Summary of Key Points
- •
Many meta-analyses, outcomes and matched cohort studies demonstrate equal long-term outcomes for video-assisted thoracoscopic surgery (VATS) and open lobectomy.
- •
Matched comparisons generally demonstrate equal long-term survival for VATS versus open lobectomy for lung cancer, suggesting that the improved survival seen in unmatched studies is due to confounding factors.
- •
Many meta-analyses, outcomes, and matched cohort studies demonstrate similar operative mortality for VATS and open lobectomy.
- •
Pain, hospital length of stay, and complications are lower after VATS than after open lobectomy.
- •
There is no difference in the incidence of N2 nodal upstaging; the effect on N1 upstaging is unclear.
- •
The ability to deliver adjuvant chemotherapy may be better after VATS lobectomy.
- •
VATS lobectomy is associated with a learning curve of about 50 cases.
Over 100 years ago, Jacobaeus first reported the diagnosis and treatment of pleural effusions using a thoracoscope. Since then, the application of thoracoscopy to pulmonary resection has advanced as a useful adjunct for surgeons, perhaps most prominently for wedge resection or pleural procedures. From the late 1980s to the 1990s, surgeons began using VATS for lobectomies to treat patients with early stage nonsmall cell lung cancer (NSCLC). In 1992, VATS simultaneously stapled lobectomy without rib spreading was reported by Lewis et al. and with individual vessel and bronchial ligation was reported by Roviaro et al. During the following year, the outcomes of VATS lobectomy were published by Walker et al., Coosemans et al., Kirby et al., and Hazelrigg et al. The surgical approach has become far less invasive as the instrumentation has gradually improved over the past two decades and VATS has evolved into a basic and vital thoracic surgical technique.
However, the penetration of VATS anatomic resections (lobectomy and segmentectomy) has been slow to occur, and currently about 30% of anatomic resections in the United States are performed using VATS. These VATS lobectomies in the United States are performed primarily by dedicated thoracic surgeons. As reported in the database of the Society of Thoracic Surgeons (STS), which represents predominantly dedicated thoracic surgeons in the United States, the proportion of lobectomies done via VATS has increased from 19% in 2005 to 44% in 2009 and is currently 66%. A similar increase from 20% to 54% from 2007 to 2011 has been reported in Denmark, which has a highly centralized health-care system. Robust data about the overall proportion of lobectomies that are performed using VATS in Europe or Asia are not available, but estimates put this well below the penetration currently seen in the United States.
Definitions
Video-assisted thoracoscopic surgery (VATS) is used for wedge resection, segmentectomy, lobectomy, pneumonectomy, sleeve lobectomy, lobectomy with chest wall resection, and extrapleural pneumonectomy. The approaches vary substantially: reports on VATS lobectomy alone describe the use of one to six incisions from 4 cm to 10 cm in length, with and without rib spreading. In general, however, VATS lobectomy is interpreted to mean an anatomic lobectomy with ligation of individual bronchi and vessels and lymph node dissection or sampling using a minimal number of ports without a retractor or rib spreading.
A clear definition of VATS lobectomy is needed. The Cancer and Leukemia Group B established a definition of VATS lobectomy for a prospective, multi-institutional trial, and this definition has been widely adopted. A VATS lobectomy is defined as involving no rib spreading; maximum incisions of 8 cm; dissection of individual veins, arteries, and airways for the lobe in question; and node sampling or dissection identical to open thoracotomy. This definition was endorsed by most of the 55 experts participating in the 20th Anniversary of VATS Lobectomy Conference: The Consensus Meeting, organized by the Scientific Secretariat and the International Scientific Committee of the International VATS Lobectomy Consensus Group. However, several participants thought that a small retractor should be acceptable in specific circumstances, for example, when performing complex procedures such as bronchoplasty or when delivering a large specimen.
Some surgeons have suggested that VATS should include only procedures done exclusively with visualization on a monitor. This criterion should be abandoned for several reasons. The most important issues for patients with malignant diseases are the incisional trauma, achievement of curative surgery, and subsequent oncologic outcomes. Occasional viewing through a 4-cm, non–rib-spreading incision does not change the nature of the procedure. A hybrid VATS approach using both a monitor and direct vision without rib spreading or a robotic approach can provide a three-dimensional understanding of anatomy as well as magnified proximity visualization and would surely clinically facilitate complex procedures such as sleeve lobectomy or segmentectomy.
Technical aspects of how to accomplish a VATS lobectomy are beyond the scope of this chapter and are the subject of surgical atlases. Styles vary in how surgeons perform different steps of the operation. The essential feature, however, is a hilar dissection and individual division of the vessels and bronchus of the lobe. Most often, these structures are divided using an endostapler, but ligation, division between clips, or sealing with energy devices is also feasible for smaller vessels.
Patient Selection
Patient selection ultimately depends on the surgeon’s judgment about the ability to accomplish an oncologically appropriate resection of a given patient’s tumor. However, some general guidance can be obtained from the opinions of experts at the recent Consensus Meeting ( Table 27.1 ). Most of these experts consider VATS to be appropriate for stage I and II tumors unless there is substantial hilar involvement or the need for chest wall, bronchial, or vascular sleeve resection.
| Indications for VATS Lobectomy | |
| ≤7 cm (T1, T2a, and T2b) | Recommended |
| N0 or N1 status | Recommended |
| Patients with previous thoracic surgery or pleurisy | Highly recommended |
| Contraindications for VATS Lobectomy | |
| Chest wall involvement including rib(s) | Contraindicated |
| Central tumor invading hilar structure(s) | Contraindicated |
| FEV 1 <30% | Contraindicated |
| DLCO <30% | Contraindicated |
| Preoperative Investigations | |
| PET/CT and sampling of positive mediastinal lymph nodes | Highly recommended |
| Sampling of positive lymph nodes by EBUS/EUS | Recommended |
| VATS assessment at the time of surgery | Highly recommended |
| Total ipsilateral lymph node dissection in all patients | Recommended |
| Indications for Conversion to Open Thoracotomy | |
| Major bleeding | Highly recommended |
| Significant chest wall involvement | Recommended |
| Vascular sleeve | Highly recommended |
| Bronchial sleeve | Highly recommended |
| Bronchovascular sleeve | Highly recommended |
| Training | |
| Number of cases to overcome steep learning curve: 50 | Highly recommended |
| Resident case volume of a training center: >50/y | Recommended |
| Minimum case volume to maintain VATS skills: >20/y | Recommended |
| Proctoring should be necessary in all new VATS surgeons | Highly recommended |
| Future Directions | |
| Establishment of multi-institutional database | Recommended |
| Increased exposure of VATS lobectomy to trainees | Highly recommended |
| Establishment of standardized VATS lobectomy workshops | Highly recommended |
Outcomes: Comparison of Vats and Open Lobectomy
The scope of what can be successfully performed thoracoscopically includes pneumonectomy, segmentectomy, sleeve lobectomy, and lobectomy with chest wall resection. However, the literature is too limited for most of these procedures to define outcomes, and the results are confounded by patient selection, making assessment of the impact of the VATS approach per se difficult at best.
By contrast, the literature on VATS lobectomy for cancer is so abundant that we have chosen to focus our review on meta-analyses and large outcomes studies. Only a few randomized controlled trials were conducted; these were early in the VATS experience and were small, underpowered studies. As the procedure matured and experience grew, increasing amounts of nonrandomized data showed that VATS lobectomy for cancer was safe, with outcomes similar to or better than those of open lobectomy. In the United States, the decision was made that a randomized controlled trial of VATS compared with open lobectomy would require a design to prove equivalence, which would necessitate too many patients and would not be worth the expense. Hence, the strongest data come from large outcomes and propensity-matched studies and not randomized controlled trials.
To provide an evidence base for this chapter, a comprehensive literature search was carried out for studies comparing VATS with open lobectomy or segmentectomy for lung cancer. We included reports that involved a meta-analysis, a randomized controlled trial, a propensity-matched or otherwise case-matched study, or an outcomes study using a large multi-institutional database. We did not include reports of individual, single-institution comparative series without case matching. Two systematic reviews were not included because a quality assessment judged them to be poor, and they included studies that were otherwise already captured. One meta-analysis was excluded because it focused only on three propensity-matched studies, which were already included individually. Another was excluded because it used an erroneous code for VATS lobectomy.
Short-Term Outcomes
The results of many studies have demonstrated that VATS lobectomy is a safe procedure ( Table 27.2 ). These studies, including meta-analyses, propensity-matched series, case-matched series, and randomized controlled trials, demonstrate that the conversion rate from VATS to open procedure is about 5% to 10%. Most of these conversions resulted from oncologic or technical factors; bleeding was the reason for conversion in only a few studies. Furthermore, conversion from VATS to an open procedure is not associated with increased perioperative mortality or complications when compared with planned open thoracotomy.
| First Author | Year | N (Total) | Inclusion Criteria, Comments | Conversion Rate % | Operative Mortality % | Complications (Overall) % | Hospital Stay (Days, Median) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| VATS | Open | p | VATS | Open | p | VATS | Open | p | |||||
| Meta-Analyses | |||||||||||||
| Cheng | 2007 | 3589 | About 20% rib spr | 6 | 1.2 | 1.7 | NS | 13 | 20 | 0.0002 | Lower | — | 0.007 |
| Chen | 2013 | 3457 | Stage I | — | — | — | — | 20 | 29 | <0.0001 | Lower | — | <0.01 |
| Yan | 2009 | 2641 | 20% Rib spr | 8 | 0.4 | 0.7 | NS | — | — | — | 12 | 12 | — |
| Cai | 2013 | 1564 | Stage I | — | — | — | — | Lower | — | 0.013 | — | — | — |
| Propensity-Matched Series | |||||||||||||
| Paul | 2013 | 41,039 | NIS | — | 1.6 | 2.3 | NS | 41 | 45 | <0.001 | 5 | 7 | <0.001 |
| Yang | 2016 | 18,780 | NCDB | — | 1.5 | 1.8 | NS | — | — | — | 5 | 6 | <0.01 |
| Falcoz | 2016 | 5442 | ESTS DB | — | 1.0 | 1.9 | 0.02 | 29 | 32 | <0.04 | 6 | 8 | 0.0003 |
| Cao | 2013 | 3634 | — | 1.3 | 1.8 | NS | 25 | 35 | 0.0001 | Lower | — | <0.00001 | |
| Cao | 2013 | 2916 | Chinese DB | 8 | 0.8 | 1.1 | — | — | — | — | — | — | — |
| Paul | 2010 | 2562 | STS | — | 0.9 | 1 | NS | 26 | 35 | <0.0001 | 4 | 6 | <0.0001 |
| Scott | 2010 | 752 | Stage cI | — | 0 | 1.6 | NS | 27 | 48 | NS | 5 | 7 | <0.001 |
| Flores | 2009 | 741 | Stage cIa | 18 | 0.3 | 0.3 | NS | 24 | 30 | 0.05 | 5 | 7 | <0.001 |
| Villamizar | 2009 | 568 | Prospective DB | 5 | 3 | 5 | 0.02 | 31 | 49 | — | 4 | 5 | <0.0001 |
| Lee | 2013 | 416 | Cornell U | 2 | 1 | 3 | NS | 15 | 18 | — | 4 | 5 | 0.02 |
| Ilonen | 2011 | 232 | Stage cI | 14 | 2.6 | 3.4 | NS | 16 | 27 | <0.03 | 8 | 11 | 0.001 |
| Jeon | 2013 | 182 | COPD, Stage cI | 11 | 0 | 3.3 | NS | 22 | 33 | NS | 6 | 9 | 0.04 |
| Scott | 2010 | 136 | Stage cI | 7 | 1.4 | 1.6 | NS | 34 | 39 | NS | 4 | 7 | <0.0001 |
| Yang | 2016 | 60 | Preop chemo | — | 3 | 7 | NS | 40 | 57 | NS | 4 | 5 | 0.007 |
| Case-Matched Series | |||||||||||||
| Cattaneo | 2008 | 164 | Elderly | 1 | 0 | 3.6 | NS | 28 | 45 | 0.04 | 5 | 6 | 0.001 |
| Jones | 2008 | 78 | Converted | 11 | 0 | 2 | NS | 50 | 48 | NS | 8 | 8 | NS |
| Demmy | 1999 | 38 | Old, frail | 14 | 16 | 5 | — | 32 | 32 | — | 5 | 12 | 0.02 |
| Outcomes Studies (Adjusted Data) a | |||||||||||||
| Ceppa | 2012 | 12,970 | STS | — | — | — | — | Lower | 0.001 | — | — | — | |
| Ceppa | 2012 | — | Hi pulm risk | — | — | — | — | Lower | 0.02 | — | — | — | |
| Farjah | 2009 | 12,958 | SEER Medicare | — | Lower | — | NS | — | — | — | 4 | 8 | <0.001 |
| Park | 2012 | 6292 | NIS | — | — | — | NS | Lower | 0.004 | Lower | — | 0.001 | |
| Swanson | 2012 | 3961 | Premiere DB | — | — | — | — | Lower | 0.02 | 6 | 8 | <0.0001 | |
| Licht | 2013 | 1513 | Stage cI. DLCR | — | 1.1 b | 2.9 b | 0.02 b | — | — | — | — | — | — |
| Randomized Controlled Trials | |||||||||||||
| Craig | 2001 | 110 | — | — | 0 | 0 | NS | 3 | 8 | — | (9) c | (8) c | (NS) c |
| Kirby | 1995 | 55 | Stage cI | 10 | — | — | — | 24 | 53 | <0.05 | 7 | 8 | NS |
a Reported data are that adjusted for multiple predictive factors (multivariate analysis).
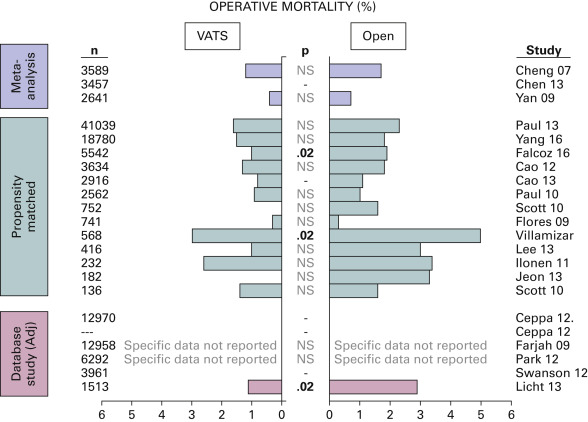
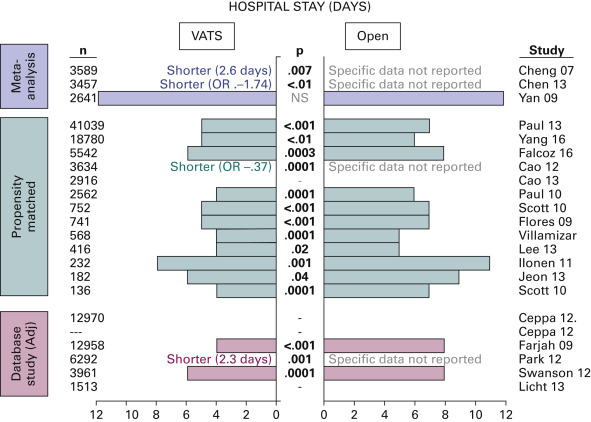
The studies included in this review ( Table 27.2 ) almost universally show no significant difference in perioperative mortality between VATS and open lobectomy ( Fig. 27.1 ). Closer examination shows that, in fact, the trend to lower perioperative mortality rates with VATS is consistent. This lower mortality rate is true even among special populations of patients (e.g., older, frail, high pulmonary risk) in case-matched series. The length of hospital stay has been significantly lower for VATS resection in most studies ( Fig. 27.2 ). The difference is approximately 1 day to 3 days, on average. Comparison between studies is difficult, however, because the average length of stay varies markedly, most likely reflecting differences in regional standards and the structure of the health-care system.
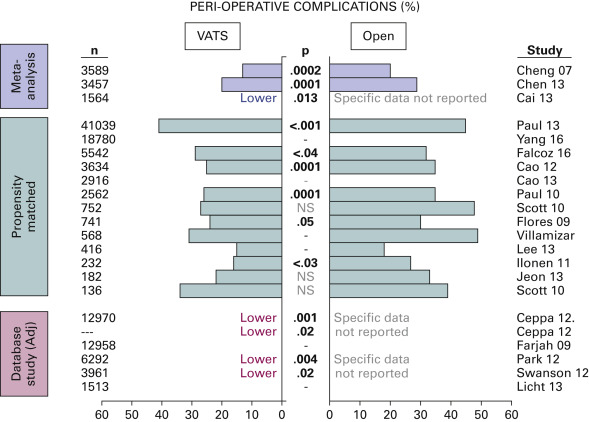
The overall rate of complications is also significantly lower in VATS resection in most studies ( Table 27.2 , Fig. 27.3 ). Comparison of complications among studies is difficult because of the varying definitions of a complication and the degree of severity of complications that were counted. Certain specific relevant complications have been reported in some studies ( Table 27.3 ). A fairly consistent trend toward lower rates of pneumonia, prolonged air leak, arrhythmia, and need for postoperative mechanical ventilation has been demonstrated, with the difference being significant in less than half of the studies.
| First Author | Year | N (Total) | Inclusion Criteria, Comments | % Pneumonia | % Prolonged Air Leak | % Arrhythmia | % Mechanical Ventilation | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| VATS | Open | p | VATS | Open | p | VATS | Open | p | VATS | Open | p | ||||
| Meta-Analyses | |||||||||||||||
| Cheng | 2007 | 3589 | ~20% Rib Spr | Lower | NS | Higher a | NS | Same | Same | NS | Lower | NS | |||
| Chen | 2013 | 3457 | Stage I | 2 | 5 | 0.03 | 5 | 7 | NS | 10 | 12 | NS | — | — | — |
| Yan (all) | 2009 | 2641 | 20% Rib Spr | 2 | 10 | NS | 5 | 6 | NS | 10 | 10 | NS | — | — | — |
| Cai | 2013 | 1564 | Stage I | Lower | — | NS | Lower | — | NS | Lower | — | 0.05 | — | — | — |
| Yan (no Rib Spr) | 2009 | 925 | No Rib Spr | 0.5 | 2 | NS | 2 | 2 | NS | 4 | 4 | NS | — | — | — |
| Propensity-Matched Series | |||||||||||||||
| Paul | 2013 | 41,039 | NIS | 7 | 8 | NS | — | — | — | 14 | 18 | <0.001 | 5 | 6 | NS |
| Falcoz | 2016 | 5442 | ESTS | 6 | 6 | NS | 10 | 9 | NS | 5 | 5 | NS | 0.7 | 1.4 | <0.008 |
| Cao | 2013 | 3634 | 3 | 5 | 0.008 | 8 | 10 | 0.02 | 7 | 12 | <0.00001 | — | — | — | |
| Paul | 2010 | 2562 | STS | 3 | 4 | NS | 8 | 9 | NS | 7 | 12 | 0.0004 | 0.5 | 0.6 | NS |
| Scott | 2010 | 752 | Stage cI | — | — | — | 2 | 7 | NS | 9 | 13 | NS | 0 | 4 | — |
| Flores | 2009 | 741 | Stage cIa | — | — | — | 4 | 4 | NS | 10 | 11 | NS | — | — | — |
| Villamizar | 2009 | 568 | Prospective DB | 5 | 10 | 0.05 | 13 | 19 | 0.05 | 13 | 21 | 0.01 | — | — | — |
| Lee | 2013 | 416 | Cornell U | 1 | 3 | — | 6 | 6 | — | 6 | 6 | NS | 1 | 3 | — |
| Ilonen | 2011 | 232 | Stage cI | 4 | 3 | — | 4 | 10 | — | 1 | 3 | — | 0 | 1 | — |
| Jeon | 2013 | 182 | COPD, Stage cI | 1 | 11 | 0.01 | 11 | 15 | NS | 8 | 9 | NS | — | — | — |
| Yang | 2015 | 60 | Preop chemo | 7 | 13 | NS | 10 | 20 | NS | 23 | 23 | NS | 0 | 3 | NS |
| Outcomes Studies (Adjusted Data) b | |||||||||||||||
| Ceppa | 2012 | 12,970 | STS | 3 c | 5 c | <0.001 | — | — | — | — | — | — | 0.4 c | 0.8 c | 0.002 |
| Swanson | 2012 | 3961 | Premiere DB | Same | Same | NS | Lower | — | NS | Lower c | — | — | — | — | — |
| Randomized Controlled Trials | |||||||||||||||
| Craig | 2001 | 110 | — | 0 | 6 | — | — | — | — | 0 | 2 | — | 2 | 0 | — |
| Kirby | 1995 | 55 | Stage cI | — | — | — | 12 | 27 | NS | — | — | — | — | — | — |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







