B-CELL ALL
Treatment for ALL lasts about 3 years and consists of three phases: induction, consolidation, and maintenance with CNS protective therapy given throughout the treatment. Induction therapy is the most intensive phase of therapy and is usually 4 to 6 weeks in length. The object of induction is to place the patient in a complete remission, which means no detectable evidence of leukemia in the bone marrow (<5% lymphoblasts or M1), or extramedullary sites, and normalization of peripheral blood counts.14,15 For children in the NCI-standard-risk group, three drugs are used for systemic therapy: vincristine, asparaginase, and a corticosteroid. Vincristine is given intravenously weekly for four doses. The corticosteroid used for standard-risk patients is dexamethasone daily for 28 days. Polyethylene glycol-conjugated asparaginase (PEG-asparaginase) is given as an intramuscular injection on day 4. For those in the NCI-high-risk group, daunomycin, given intravenously weekly for four doses, is added and the steroid is prednisone daily for 28 days. PEG-asparaginase is used rather than native asparaginase, because it is equally effective and less immunogenic.16 Although dexamethasone provides better CNS protection than prednisone,17 patients older than 10 years have a higher incidence of osteonecrosis with dexamethasone,18 so prednisone becomes the steroid of choice. These regimens produce a >95% remission rate by the end of induction therapy.
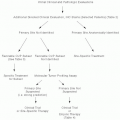
During induction, response to treatment is measured at day 8 or 15, at day 29 and, if needed, at day 43. Children with an M1 marrow at day 8 or day 15 are considered rapid early responders
(RER). Children with an M3 marrow (more than 25% lymphoblasts) on day 8 or an M2 (5% to 25% lymphoblasts) or M3 marrow on day 15 are considered slow early responders (SER). Rapid responders have a better event-free survival (EFS) than slow responders.6 Children who have an M2 marrow on day 29 receive an additional 2 weeks of four-drug therapy. If they achieve remission on day 43, they are nonrandomly assigned to the most intensive arm of treatment. If they have an M3 marrow on day 29 or an M2 or M3 marrow on day 43, they are considered to have failed induction and receive treatment on a regimen for very high-risk patients. A rapid responder receives standard therapy for consolidation and maintenance and a slow responder receives augmented therapy.
(RER). Children with an M3 marrow (more than 25% lymphoblasts) on day 8 or an M2 (5% to 25% lymphoblasts) or M3 marrow on day 15 are considered slow early responders (SER). Rapid responders have a better event-free survival (EFS) than slow responders.6 Children who have an M2 marrow on day 29 receive an additional 2 weeks of four-drug therapy. If they achieve remission on day 43, they are nonrandomly assigned to the most intensive arm of treatment. If they have an M3 marrow on day 29 or an M2 or M3 marrow on day 43, they are considered to have failed induction and receive treatment on a regimen for very high-risk patients. A rapid responder receives standard therapy for consolidation and maintenance and a slow responder receives augmented therapy.
An increasingly important marker of response to treatment is minimal residual disease (MRD) measured in the peripheral blood on induction day 8 and in the bone marrow at the end of induction. Children with negative MRD at the end of induction consistently have better EFS than those with positive MRD, regardless of risk group or therapy. Those with negative MRD on day 8 also had better outcomes than those with positive MRD.19 MRD at the end of induction identifies patients who would benefit from either less intensive or augmented therapy and is used in treatment assignment on the current COG clinical trials. In the future, the day 8 peripheral blood MRD may replace the day 8 bone marrow aspiration for response assessment.
For ongoing COG trials, response to induction combines marrow response and day 29 MRD. Patients who are rapid responders to induction therapy (Ml marrow by day 15 of induction) and have negative residual disease (MRD <0.1% at day 29) are treated in a lower or average risk subgroup, depending upon the cytogenetic features of their disease. Patients who are SER in induction therapy (M2 or M3 on day 15 of induction) or have intermediate levels of residual disease (MRD between 0.1% and 1%) have a poorer overall outcome and were treated in the higher risk subgroup. The children who are in the higher risk subgroup receive more intensive treatment than those who are in the lower or average risk subgroups. The small numbers of patients who fail induction or have high levels of residual disease at the end of induction (MRD >1%) are considered the highest risk patients because of their very poor outcome.6
Postinduction intensification has led to significant improvements for ALL patients regardless of risk group. The importance of intensifying treatment was demonstrated by a CCG trial comparing two regimens that intensified therapy; one was a modification of the Berlin-Frankfurt-Munster (BFM) 1976 regimen and the other, the New York regimen, with a regimen which did not intensify therapy in the treatment of high-risk ALL patients.20 The modified BFM regimen added an intensive consolidation immediately after induction and inserted a combined 3 weeks of induction with 4 weeks of the intensified consolidation (delayed intensification) immediately following 8 weeks of maintenance (interim maintenance) to the nonintensified treatment. The New York regimen, a modified LSA2L2 regimen, was intensive throughout the entire treatment. Owing to the clear inferiority of outcomes for children on the nonintensified therapy, it was closed 21 months after the start of the trial. The two intensive regimens had similar EFS (63% vs. 61% at 7 years), but the modified BFM therapy used lower cumulative doses of anthracycline and alkylating agents and had a lower morbidity than the New York regimen. The modified BFM regimen became the standard for high-risk ALL therapy in CCG.
In a later trial, the high-risk treatment was further intensified for slow responders with an augmented consolidation and two cycles of augmented interim maintenance alternating with two cycles of delayed intensification.21,22 Children receiving augmented therapy had greatly improved EFS compared with those receiving standard therapy (75% vs. 55% at 5 years). Although an augmented regimen was also shown in a successor trial to benefit rapid responders, there was no advantage in adding a second interim maintenance and a second delayed intensification.23
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree