For initial staging and at end of treatment to document remission status, PET is the standard imaging modality. Interim scanning remains investigational. Surveillance PET is not beneficial in the majority of patients. PET has also been used to predict outcome in the pre-autologous transplant setting. PET in the pre-allogeneic setting has a less established benefit. There is limited data on its use after transplant.
Key points
- •
Positron emission tomography (PET) is standard of care at diagnosis and for determining remission status at the end of treatment, but remains investigational when performed in the middle of therapy.
- •
Surveillance PET is not beneficial in the majority of patients.
- •
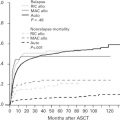
PET pre-auto hematopoietic stem cell transplant is prognostic of outcome.
- •
Improvements in interpretation and standardization of PET across institutions, and the use of new tracers, can improve this modality.
Introduction
Positron emission tomography-low dose computed tomography with 18F-fluorodeoxyglucose (PET) has become a valuable imaging modality studied at all stages of diffuse large B-cell lymphoma (DLBCL) management. In 2007, the first guidelines for the use of PET in lymphoma were presented by the International Harmonization Project and incorporated into response criteria. In an effort to standardize the results of PET scans, a 5-point scale, known as the Deauville criteria, was accepted in 2009. Consensus guidelines were then most recently updated in 2013 and known as the Lugano Classification. This article discusses the literature at each phase of treatment including the role of PET scans periautologous and allogeneic hematopoietic stem cell transplant (HSCT) and newer semiquantitative measurements such as metabolic tumor volume.
Introduction
Positron emission tomography-low dose computed tomography with 18F-fluorodeoxyglucose (PET) has become a valuable imaging modality studied at all stages of diffuse large B-cell lymphoma (DLBCL) management. In 2007, the first guidelines for the use of PET in lymphoma were presented by the International Harmonization Project and incorporated into response criteria. In an effort to standardize the results of PET scans, a 5-point scale, known as the Deauville criteria, was accepted in 2009. Consensus guidelines were then most recently updated in 2013 and known as the Lugano Classification. This article discusses the literature at each phase of treatment including the role of PET scans periautologous and allogeneic hematopoietic stem cell transplant (HSCT) and newer semiquantitative measurements such as metabolic tumor volume.
Deauville criteria
The 5-point scale is depicted in Table 1 . One of the major values of this system is that it is reproducible between centers. In addition, it allows for altering the positive and negative thresholds in the context of a clinical trial. For example, to avoid undertreatment, a lower score would be considered negative. Similarly, a higher score can be used to define a positive scan to avoid overtreatment. More recently, definitions for the distinction between standardized uptake value (SUV) (ie, moderately or markedly [scores 4 and 5] greater than the liver) have been suggested, with scores of 5 applied when the uptake is 2 to 3 times greater than the maximum SUV (SUVmax) of the liver.
| Score | Definition |
|---|---|
| 1 | No uptake |
| 2 | Uptake ≤ mediastinum |
| 3 | Uptake > mediastinum but ≤ liver |
| 4 | Uptake moderately higher than liver |
| 5 | Uptake markedly higher than liver and/or new lesions |
| X | New areas of uptake unlikely to be related to lymphoma |
Initial staging
PET scanning with the accompanying low-dose computed tomography (CT) is uniformly agreed upon as more accurate than contrast enhanced CECT alone for initial staging of DLCBL due to increased sensitivity for both nodal and extranodal disease. One of the remaining questions is the use of CECT in addition to PET. There are no studies comparing PET with low-dose CT to PET with CECT. The main limitations include the availability of performing the dedicated CT at the same time and the cost of the additional study if it cannot be done simultaneously. When possible, the optimal recommendation is to have both studies at diagnosis for better anatomic staging, as the inclusion of CECT has been shown to upstage 10% to 25% of patients. However, as studies have not shown improved survival in those upstaged patients treated more aggressively, in patients who cannot have a CECT performed with the PET, a diagnostic CT is likely only needed in patients with localized disease for which precise anatomy needs to be defined for the consideration of radiotherapy.
Another remaining question is the ability to eliminate a bone marrow biopsy (BMBx) from routine staging work-up based on the results of the PET. Patients eligible for curative treatment are recommended to have a BMBx under the current guidelines. However, other authors suggest that not all patients require this procedure at diagnosis. The 2 main considerations include the pattern of involvement on the PET scan and the prognostic significance of the presence of concordant DLBCL versus discordant small cleaved cells histologically.
On PET scan, the marrow may have no, focal, or diffuse uptake, with each having a different association with a positive BMBx. Adams and colleagues conducted a meta-analysis of 7 studies, from which they concluded that a negative PET did not rule out the presence of lymphoma, but a focally or diffusely positive scan obviated the need for a biopsy given a pooled sensitivity and specificity of 88.7% (95% confidence interval, CI, 82.5%–93.3%) and 99.8% (95% CI 98.8%–100%), respectively. A subsequent retrospective study showed that 31% of patients with a negative PET had a positive BMBx, exemplifying the benefit of a biopsy in staging those with a negative marrow on PET. On the other hand, Khan and colleagues demonstrated that PET can identify all clinically important marrow DLBCL and that patients with a positive bone marrow (BM) identified by PET-CT but not BMBx had a progression-free survival (PFS) and overall survival (OS) similar to stage IV disease without marrow involvement.
Sehn and colleagues suggest that discordant marrow positivity does not impact OS as long as there is no change in the International Prognostic Index (IPI), while concordant BM involvement negatively affects both OS and PFS independently. As such, although marrow involved with discordant lymphoma may be missed by a false-negative PET scan, a patient’s overall course may be unchanged by omitting the BMBx.
Therefore, it would be reasonable for patients with negative or diffusely positive marrow by PET to undergo BM evaluation with aspirate, biopsy, and flow cytometry, while those with focal or focal and diffuse PET uptake would likely have marrow involvement and should be treated as such if a biopsy is omitted.
Interim
Interim PET scans (iPET) remain among the most controversial and least standardized uses of this modality in lymphoma management ( Table 2 ). Although the purpose would be to exclude progression and possibly individualize therapy based on response, several issues exist including timing of the scan, interobserver reproducibility without a standard definition of positive and negative, and false positivity due to inflammatory responses from immunotherapy.
| Reference | DLBCL Patients (n) | Type of Study | Treatment | # Cycles Before iPET | Median Follow-Up (mo) | iPET Negative | PPV | NPV | PFS w/Neg iPET | PFS w/Pos iPET | OS w/Neg iPET | OS w/Pos iPET |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cashen et al, 2011 | 52 | SC, R | R-CHOP-21 x6 | 2 | 33.9 | 52% | 42% | 77% | 2 yr: 85% | 2 yr: 63% | 2 yr: 85% | 2 yr: 65% |
| Cassanovas et al, 2011 | 113 | MC, P | R-CHOP or R-AVCBP | 2 & 4 | 19 | deltaSUV: after 2: 78%, after 4: 88% | NR | NR | 2 yr: after 2: 77%, after 4: 83% | 2 yr: after 2: 57%, after 4: 40% | 2 yr: after 2: 93%, after 4: 94% | 2 yr: after 2: 60%, after 4: 50% |
| Itti et al, 2010 | 80 | MC, P | CHOP or AVCBP ± Rituximab | 4 | 41 | deltaSUV: 78.7% | 70.6% | 79.4% | 2 yr: 79% | 2 yr: 32% | NR | NR |
| Kostakoglu et al, 2006 | 24/47 | SC, R | CHOP ± Rituximab x 6–8 | 1 | 21 | 45% | 75% | 100% | 2 yr: 100% | 2 yr: 12.5% | NR | NR |
| Lin et al, 2007 | 92 | MC, P | CHOP or AVCBP ± Rituximab | 2 | 42 | deltaSUV: 82.6% | 81.3% | 75% | 2 yr: 79% | 2 yr: 21% | NR | NR |
| Moskowitz et al, 2010 | 98 | SC, R |
| 4 | 44 | 61% (33/38 w/pos iPET had neg bx) | NR | NR | 2 yr: >90% | 2 yr: Neg bx 80%–85%, Pos bx 60% | NR | NR |
| Nols et al, 2014 | 73 | MC, R | R-CHOP or R-AVCBP | 3–4 | 28 | deltaSUV: 82% | 46% | 75% | 2 yr: 78% | 2 yr: 50% | 2 yr: 88% | 2 yr: 56% |
| Pregno et al, 2012 | 88 | MC, R | R-CHOP | 2–4 | 26.2 | 72% | 36% | 82.5% | 85% | 72% | NR | NR |
| Safar et al, 2012 | 112 | MC, P | R-CHOP or R-AVCBP | 2 | 38 | 62.5% | NR | NR | 3 yr: 84% | 3 yr: 47% | 3 yr: 88% | 3 yr: 62% |
| Yang et al, 2011 | 161 | SC, P | R-CHOP-21 x6-8 | 3–4 | 30 | 72% | NR | NR | 3 yr: 88.3% | 3 yr: 52.5% | 3 yr: 91.4% | 3 yr: 53.3% |
| Yoo et al, 2011 | 155 | MC, R | R-CHOP | 2–4 | 20 | 64.5% | 62% | 93% | 3 yr: 84% | 3 yr: 66% | 3 yr: 84% | 3 yr: 77% |
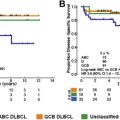
Two large meta-analyses have been recently published with conflicting results. Zhu and colleagues included 11 studies of DLBCL patients treated with rituximab-based immunochemotherapy who underwent scans after 2 to 4 cycles of therapy. They found that PFS was significantly shorter for those with a positive interim scan with a pooled hazard ratio (HR) of 2.96 (95% CI, 2.25–3.89). On the other hand, Sun and colleagues limited their analysis to patients receiving rituximab, cyclophosphamide, adriamycin, vincristine, and prednisone (R-CHOP). In 6 studies including 605 patients, the pooled sensitivity and specificity in predicting outcomes were 52.4% and 67.8%, respectively.
One explanation for the difference across studies is the variable time at which the scan is done, with PET scans after 2 cycles evaluating chemosensitivity and after 4 cycles possibly portraying regrowth of disease.
Studies have been done as early as after 1 cycle of chemotherapy, again with contradictory results. In a cohort of DLBCL and Hodgkin lymphoma patients, Kostakoglu and colleagues found that all patients with a negative PET after 1 cycle had a sustained remission with a median follow-up of 28 months. More recently, however, Mylam and colleagues report that in 112 DLBCL patients, there was no difference in PFS for PET-negative versus -positive patients when using a Deauville score of greater than 3.
Several suggestions have been evaluated to improve on the reproducibility of the interpretation beyond visual scales including semiquantitative measurements, such as ΔSUVmax and metabolic tumor volumes, or biopsy of the area with increased uptake.
The percent change in maximum SUV (ΔSUVmax) from baseline to the subsequent scan can be quantified and has been shown to improve interobserver agreement when compared with visual assessment. Thresholds predicting response vary between studies based on the time point of the scans and range from 66% to 92%. Lin and colleagues reported the first large quantitative study and found an optimal cutoff of 66% for PET done after 2 cycles of chemotherapy (PET2) using receiver operating characteristic (ROC) analysis. Patients with a ΔSUVmax greater than the cutoff had a 2-year event-free survival (EFS) of 79% compared with 21% in those with a lesser reduction ( P = .001). The same group found that for PET after 4 cycles of chemotherapy (PET4), the threshold increased to 73% with a 2-year EFS of 79 versus 32%, and concluded that while semiquantification after 2 cycles of chemotherapy reduced false-positive scans, it was equivalent to visual analysis after 4 cycles.
Other groups have also shown that ΔSUVmax is able to predict outcomes. Casasnovas and colleagues showed an OS benefit of 93% versus 60% ( P <.0001) with a PET2 ΔSUVmax cutoff of 66% and 94% versus 50% ( P <.0001) with a PET4 ΔSUVmax cutoff of 70%. On the other hand, using the same 66% threshold, Pregno and colleagues were unable to show a difference in outcome based on iPET after 2 to 4 cycles of therapy.
To evaluate changing treatment based on an unfavorable iPET, the PETAL (Positron Emission Tomography guided therapy of Aggressive non-Hodgkin Lymphomas) trial prospectively applied a ΔSUVmax threshold of 66% on PET2 with patients not meeting the cutoff escalated to a Burkitt-like regimen. With 926 patients, iPET was unfavorable in 13% and highly predictive of outcome with a 2-year time to treatment failure of 79% versus 47% ( P <.0001), but they were unable to show a benefit to switching therapy. The GAINED (GA in Newly Diagnosed Diffuse Large B-cell Lymphomas) trial and the UK Clinical Research Network iPET study are ongoing.
Other semiquantitative approaches under investigation include the use of metabolic tumor volume (MTV) and total lesion glycolysis (TLG), with prognostic significance both at diagnosis and at interim restaging. MTV is defined as the volume of hypermetabolic tissue with an SUV greater than a threshold value of 2.5 (MTV2.5) and is thought to better represent tumor burden by measuring the viable tumor fraction. TLG goes 1 step further and quantifies the metabolic disease burden by multiplying the glucose utilization rate (SUVmean) and the MTV. Yang and colleagues compared the ΔMTV2.5 with the Deauville 5-point scale and ΔSUVmax in 186 patients after 3 to 4 cycles of R-CHOP and found that patients with a worse scan by each method had a shorter PFS. In addition, when given a point for each method patients scored positively in, any score greater than zero predicted for worse outcomes. Interestingly, the mean MTV2.5 reduction rate on the iPET was not significantly different between patients who relapsed and those who did not (98.2 vs 93%). Using ROC analysis, they determined that the ΔMTV2.5 cutoff for interim scanning was 99.3% and found a 2-year PFS of 84.2 versus 64.9% for those above and below the threshold, respectively. Similarly, Malek and colleagues retrospectively evaluated iPET after 2 to 4 cycles of R-CHOP or dose-adjusted R-EPOCH in 140 patients. In their ROC analysis, the ΔMTV was 52% with an HR of 1.37 ( P = .02) for PFS when comparing achieving a ΔMTV greater than 52% versus less than 52%. Given the wide variation in ΔMTV thresholds, further research is clearly necessary to determine the optimal cutoff for this methodology.
Histologic confirmation of areas of increased SUV on interim scans can help increase the accuracy of interpretation if therapy changes are being considered based on the results. However, Moskowitz and colleagues found that 33 of 38 patients with positive iPET had a negative biopsy, and their outcome was similar to the PET-negative patients. The use of an induction/consolidation strategy with all patients receiving escalated immunochemotherapy and the timing of the scan may have contributed to the high false-positive rate. Therefore, this strategy is limited by the possibility of subjecting many patients to unnecessary biopsies when their scan positivity was based visual scales.
Finally, the use of an alternative tracer,18F-fluorodeoxythymidine (FLT), may allow for better early discrimination of inflammation versus tumor proliferation. Minamimoto and colleagues conducted a prospective multicenter study evaluating which of FDG or FLT PET after 2 cycles of chemotherapy was better able to predict response after 6 cycles. They found FLT iPET had a significantly higher positive predictive value (PPV), but similar negative predictive value. On the other hand, Schoder and colleagues prospectively used FLT PET in the induction/consolidation DLBCL patients and showed that while FLT PET predicts PFS and OS, the PPV too low to justify changes in therapy. Additional investigations remain ongoing to improve this methodology.
Overall, even if these issues are solved, the number of scans a patient will have in a few months’ span and the cost of these scans without significant benefit remain problems. In addition, there are little data supporting improved outcomes with a risk-adapted treatment strategy. Therefore, interim PET for DLBCL is not recommended outside the context of a clinical trial.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree