Chapter 49 Rectal Cancer
Etiology and Epidemiology
The etiology of colorectal cancer appears to be multifactorial and includes both environmental and genetic factors. Approximately 75% of colorectal cancers are sporadic, whereas 15% to 20% develop in those with either a positive family history or a personal history of colorectal cancer or polyps.2 The remaining cases occur in people with genetic predispositions, such as hereditary nonpolyposis colorectal cancer (HNPCC) (4% to 7%) or familial adenomatous polyposis (FAP) (1%), or in people with inflammatory bowel disease, particularly chronic ulcerative colitis (1%).
The fundamental role of environmental factors is supported by observations in migrant populations. Generally, migrants from low-incidence regions in Africa and Asia who relocate to high-incidence regions of North America or Australia assume the incidence of the host country within one generation.3 Specifically, a high-fat, low-fiber diet is associated with the development of colorectal cancer, although it is unclear if it is causative. Conversely, the ingestion of a high-fiber diet is associated with protection against colorectal cancer. Fiber causes the formation of a soft, bulky stool that dilutes out carcinogens; it also decreases colonic transit time, allowing less time for carcinogenic substances to contact the mucosa. The more sedentary lifestyle in Western countries, cigarette smoking, and alcohol consumption also appear to be linked with the risk of colorectal neoplasia.
Most colorectal cancers arise from benign adenomatous polyps lining the wall of the bowel. Those that grow to a large size (>2 cm) and have a villous appearance or contain dysplastic cells are most likely to progress to cancer. This progression from adenoma to carcinoma is associated with an accumulation of genetic alterations, including activation of oncogenes and inactivation of tumor suppressor genes.4 One of the early steps in this process is the interruption of the APC/?β-catenin/TCF-4 pathway, allowing unchecked cellular replication at the crypt surface.5 This can occur in the germline of FAP patients, with the second allele being inactivated somatically, or in sporadic cancers, in which both alleles are somatically inactivated.
There are likely three pathways that lead to colorectal cancer: chromosomal instability (CIN), microsatellite instability (MSI), and CpG island methylator phenotype (CIMP).6 CIN is the genetic reason for tumor formation in 50% to 70% of colorectal cancers and the mechanism operative in FAP. It is typically coupled with mutations in the KRAS, APC, and TP53 genes, ultimately leading to loss of heterozygosity of TP53 and malignant transformation. MSI is found in more than 90% of HNPCCs that carry a germline inactivation in DNA mismatch repair genes, but also in 15% of sporadic cancers, in which epigenetic hypermethylation silences gene transcription of hMLH1. With MSI, multiple frameshift mutations at microsatellite sequences occur, including those in exon coding sequences of the transforming growth factor-beta receptor II, the proapoptotic BAX gene, and the DNA mismatch repair genes (hMSH3 and hMSH6 genes). The third type, CIMP, is a relatively heterogeneous subgroup and occurs in approximately 10% to 30% of patients, is predominantly associated with KRAS gene mutations but sometimes with BRAF gene mutations, usually lacks chromosomal instability, and has the poorest prognosis of the three types and perhaps a poorer response to chemotherapy. Of the numerous molecular markers examined to date, MSI, 18q, thymidylate synthase, and TP53 overexpression are among those which appear to have the most prognostic significance in colon cancer.7 Although the markers are not currently incorporated into the staging system, they should be noted.
Colorectal cancer is the fourth commonest form of cancer worldwide, with an estimated 800,000 new cases diagnosed each year, accounting for roughly 10% of all cancers.8 Globally, the colorectal cancer incidence per 100,000 persons in 1990 was 19.4 for men and 15.3 for women. High incidence rates are found in North America, Western Europe, and Australia (40 to 45 cases per 100,000 population) and intermediate rates are found in Eastern Europe (26 cases per 100,000 population), with the lowest rates found in Africa (3 to 8 cases per 100,000 population). Approximately two-thirds of cases occur in the colon and one-third in the rectum. In the United States, 39,760 new cases of rectal cancer were estimated to occur in 2011 (22,620 in men, 17,050 in women),1 there is little difference in incidence among whites, African Americans, and Asian Americans.
The occurrence of sporadic colorectal cancer increases continuously above the age of 45 to 50 years for both genders and peaks in the seventh decade. Subgroups of patients, including those with inherited syndromes such as familial adenomatous polyposis (FAP), hereditary nonpolyposis colorectal cancer (HNPCC), or hamartomatous polyposis conditions (e.g., Peutz-Jeghers syndrome), can experience colorectal cancer at a much earlier age.9
Prevention and Early Detection
Primary Prevention
Primary prevention involves the identification and elimination of factors that cause or promote colorectal cancer or interfere with the adenoma-to-carcinoma cascade. Dietary and lifestyle approaches employ higher-fiber, lower-fat components and increased physical activity to inhibit the carcinogenic process. Other dietary components, such as selenium, carotenoids, and vitamins A, C, and E, may also have protective effects by scavenging free oxygen radicals. Folic acid, a component of fresh fruits and green vegetables, supplies methyl groups necessary for nucleotide synthesis and gene regulation. Prospective studies generally support an inverse association between folate intake and colorectal cancer risk.10
Chemopreventive strategies are based on population-based studies that strongly support an inverse relationship between the use of nonsteroidal anti-inflammatory drugs, such as aspirin, sulindac, or the new selective COX-2 inhibitors, and the risk of colorectal adenomas or carcinomas.11 COX-2 is overexpressed in more than 50% of adenomas and 80% to 85% of adenocarcinomas. Trials are currently under way that focus on FAP patients, those with resection of early-stage colorectal carcinomas, and those with a history of adenomatous polyps.
Screening for Early Detection
The process of malignant transformation from adenoma to carcinoma takes several years. The goal of screening is to prevent rectal cancer deaths through the detection and treatment of benign or premalignant lesions and curable-stage cancers.12,13 For the average-risk population, screening should begin at age 50 years and should follow one of the following testing options: fecal occult blood testing every year, flexible sigmoidoscopy every 5 years, yearly fecal blood testing and flexible sigmoidoscopy every 5 years, colonoscopy (preferably) every 10 years, or double-contrast barium enema studies every 5 years. If polyps are found, however, colonoscopy should be performed every year until the patient is polyp free.
Two promising but investigational approaches to screening include virtual colonoscopy and molecular stool testing.7,14 Virtual colonoscopy employs virtual reality technology from cross-sectional CT or MRI scans. Molecular stool testing is based on the molecular detection of neoplasm-specific DNA from exfoliated cancer cells.
Biologic Characteristics and Molecular Biology
The most important prognostic factor for overall survival is the pathologic extent of disease as determined by the degree of bowel wall penetration by the tumor, and the presence or absence of lymph node metastases or distant metastases (TNM stage).15 Tumor differentiation is also prognostically important because poorly differentiated adenocarcinomas are associated with lymph node metastases in more than 50% of cases and also correlate with the likelihood of lymphatic and venous invasion.16 An elevated carcinoembryonic antigen (CEA) level at the time of presentation has an adverse impact on survival times independent of tumor stage.17 If the level is higher than 100 ng/mL, the patient has distant metastasis (most likely, to the liver or lung) until proven otherwise. Detection of occult metastases in lymph nodes, blood, or bone marrow by molecular techniques may allow further refinement in pathologic staging. Molecular strategies added to the more traditional histopathologic information may help in the future to identify patients at a lower stage whose tumors are likely to behave like higher-stage lesions, and vice versa. Several biologic markers, including allelic loss of 18q, alteration in KRAS, MSI, thymidylate synthase, thymidine phosphorylase, vascular endothelial growth factor (VEGF), epidermal growth factor receptor (EGFR), P21, P27, BCL2, BAX, and TP53, among others, are now being prospectively evaluated in clinical trials to determine their prognostic utility.2 At the present time, however, the TNM staging system is the most reliable.
Pathology and Pathways of Spread
Histopathology
The majority (>90%) of colorectal cancers are adenocarcinomas. Some adenocarcinomas have mucin, which can be extracellular (colloid) or intracellular (signet-ring cell). Colloid cancer, which occurs in 15% to 20% of adenocarcinomas, is not an independent prognostic factor, whereas signet-ring cell carcinoma, which occurs in 1% to 2% of adenocarcinomas, is an independently poor prognostic factor for survival.18,19 Other histologic types are rare and include carcinoid tumors,20 leiomyosarcomas,21,22 lymphomas,23 and squamous cell cancers.24 The grading system used for adenocarcinomas refers to the degree of differentiation. Some institutions use a three-grade system (well, moderate, poor), and others use a four-grade system. Despite substantial interobserver and intraobserver variability in tumor grading, poorly differentiated tumors have consistently been found to be associated with a worse prognosis in multivariate analysis.
Anatomy and Pathways of Spread
The anterior peritoneal reflexion represents the point at which the rectum exits the peritoneal cavity and becomes a retroperitoneal structure (approximately 12 to 15 cm from the anal verge). Below this level, there is a mesorectal, or circumferential, resection margin all around the rectum. The circumferential resection margin (CRM) is related more to the type of surgical procedure than to an anatomic landmark, however. While distal intramural spread usually extends no more than millimeters beyond the grossly recognizable margin of the tumor, microscopic tumor nodules (satellites) are found in the mesorectum, predominantly in a radial direction but also in a distal one, some centimeters from the lower tumor margin.25 A layer of visceral fascia encloses both the rectum and mesorectum and thus forms a separate compartment within the pelvis. With total mesorectal excision (TME), the entire specimen is removed by sharp dissection along the mesorectal plane. Patients entered into postoperative adjuvant rectal trials in the United States were required to have tumors with the inferior aspect at or below the peritoneal reflection. For entry into preoperative trials, most use tumors with a distance of less than 12 cm from the anal verge for eligibility. The German trial allowed tumors at a distance of as much as 16 cm, however.26
Clinical Manifestations, Patient Evaluation, and Staging
Patient Evaluation
The standard diagnostic algorithm for rectal cancer is seen in Table 49-1. The pretreatment evaluation of a patient with rectal cancer should include a careful history and physical examination. By digital rectal examination (the average finger can reach approximately 7 to 8 cm), tumors can be assessed for size, ulceration, and fixation to surrounding structures. This examination also permits evaluation of sphincter function, which is critical when determining whether a patient is a candidate for a sphincter-sparing procedure. Rigid proctosigmoidoscopy allows direct visualization of the lesion and provides an estimation of the size of the lesion and degree of obstruction. This procedure is used to obtain biopsies and gives an accurate measurement of the distance of the lesion from the anal verge. A complete evaluation of the large bowel, preferably by colonoscopy, should be done to rule out synchronous neoplasms.
TABLE 49-1 Diagnostic Algorithm for Rectal Cancer
| History | Including family history of colorectal cancer or polyps |
| Physical examination | Including assessment of size, minimum diameter of lumen, mobility, distance from anal verge, and cursory evaluation of sphincter function |
| Proctoscopy | Including assessment of mobility, minimum diameter of lumen, and distance from anal verge. Allows biopsy of the primary tumor. |
| Colonoscopy or barium enema | To detect possible synchronous neoplasm |
| Endorectal ultrasound | To assess extent of primary tumor, if considering local excision or preoperative therapy |
| Pelvic CT or MRI scanning | To assess extent of primary tumor and lymph node involvement (for accuracy of transrectal ultrasound, CT; MRI for T and N category) (see Table 49-2) |
| Chest radiograph and abdominal ultrasound | To detect possible metastatic disease |
| Abdominal CT/MRI scanning Lung CT scanning | To further investigate suspicious findings of chest radiographs and abdominal ultrasound |
| PET/CT scanning | To rule out metastatic blood-borne or nodal disease |
| CEA levels | To obtain baseline CEA level (a prognostic factor and important for follow-up) |
| Complete blood count | To check for anemia secondary to bleeding |
CEA, carcinoembryonic antigen; CT, computed tomography; MRI, magnetic resonance imaging; PET, positron emission tomography.
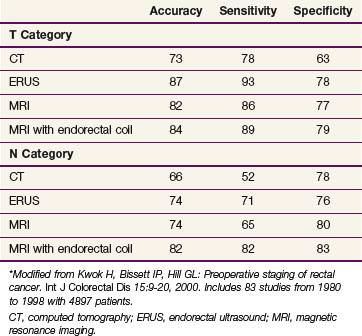
The primary imaging modalities for assessing the extent of the primary tumor are endorectal ultrasound (ERUS), CT, positron emission tomography (PET), and MRI. ERUS and high-resolution pelvic MRI are the most accurate tools in predicting the T stage of rectal cancers (Fig. 49-1 and Table 49-2). With the shift to preoperative therapy, clinical staging to accurately identify both T stage and N stage is critical. Imaging techniques to assess the extent of the primary tumor include CT, MRI, PET with 18F-fluorodeoxyglucose (FDG-PET), and transrectal ultrasound. In the United States, ultrasound plus CT or MRI is commonly used, whereas in many European countries, high-resolution pelvic MRI is preferred. High-resolution MRI also allows for identification of patients likely to have close or positive radial margins if they undergo initial surgery and therefore they are selected to receive preoperative therapy.27 For example, the Mercury trial, based in the United Kingdom, uses MRI to select for the intensity of preoperative therapy.28 In a retrospective analysis of 504 patients reported by Bail and colleagues,29 even following preoperative chemoradiation, those with positive radial margins still had a higher local recurrence rate (35% vs. 11%) and a lower 5-year survival rate (27% vs. 73%) compared with those with negative radial margins.
The overall accuracy of imaging studies in predicting disease extent varies by imaging modality and disease category (T vs. N vs. M). The accuracy for T category is approximately 50% to 90% with transrectal ultrasound30 or high-resolution MRI31 and 50% to 70% with CT or conventional MRI scanning.32 For identification of metastatic disease (M stage), FDG-PET/CT may be more accurate than CT alone.33 The use of PET/CT to restage patients following preoperative chemoradiation remains controversial.34–36
The identification of positive lymph nodes is more difficult. The overall accuracy in detecting positive pelvic lymph nodes with the above techniques is approximately 50% to 75%. The accuracy of MRI is similar to that of CT, but it is improved with the use of external and/or endorectal coils. Both CT and MRI can identify lymph nodes measuring 1 cm or more, although enlarged lymph nodes are not pathognomonic of tumor involvement. The accuracy of MRI is similar to that of CT and may be further enhanced with the use of superparamagnetic iron oxide particles.37 Likewise, the accuracy of ultrasound for the detection of involved perirectal lymph nodes may be augmented if ultrasound is combined with fine-needle aspiration.38 Despite these advances, the ability to accurately predict the pathologic stage following preoperative chemoradiation with MRI,39,40 ultrasound,41,42 FDG-PET,34 or physical examination43 remains suboptimal. The tumor regression grade44,45 may help predict lymph node positivity; patients would have already received preoperative chemoradiation, however.
Screening for distant metastatic disease is commonly performed with CT and/or MRI. The major advantage of a PET/CT scan is to differentiate between recurrent tumor and scar tissue by measuring tissue metabolism of an injected glucose-based substance.46,47 Scar tissue is inactive, whereas tumor tissue is generally hypermetabolic. At the present time, PET/CT is considered investigational for a routine preoperative metastatic workup in a patient who presents with primary disease,33 but its use should be considered strongly for patients with presumed locoregional relapse who are being considered for aggressive treatment approaches with curative intent.33
Imaging after Chemoradiation
Although ERUS, CT, and MRI can be used to assess downstaging of the tumor after neoadjuvant treatment, none is accurate in distinguishing among ypT0, ypT1, ypT2, or ypT3 tumors. Overstaging is common, especially when there is a fibrotic thickening of the rectal wall. A reasonably high level of accuracy has been observed by phased-array MRI for differentiating ypT0 to T2 versus ypT3 disease.48 Both diffusion-weighted MRI and FDG-PET/CT have been used to monitor therapy response and to predict the outcome following preoperative therapy. Of the two, FDG-PET/CT has a larger role. Many studies have reported a significant decrease in standardized uptake values (SUVs) on postirradiation FDG-PET/CT scans in responders when compared with nonresponders, but the clinical value of this information remains to be determined.49
Staging
The first practical staging system was the Dukes’ classification.50 This system classified colorectal tumors from A to C, with stage A indicating penetration into but not through the bowel wall, stage B indicating penetration through the bowel wall, and stage C indicating involvement of lymph nodes, regardless of the extent of bowel wall penetration. The system has since been modified by many authors, including Dukes, to reflect finer levels of penetration and nodal metastases and has been extended to include the colon as well as the rectum.
The Astler-Coller staging system allowed separation of wall penetration and nodal status. The Gunderson-Sosin modification of the Astler-Coller staging system subdivided T3 tumors into those with microscopic (B2m or C2m) or gross (B2m+g or C2m+g) penetration of tumor through the bowel wall.51 It also defined tumors adherent to or invading an adjacent organ or structure as B3 if the nodes were negative and C3 if the nodes were positive. Several studies have analyzed both local failure and survival using the modified Astler-Coller staging system,52 with most confirming the predictive capability of this system.
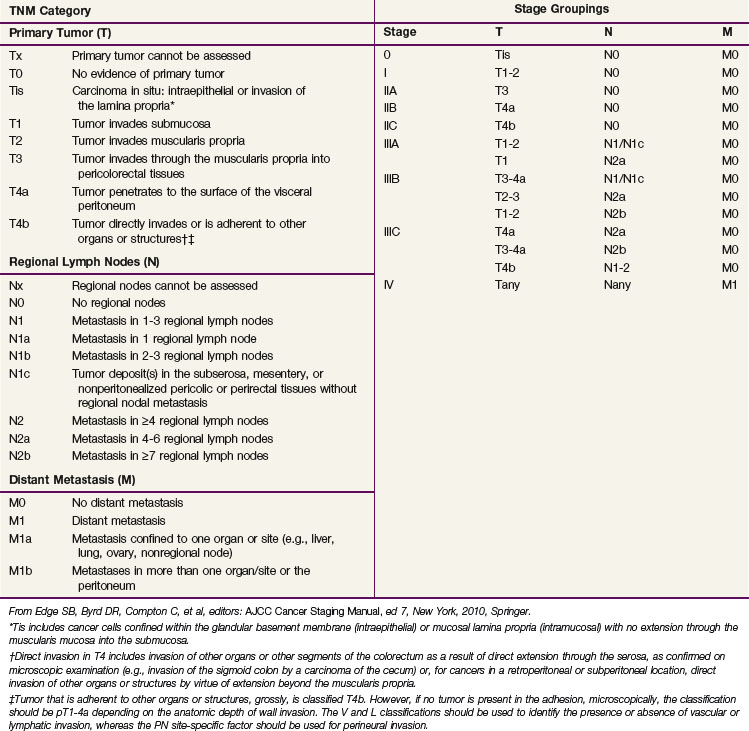
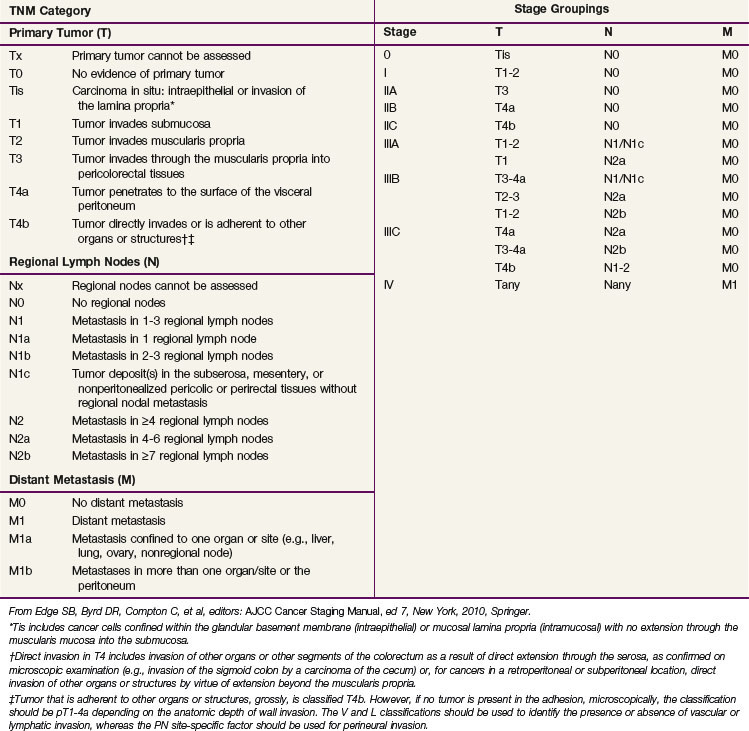
In the sixth edition of the AJCC staging manual, stage II colorectal cancer was subdivided into IIA (T3N0) and IIB (T4N0) and stage III was subdivided into IIIA (T1-2N1M0), IIIB (T3-4N1M0), and IIIC (any TN2M0), based on improved outcomes for patients with IIA versus IIB disease and IIIA versus IIIB disease.53 The prognostic validity of this change was supported by a subsequent pooled analysis of the U.S. GI Intergroup and National Surgical Adjuvant Breast and Bowel Project (NSABP) postoperative trials54 and the retrospective analysis of the American College of Surgeons National Cancer Database (NCDB).55 The placement of all TN2 patients into stage IIIC, however, was not based on in-depth outcomes analyses, because the impact of depth of bowel wall invasion (T category) in N2 patients had not been evaluated in detail.
Before making substantive changes in the AJCC seventh edition staging manual for colon and rectal cancer (Table 49-3), the AJCC Hindgut Task Force sought population-based validation that depth of invasion and nodal status interact to affect survival rates. Surveillance, Epidemiology, and End Results (SEER) survival data were obtained for patients with invasive colon and rectal cancer and evaluable TN category of disease (35,829 rectal and 109,953 colon cancer patients).56 T4N0 cancers were stratified by “tumors that perforate visceral peritoneum” (T4a) versus “tumors that invade or are adherent to adjacent organs or structures” (T4b). N1 and N2 were stratified by number of involved nodes (N+): N1a/N1b (1 vs. 2 or 3 nodes), and N2a/N2b (4 to 6 vs. ≥7 nodes). Rates of 5-year observed and relative survival were obtained for each TN category. The analyses indicated the following information: survival rates are better for T1-2N0 cancers than T3N0 cancers, better for T3N0 cancers than T4N0 cancers, better for T1-2N2 cancers than T3-4N2 cancers, and similar for T4bN1 and T4N2 cancers. In addition, patients with T4a lesions have better survival rates than those with T4b lesions by N category, and the number of positive lymph nodes affects survival for each T category. The SEER population-based colon and rectal cancer analyses supported subdividing T4 (T4a/T4b), N1 (N1a/N1b), and N2 (N2a/N2b) and supported revised substaging of stages II and III (shift of T1-2N2 lesions from IIIC to IIIA/IIIB and T4bN1 lesions from IIIB to IIIC.56,57
There are additional descriptors that do not affect the stage grouping but do indicate cases needing separate analysis. The AJCC TNM staging system should be used routinely for staging and treatment purposes. Although CEA has prognostic importance, it was not added to the staging system.15
The role of the pathologist is critical to proper staging. Following surgery alone, at least 12 pelvic nodes must be examined to obtain an accurate pN stage. Tumors treated with preoperative chemoradiation are downstaged, however, and it is commonly not possible to evaluate 12 lymph nodes for this purpose.58,59
Primary and Adjuvant Therapy for Resectable Disease
Adjuvant Irradiation without Chemotherapy
Postoperative Irradiation
Until 1990, most patients in the United States underwent surgery and, if needed, received postoperative external beam radiation therapy (EBRT). The primary advantage with this approach was pathologic staging and avoiding overtreatment with preoperative therapy. As confirmed by the German CAO/ARO/AIO 94 phase III trial that randomized preoperative versus postoperative chemoradiation, the disadvantage of postoperative therapy is significantly higher rates of local recurrence and acute and chronic toxicity, as well as a significantly lower chance of sphincter preservation.26 Lastly, if the patient has undergone an APR, the radiation field must be extended to include the perineal scar.
Historical nonrandomized data from the Massachusetts General Hospital60 and M.D. Anderson Cancer Center61 reveal crude local failure rates of 4% to 31% in patients with stage pT3-4N0M0 disease and 8% to 53% in patients with stage pT3-4N1-2M0 disease who received 45 to 55 Gy without chemotherapy.
There are five randomized trials examining the use of adjuvant postoperative irradiation without chemotherapy in stage pT3 and/or N1-2 rectal cancer.62,63,64,65,66 None have shown an improvement in overall survival (OS). Two reveal a decrease in local failure rates; NSABP trial R-01 (16% vs. 25%; p = .06) and the Medical Research Council (MRC) trial (21% vs. 34%; p = .001).65
Preoperative Irradiation
Dose escalation has not shown a clear benefit. In the Lyon R96-02 trial, 88 patients with cT2 to T3 rectal cancer received 39 Gy in 13 fractions to the pelvis and were randomized to observation or a boost with contact irradiation to a total dose of 85 Gy.67 A total of 23 patients were selected to receive postoperative chemotherapy. Patients who received the boost had a decrease in the local failure rate (2% vs. 7%) but there was no difference in 2-year disease-free survival (DFS) (92% vs. 88%).
A unique clinical situation in which preoperative radiation therapy alone is recommended is when a patient has a distal uT2N0 tumor and refuses an APR. Although APR is the standard therapy, an alternative treatment is preoperative irradiation followed by low anterior resection (LAR) and, if the pelvic nodes are positive, postoperative chemotherapy. In a series of 27 patients with cT2N0 distal rectal cancer who refused APR and received preoperative EBRT, 78%underwent a sphincter-sparing operation.68 The incidence of 5-year actuarial local recurrence in those undergoing sphincter preservation was 13%; the colostomy-free survival rate, 100%; and the OS, 85%. Overall, 77% of those who underwent a sphincter-sparing procedure had good to excellent bowel function at 24 to 36 months after surgery.
Short-Course Preoperative Irradiation
There are 12 modern randomized trials of preoperative radiation therapy (without chemotherapy).69 All use low to moderate doses of radiation. Most of the trials showed a decrease in local recurrence rates, and in five of the trials, this difference reached statistical significance. Although in some trials a subset analysis revealed a significant improvement in survival rates, the Swedish Rectal Cancer Trial is the only one that reported a survival advantage for the total treatment group. Two meta-analyses report conflicting results. Although both revealed a decrease in local recurrence rates, the analysis by Camma and associates70 reported a survival advantage, whereas the analysis by the Colorectal Cancer Collaborative Group71 did not.
In the Swedish Rectal Cancer Trial, patients with cT1-3 rectal cancer were randomized to receive 25 Gy in 1 week followed by surgery 1 week later versus surgery alone.72 Those who received preoperative irradiation had a significant decrease in local recurrence rates (12% vs. 27%; p <.001) and a correspondingly significant improvement in 5-year OS (58% vs. 48%; p = .004). After 13 years, the OS is still significantly improved (38% vs. 30%; p = .008).73 Of interest, the local recurrence rate in node-positive patients who underwent surgery alone was 46%, illustrating the inferior results of surgery before the adoption of TME.
The Dutch CKVO 95-04 trial randomized 1805 patients with cT1 to T3 disease to TME or intensive short-course preoperative radiation therapy followed by TME.74 Irradiation significantly decreased the local recurrence rate (8% vs. 2%; p < .0001), but there was no difference in the 2-year survival rate (82%). With longer follow-up, the 5-year local failure rate was higher with TME (11%) but was still significantly decreased (to 6%) with preoperative irradiation.75 The acute toxicity rates in the Dutch CKVO 95-04 trial included a 10% rate of neurotoxicity, a 29% rate of perineal wound complications, and a 12% rate of postoperative leaks.76 Of the patients who developed postoperative leaks, 80% required surgery, resulting in death in 11%.
The presence of a positive circumferential margin is an important negative prognostic sign. In the Dutch CKVO trial, 17% had positive circumferential margins. Although they received 50 Gy postoperatively, this did not compensate for positive margins.77 Few centers perform the necessary pathologic examination to detect positive circumferential margins.29,78 MRI can help identify patients who will have positive margins with surgery alone as well as select those who may benefit from preoperative therapy.79–81
Preoperative plus Postoperative Irradiation
This approach, also known as the sandwich technique, includes a short preoperative course of radiation (5 to 15 Gy) followed by surgery, and in patients with pT3-4N1-2 disease, an additional 40 to 45 Gy postoperatively. The Radiation Therapy Oncology Group (RTOG) trial 81-15 randomized 350 patients (87% with rectal cancer) to preoperative irradiation with 5 Gy versus surgery alone.82 Patients with stage pT3 and/or N1-2 disease received a minimum dose of 45 Gy postoperatively. No chemotherapy was delivered. There were no differences in rates of local failure, distant failure, or OS between the arms. A retrospective analysis of 155 patients treated at the Institut Gustave Roussy also revealed no advantage of the sandwich technique compared with preoperative irradiation.83 This approach is no longer used.
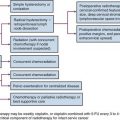
Adjuvant Combined-Modality Therapy
There are two conventional treatment approaches for clinically resectable rectal cancers. For patients with cT1-2N0 disease, the initial treatment is surgery, and if the tumor is pT3N0 or TanyN1-2, this is followed by postoperative chemoradiation.84 For patients with cT3-4N0 or TanyN+ lesions, preoperative chemoradiation is given, followed by surgery and postoperative adjuvant chemotherapy.
Postoperative Chemoradiation
The National Cancer Institute (NCI) Consensus Conference concluded in 1990 that chemoradiation was the standard postoperative adjuvant treatment for patients with pT3 and/or N1-2 disease.84 This recommendation was based on phase III trials that compared postoperative chemoradiation arms with control arms of either surgery alone or surgery plus postoperative irradiation (Mayo/NCCTG 79-47-51) and demonstrated improvements in both DFS and OS.85 The standard design in U.S. trials was to deliver six cycles of bolus 5-fluorouracil (5-FU)–based chemotherapy; concurrent irradiation was also given during cycles 3 and 4.
The U.S. GI Intergroup 86-47-51 trial did not demonstrate an incremental benefit to semustine when it was added to postoperative irradiation plus concurrent and maintenance 5-FU.86 However, a 2 × 2 component of the study demonstrated a positive benefit for giving protracted venous infusion (PVI) 5-FU rather than interrupted bolus 5-FU concurrently with pelvic irradiation. Patients randomized to receive concurrent PVI 5-FU (225 mg/m2/day, 7 days/week or until intolerance) had improvements in rates of disease control, DFS (at 4 years, 63% vs. 53%; p = .01), and OS (at 4 years, 70% vs. 60%; p = .005).
The successor INT 0114 four-arm trial randomized patients with pT3-4N0 and/or TanyN+ rectal cancer to postoperative irradiation and bolus 5-FU with or without leucovorin, levamisole, or leucovorin plus levamisole (INT 86-47-51 results were not available before INT0114 study design and completion). There was no significant difference in local control or survival rates among the four arms.87 With longer follow-up, the study also revealed that local control and survival results continued to deteriorate after 5 years. At 7 years, the local failure rate was 17% and the survival rate was 56%, compared with 14% and 64%, respectively, at 5 years. Patients with high-risk (pT3N+ or T4) disease had a lower survival rate compared with lower-risk (pT1-2N+ or T3N0) disease (45% vs. 70%). Further analysis of the INT 0114 trial has revealed that body mass is related to outcome and treatment-related toxicity,88 and both surgeons and hospitals with higher volumes of rectal cancer surgery have improved outcomes compared with those with lower volumes.89
The subsequent INT 0144 postoperative adjuvant rectal trial was designed to follow up on the positive results achieved with concurrent PVI 5-FU during irradiation in trial 86-47-51.90 Patients were randomized to three arms: arm 1, bolus 5-FU/PVI 5-FU + RT/bolus 5-FU (control arm from 86-47-51); arm 2, PVI 5-FU/PVI 5-FU + RT/PVI 5-FU; arm 3, bolus 5-FU–leucovorin(LV)–levamisole/bolus 5-FU–LV-levamisole + RT/bolus 5-FU–LV-levamisole. The concurrent PVI 5-FU arms did not confirm a survival benefit relative to the bolus 5FU/LV/levamisole arm, but arm 2 did report a lower incidence of grade 3+ hematologic toxicity. Based on these results, when 5-FU is used with either preoperative or postoperative chemoradiation, PVI has been the preferable standard.
Do Patients with Pathologic Node-Negative Rectal Cancer Require Pelvic Irradiation?
The 1990 NCI Consensus Conference recommendation for postoperative chemoradiation was published nearly 20 years ago and was based on trials where neither a TME nor an examination of 12 nodes or more was required. Retrospective data suggest that there may be a subset of patients with pT3N0 disease who may not require adjuvant therapy. Nissan and associates91 reported results of 100 patients with uT2-3N0 disease who underwent TME alone and had 12 nodes or more examined.
The sixth edition of the AJCC staging manual subdivided stage III into IIIA (T1-2N1), IIIB (T3-4N1), and IIIC (TanyN2). The prognostic validity of this change was supported by both the rectal pooled analysis of the U.S. GI Intergroup and NSABP postoperative trials54 and the retrospective analysis of the American College of Surgeons National Cancer Database.55 The 5-year survival rates by stages IIIA, B, and C in the pooled analysis were 81%, 57%, and 49% and in the NCDB database were 55%, 35%, and 25%, respectively. These data provided further evidence that patients who undergo TME, have at least 12 nodes examined, and have stage pT3N0 disease may not need the radiation component of chemoradiation, dependent on the adequacy of radial and distal margins of resection. The approximately 3% to 4% benefit in local control with irradiation may not be worth the risks, especially in women of reproductive age. However, patients with pT3N0 tumors with adverse pathologic features, or who undergo resection without TME, or who have fewer than 12 nodes examined should still receive postoperative chemoradiation.
Although the number of nodes is defined in the AJCC staging system, the location of pelvic nodes is not. Leibold and associates59 treated 121 patients with preoperative chemoradiation and found that the incidence of metastatic disease was higher in those patients with positive nodes in the proximal pelvis compared with positive nodes anywhere in the pelvis (46% vs. 32%). Of note, the proximal nodes are above the superior border of the typical radiation field (L5/S1) because they are located along the apical and mid portion of the inferior mesenteric artery.
Preoperative Chemoradiation
Based on the German CAO/ARO/AIO 94 trial, preoperative chemoradiation is standard treatment for patients with cT3-4N0 or TanyN+ disease.26 The disadvantage of preoperative therapy is the possible overtreatment of patients with either early-stage disease (pT1-2N0) or undetected metastatic disease. In the German trial that used CT and transrectal ultrasound, 18% of patients were overstaged. A number of questions and issues exist with regard to patient selection for preoperative chemoradiation and optimization of treatment that will be addressed in the following subsections.
The Need for Chemotherapy with Preoperative Irradiation
Almost every randomized trial for the past two decades has confirmed a 10% to 15% survival benefit of a total of 6 months of adjuvant 5-FU-based chemotherapy for patients with lymph node-positive colon or rectal cancer. Both retrospective92 and randomized trials,93,94 however, question whether chemotherapy improves the results of preoperative irradiation in patients with cT3-4 rectal cancer.
The European Organization for Research and Treatment of Cancer (EORTC) trial 22921 was a four-arm randomized trial of 1011 patients who received preoperative irradiation of 45 Gy with or without a concurrent bolus of 5-FU/leucovorin followed by surgery with or without four cycles of postoperative 5-FU/leucovorin.93 Only 37% had a TME. The EORTC trial revealed a significant decrease in the local failure rate in those patients who receive chemoradiation compared with irradiation (8% to 10% vs. 17%; p <.001) but no difference in the 5-year OS (65%). However, only 43% received 95% or more of the planned postoperative chemotherapy, which may explain the negative results. Furthermore, a subset analysis of the EORTC trial revealed that patients who responded to preoperative chemoradiation had a survival benefit from postoperative chemotherapy.95
A trial by the Fédération Francophone de la Cancérologie Digestive (FFCD 9203) was a two-arm trial of 742 patients randomized to preoperative irradiation of 45 Gy with or without bolus 5-FU/leucovorin.94 All patients were scheduled to receive postoperative chemotherapy, and 73% received such. The FFCD trial reported a similar decrease in local failure rates (8% vs. 17%; p <.05) and a corresponding increase in pathologic complete response (pCR) (11% vs. 4%; p <.05) with preoperative chemoradiation vs. irradiation alone, but no survival benefit (68% vs. 67%).
Because most patients did not receive adequate doses of postoperative chemotherapy in the EORTC trial and the FFCD trial only tested the impact of concurrent chemotherapy with preoperative irradiation, preoperative chemoradiation followed by surgery and 4 months of postoperative adjuvant chemotherapy remains the standard practice in North America. However, there remains considerable controversy in some European countries regarding its use. A recent consensus conference failed to reach a definitive recommendation regarding its use.96
Potential Overtreatment with Preoperative Therapy
In the German CAO/ARO/AIO 94 rectal trial, 18% of patients clinically staged as cT3N0 preoperatively and who underwent initial surgery without preoperative therapy had pT1-2N0 disease.26 Therefore, those patients would have been overtreated if they had received preoperative therapy. Although not ideal, preoperative therapy is still preferred to performing surgery first because even after preoperative chemoradiation (which downstages tumors), Guillem and coauthors97 reported that 22% will have ypN+ disease at the time of surgery. In patients who undergo surgery alone, this number is as high as 40%.98 These patients will then require postoperative chemoradiation, which, compared with preoperative chemoradiation, has inferior rates of local control, higher rates of acute and chronic toxicity, and, if a low anastomosis is performed, inferior functional results.
In the report by Guillem and coauthors,97 the incidence of positive nodes was not dependent on the distance from the anal verge. Of the 103 patients with tumors that were 0 to 5 cm from the anal verge, 23% were ypN+, whereas of the 85 patients with tumors that were 6 to 12 cm from the anal verge, the incidence was 20%. These data suggest that in tumors up to 12 cm from the anal verge, the risk of positive nodes (and likely local recurrence) is similar.
Positive Radial (Circumferential) Margins
Although the distal margin is predictive of both local recurrence and the feasibility of a sphincter-preserving operation, the radial (circumferential) margin also has a substantial impact on the local recurrence rate.99 An analysis of more than 17,500 pathologic specimens by Nagtegaal and associates99 reported inferior survival rates in patients with positive CRMs after neoadjuvant treatment compared with immediate surgery (hazard ratio [HR], 6.3; 95% CI, 3.7 to 16.7 vs. HR, 2; 95% CI, 1.4 to 2.9, respectively).
In the Dutch CKVO trial, 17% of patients had positive circumferential margins. In a subset analysis by Nagtegaal and colleagues,100 patients with positive radial margins who underwent TME alone had a local recurrence rate of 17% after an LAR and 30% after an APR.
Unfortunately, few centers perform the necessary pathologic examination to detect positive circumferential margins.78 High-resolution MRI can help identify patients who will have positive margins.79–81 In a retrospective analysis reported by Bail and colleagues,29 despite receiving preoperative chemoradiation, 504 patients with positive radial margins had a higher local recurrence rate (35% vs. 11%) and a lower 5-year OS (27% vs. 73%) compared with those with negative radial margins.
As reported with preoperative therapy, postoperative treatment has limited ability to control positive radial margins. In the MRC CR-07 trial, patients with positive radial margins who received postoperative chemoradiation had an 11% local recurrence rate.101 Likewise, in a subset analysis of the Dutch CKVO trial, 50 Gy postoperatively did not compensate for positive margins.77
Distance from the Anal Verge
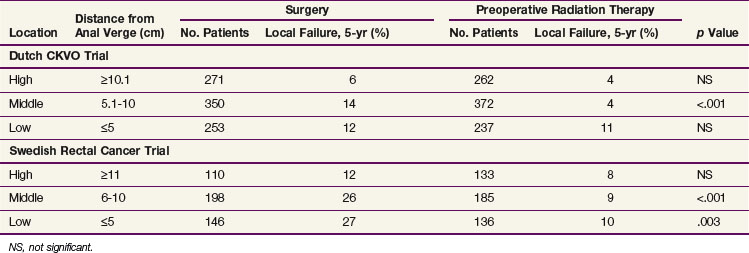
There are no prospective randomized data examining the impact of the distance from the anal verge on local recurrence. The available data are subset analyses from randomized trials that were not stratified by distance. Of the three trials, two used short-course preoperative irradiation and included patients with cT1-2N0 disease (Dutch CKVO75 and the Swedish Rectal Cancer Trial),73 whereas the German trial used chemoradiation and was limited to patients with cT3N+ disease.26,102 The MRC-C07 trial made a similar subset analysis, and the distance from the anal verge was determined by rigid sigmoidoscopy. There were additional variables that could have contributed to the differences in local failure rates. For example, TME (and its associated impact on radial margins) was used in the Dutch CKCO and German trials and not in the Swedish trial. All three trials included patients with tumors more than 12 cm from the anal verge in the “upper or high” category. Since the peritoneal reflection varies from 12 to 16 cm, some patients with tumors above the peritoneal reflection (colon cancer) were included in the three trials. Most investigators now limit preoperative treatment to tumors less than 12 cm from the anal verge.97 Lastly, distance measurements using a flexible proctoscope are less accurate than straight proctoscope measurements. Flexible scopes were used in the Dutch CKVO trial. The German trial used a straight scope. In the Swedish trial, proctoscopic information was not mentioned. However, eligibility was limited to tumors “below the promontory as identified by barium enema.” The Polish trial is not discussed, because all tumors were palpable by digital examination.103
As seen in Table 49-4, by univariate analysis, “high” tumors in both the Dutch CKVO and Swedish trials (defined as ≥10.1 cm and ≥11 cm, respectively) had a lower incidence of local recurrence compared with mid and lower tumors. Short-course irradiation did not significantly decrease local recurrence rates. By multivariate analysis, tumor location was an independent prognostic variable in the Dutch trial. It is interesting to note that irradiation did significantly decrease local recurrence rates for mid tumors in both trials, whereas for lower tumors it was helpful only in the Swedish trial.
In contrast, there was no significant difference between mid and upper tumors in the German trial.104 However, data were not provided. In a recent subset analysis, patients with tumors above 6 cm had a lower local recurrence rate (Rödel, personal communication).
In summary, given the conflicting data combined with the report from Guillem and associates97 confirming that the incidence of positive nodes (ypN0 disease following preoperative chemoradiation) is the same from 0 to 12 cm from the anal verge, treatment decisions based on the current definitions of low versus mid versus high should not be used.
Sphincter Preservation with Preoperative Chemoradiation
An analysis of 1316 patients who received intensive short-course preoperative irradiation revealed that downstaging was most pronounced when the interval between the completion of irradiation and surgery was at least 10 days.105 In the Dutch CKVO 95-04 trial, where the interval was 1 week, there was no downstaging.106
When the goal of preoperative therapy is sphincter preservation, conventional irradiation doses and techniques are recommended. These include multiple-field techniques to a total dose of 45 to 50.4 Gy at 1.8 Gy per fraction. Surgery should be performed 4 to 8 weeks following the completion of irradiation. Unlike the intensive short course of irradiation regimen, this conventional design allows for two important events to occur. First is the recovery from the acute side effects of irradiation, and second is adequate time for tumor downstaging. Data from the Lyon R90-01 trial of preoperative irradiation suggest that an interval of longer than 2 weeks following the completion of irradiation increases the chance of downstaging.107 Most series recommend a 4- to 8-week interval.108–110 Whether increasing the interval between the end of intensive short-course irradiation and surgery to more than 4 weeks will increase downstaging is not known. This question is being addressed in the ongoing Stockholm III trial.
Clinical Experience with Sphincter Preservation
A valid concern of surgeons is that to perform sphincter preservation in those patients who would otherwise require an APR, the distal resection margin may be suboptimal (<1 cm). Can preoperative therapy compensate for this? Retrospective data from the Memorial Sloan-Kettering Cancer Center reveal that with preoperative chemoradiation, the 3-year local control rates were similar regardless of the margins being more than 2 cm, less than 2 cm, more than 1 cm, or less than 1 cm, providing they were negative.78,111 Similar data have been reported from other investigators.112
Sphincter preservation without good function is of questionable benefit. In a series of 73 patients who underwent surgery, Grumann and associates113 reported that the 23 patients who underwent an APR had a more favorable quality of life compared with the 50 who underwent an LAR. Krouse and colleagues114 reported that both men and women with ostomies had significantly worse social well-being compared with those without ostomies, however.
Although preoperative chemoradiation may adversely affect sphincter function,115 the impact is most likely less than postoperative chemoradiation.116 Most phase II trials that examine functional outcome report good to excellent results. Functional results continue to improve up to 1 year after surgery. Functional data from the German trial are pending.
Is Surgery Needed after Preoperative Chemoradiation?
In one series, the value of radical surgery in patients who had a biopsy-proven complete response was questioned.117 The trial included patients with cT1-3 disease, however, and has not been reproduced by other investigators. In series limited to patients with cT3 disease who received preoperative chemoradiation, radical surgery is still necessary to fully evaluate whether a pathologic response has been achieved. Neither post-treatment ultrasound41,42 nor physical examination (which is only 25% accurate)118 is sufficient. The use of PET scanning119,120,34 and diffusion MRI121 as noninvasive measures of response is being investigated, and reported results have been mixed. Although Kalff and associates35 reported that postchemoradiation FDG-PET identification of residual viable tumor in 63 patients had a high positive predictive value (0.94; 95% CI, 85% to 99%), other groups have reported opposite results.
Glynne-Jones and colleagues122 reviewed 218 phase II and 28 phase III trials of preoperative irradiation or chemoradiation and confirmed that a clinical and/or radiologic response does not sufficiently correlate with the pathologic response; they do not recommend a “wait and see” approach to surgery following preoperative therapy.
Randomized Trials of Preoperative Versus Postoperative Chemoradiation
Two randomized trials of preoperative versus postoperative chemoradiation for clinically resectable rectal cancer have been performed, NSABP R0-3123 and the German CAO/ARO/AIO 94 trial.26
The German trial completed the planned accrual of over 800 patients and randomized patients with uT3-4 and/or LN+ rectal cancers less than 16 cm from the anal verge to preoperative chemoradiation (with CI 5-FU during weeks 1 and 5) versus postoperative chemoradiation.26 Patients were stratified by surgeon. Compared with postoperative chemoradiation, patients who received preoperative therapy had a significant decrease in rates of local failure (6% vs. 13%; p = .006), acute toxicity (27% vs. 40%; p = .001), and chronic toxicity (14% vs. 24%; p = .012), and in the 194 patients judged by the surgeon before treatment to require an APR, there was a significant increase in rates of sphincter preservation (39% vs. 20%; p = .004). With a median follow-up of 40 months, there was no difference in 5-year OS (74% vs. 76%). A subsequent analysis revealed that the treatment center, schedule, and gender were independent prognostic factors for local control.124
The NSABP R-03 study accrued only 267 of a planned 900 patients with cT3-4 rectal cancers.123 Patients received induction chemotherapy followed by conventional chemoradiation and were randomized to receive it either preoperatively or postoperatively. TME was not required, and some patients underwent local excision. Patients who received preoperative versus postoperative therapy had a significant improvement in 5-year DFS (65% vs. 53%; p = .011) and a borderline significant improvement in 5-year OS (75% vs. 66%; p = .065). There was no difference in 5-year local recurrence rates (11%). There was a correspondingly higher incidence of grade 4+ toxicity, almost all related to early diarrhea (33% vs. 23%), but the incidence of grade 3+ toxicity was lower (41% vs. 50%). Lastly, based on a prospective office assessment by the operating surgeon, there was no improvement in rates of sphincter preservation (48% vs. 39%). The results do not parallel the German trial, likely because of the fact that only 267 of the 900 planned patients were accrued, thereby limiting the statistical power to detect differences.
Given the improved local control rates, acute and long-term toxicity profiles, and sphincter preservation rates reported in the German trial, patients with cT3-4 rectal cancer who require chemoradiation should receive it preoperatively. In the German trial, 18% of patients who were clinically staged as cT3N0 preoperatively and underwent surgery without preoperative therapy had pT1-2N0 disease. Therefore, those patients would have been overtreated if they had received preoperative therapy. Although not ideal, this is preferred to performing surgery first because 20% to 40% will have LN+ disease at the time of surgery and require postoperative chemoradiation, which has inferior rates of local control, higher rates of acute and chronic toxicity, and, if a low anastomosis is performed, inferior functional results.97
Clearly, the development of more accurate methods to identify LN+ disease, including imaging techniques and/or molecular markers, is essential because more patients are being treated with preoperative chemoradiation.44,125–128
The UK Medical Research Council trial (MRC C07) randomized 1350 patients with clinical stage I to III rectal cancer to preoperative irradiation of 5 Gy in five fractions or selective postoperative chemoradiation (45 Gy with concurrent 5-FU), which was delivered only to patients with a histologic CRM of less than 1 mm (12% of all patients with immediate surgery).130 With a median follow-up of 4 years, patients who received preoperative compared with selective postoperative treatment had significantly lower 3-year local recurrence rates (4.4% vs. 10.6%; p <.0001) and higher 3-year DFS (77.5% vs. 71.5%; p = .013).
Short-Course Preoperative Irradiation Versus Standard-Course Preoperative Chemoradiation
Bujko and colleagues103,129 performed a randomized trial of two preoperative approaches. A total of 316 patients with cT3 rectal cancer were randomized to 5 Gy in five fractions followed by surgery (median, 8 days) versus conventional preoperative chemoradiation (50.4 Gy plus bolus 5-FU/leucovorin daily for 5 days, during weeks 1 and 5) followed by surgery (median, 78 days). All tumors were above the anorectal ring; TME was performed for distal tumors; and there was no irradiation quality control review. The incidence of CRM positivity was lower following chemoradiation compared with irradiation alone (4% vs. 13%; p = .017).
Standard and Novel Combined-Modality Therapy Regimens and Issues
The NCCTG 85-47-51 postoperative adjuvant rectal trial revealed a 10% survival benefit for patients who received concurrent PVI versus bolus 5-FU.86 Therefore, when 5-FU is combined with irradiation, either preoperatively or postoperatively, it should be delivered as a continuous infusion (CI). Although a survival benefit with CI 5-FU was not confirmed in the Intergroup 0144 trial, the CI 5-FU arm was associated with a lower incidence of hematologic toxicity.90,131 Although it is just now being studied in rectal cancer, the combination of CI 5-FU and oxaliplatin (FOLFOX) has replaced CI 5-FU as a standard postoperative chemotherapy treatment based on the efficacy demonstrated in stage III colon cancer patients.132
As an alternative, based on the X-ACT trial, which reported equivalence with the Mayo Clinic regimen in patients with stage II and III colon cancer, it is reasonable to substitute capecitabine for 5-FU.133 However, capecitabine has not been directly compared with CI 5-FU, and this is one of the end points of the NSAPB R-04 rectal trial.
The Cancer and Leukemia Group B (CALGB) 89803 trial illustrated that the survival benefit of irinotecan in patients with metastatic disease does not necessarily translate into the adjuvant setting.134 In contrast, based on the MOSAIC trial, which revealed a survival benefit with FOLFOX for node-positive colon cancer, oxaliplatin-based chemoradiation programs have been investigated. Many phase I and II trials have shown higher pCR rates compared with 5-FU-based chemoradiation regimens.
However, two phase III trials have reported significantly higher acute toxicity rates with no benefit in the pCR rate with the addition of oxaliplatin to CI 5-FU-based chemoradiation regimens in patients with cT3-4N+ rectal cancer (see Table 49-5). The STAR-01 trial randomized 747 patients to preoperative chemoradiation with 50.4 Gy plus CI 5-FU with or without oxaliplatin (60 mg/m2 weekly).135 There was a significant increase in grade 3+ toxicity with oxaliplatin (24% vs. 8%; p <.001) with no improvement in the pCR rate (15% vs. 16%). The ACCORD trial randomized 598 patients to preoperative chemoradiation with 50 Gy plus CAPOX versus 45 Gy plus capecitabine.136 There was a similar significant increase in grade 3+ toxicity with oxaliplatin (25% vs. 11%; p <.001) with no improvement in the pCR rate (19% vs. 14%). Although local control and survival outcomes are pending, these early results underscore the importance of phase III data.
Most preoperative chemoradiation regimens have been developed somewhat empirically without clear criteria for timing of the irradiation. For example, in a retrospective analysis, Yu and colleagues137 reported a significantly improved pCR rate when capecitabine was delivered 1 hour before irradiation compared with other intervals (24% vs. 10%; p = .01). Most phase I to II chemoradiation trials do not control for this variable.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree