10 Radiologic Techniques: Virtual Colonoscopy
Principles and Supporting Literature
Virtual colonoscopy is a method by which colon polyps can be detected using multidetector computed tomography (MDCT) scanners combined with specialized three-dimensional (3D) software. It requires bowel cleansing, colon insufflation, and careful review of the data. The method was first described in 1995, but although the concept was valid, early results were limited because of slow scanner speed, relatively thick collimation (3- to 5-mm slices), and lack of reliable high-speed 3D software.1 Over the years, these limitations are no longer an obstacle. New MDCT scanners allow submillimeter slices, extremely fast scanning speeds, and now fast real-time software designed specifically for this application.
Most of the early published data from the 1990s and early 2000s involved only high-risk patients and patients with polyposis syndromes, but these studies did show encouraging results. However, virtual colonoscopy did not get widespread attention until the publication of the first large screening trial by Perry Pickhardt2 in 2003. In this trial, 1233 asymptomatic adults underwent virtual colonoscopy and conventional colonoscopy in the same day. Virtual colonoscopy demonstrated a patient sensitivity of 94% and a specificity of 96%,2 as seen in Table 10-1. In addition, the sensitivity of detecting polyps larger than 1 cm was 94% for the virtual colonoscopy and only 88% for the optical colonoscopy.2 Although this difference was not statistically significant, this manuscript attracted a lot of attention from both the medical community and the lay community. This was the first large screening study to demonstrate high sensitivity and specificity for clinically significant polyps.
Table 10-1 Performance Characteristics of Virtual Colonoscopy and Optical Colonoscopy for the Detection of Adenomas *
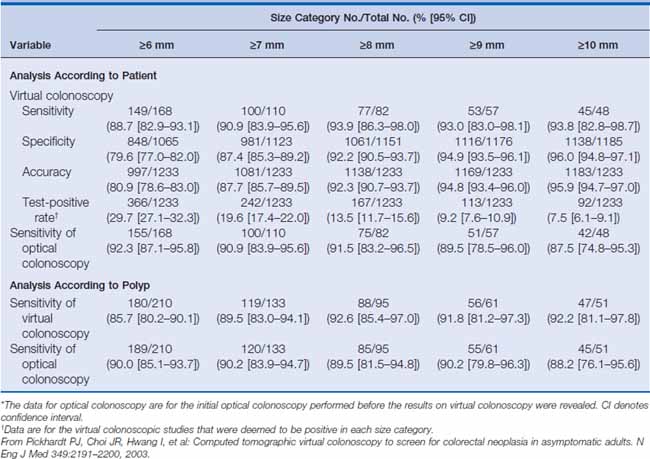
Two smaller studies of screening virtual colonoscopy were published in 2004 with less impressive results. The first was published by Cotton and colleagues,3 and the second was published by Rockey and colleagues.4 Both studies showed a significantly lower sensitivity and specificity for polyps, even in the centimeter range. These two studies had some limitations, especially involving training of the participating radiologists.3,4 The Pickhardt study, however, showed that at least in that trial it was possible to get high sensitivity and specificity for colon polyps with high-quality data and experienced radiologists.2 To confirm his results, the ACRIN National CT Colonography Trial was established. The trial enrolled over 2600 patients and was a multi-institutional trial involving 15 centers. Patients in this trial also underwent virtual colonoscopy and conventional colonoscopy on the same day. The results of this trial were published in September 2008.5 In this study of asymptomatic adults, the CT colonography identified 90% of subjects with adenomas or cancers 10 mm or more in diameter.
Technique
Bowel Cleansing
The bowel preparation begins the day before the examinations and consists of several steps. In addition to a clear liquid diet the day before the CT, the patient drinks 4 liters of polyethylene glycol mixture as directed. Two bisacodyl tablets are also given to the patient to clear some of the residual fluid remaining in the colon. In most patients, this preparation is adequate.
Stool Tagging
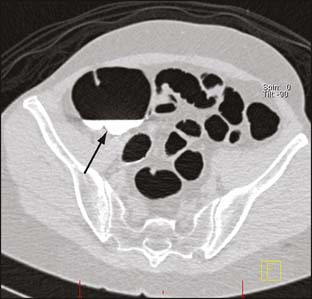
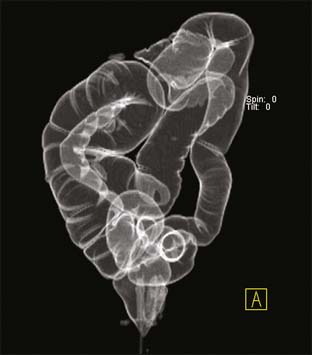
In addition to the bowel-cleansing agents, it is necessary to include stool-tagging agents in an attempt to “mark” any residual stool or fluid. Solid stool tagging is accomplished when the patient drinks a small quantity of barium during the bowel cleansing. This dilute barium mixes with residual solid stool, allowing quick identification on the CT (Fig. 10-1). A small quantity of iodinated oral contrast is also given to the patient just before bedtime (i.e., the night before the CT scan). This mixes with residual fluid increasing its density. Therefore, residual fluid also appears white (Fig. 10-2).
Colonic Insufflation
To identify polyps in the colon, the colon must be adequately distended with air (Fig. 10-3). If the colon is collapsed, polyps and masses may be overlooked. Colonic insufflation can be accomplished with either room air or carbon dioxide. If room air is used, a small tube is inserted into the rectum and the colon is distended by manually pumping in room air, similar to the procedure used during a barium enema. However, many investigators and radiologists prefer to use an electronic insufflator pump and carbon dioxide. Carbon dioxide is absorbed by the body and exhaled by the patient. Therefore within minutes after the study the patient feels fine. The pump also maintains a steady colonic pressure during the study, automatically adding more gas when needed (Tables 10-2 and 10-3).
Table 10-2 Clinical Adequacy of Distention for Individual Colon Segments According to Insufflation Method
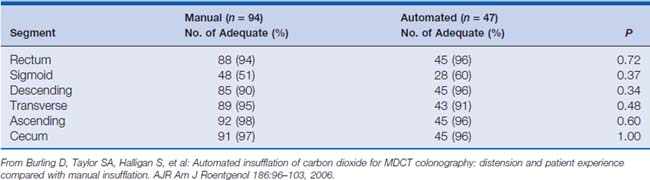
Table 10-3 Effect of Increasing Total Volume of Carbon Dioxide Administered on Distention Score According to Patient Position
| Position and Segment | Odds Ratio* (95% CI) | P† |
|---|---|---|
| Supine | ||
| Rectum | 0.69 (0.40–1.18) | .17 |
| Sigmoid | 0.65 (0.36–1.14) | .13 |
| Descending | 0.78 (0.44–1.34) | .37 |
| Transverse | 0.61 (0.27–1.34) | .22 |
| Ascending | 0.78 (0.45–1.75) | .55 |
| Cecum | 0.72 (0.36–1.46) | .37 |
| Prone | ||
| Rectum | 0.56 (0.27–1.15) | .11 |
| Sigmoid | 0.47 (0.27–0.92) | .03 |
| Descending | 0.46 (0.21–0.98) | .04 |
| Transverse | 0.66 (0.37–1.17) | .16 |
| Ascending | 0.78 (0.22–2.70) | .52 |
| Cecum | 0.51 (0.28–0.92) | .03 |
| Supine and prone combined | ||
| Rectum | 0.64 (0.41–1.02) | .06 |
| Sigmoid | 0.57 (0.34–0.94) | .03 |
| Descending | 0.66 (0.36–1.23) | .19 |
| Transverse | 0.64 (0.34–1.22) | .18 |
| Ascending | 0.78 (0.22–2.70) | .70 |
| Cecum | 0.59 (0.36–0.95) | .03 |
CI, confidence interval.
* Odds ratio is odds of being in next highest distention category for a 1-L increase in carbon dioxide volume.
† Values in boldface are statistically significant.
From Burling D, Taylor SA, Halligan S, et al: Automated insufflation of carbon dioxide for MDCT colonography: distension and patient experience compared with manual insufflation. AJR Am J Roentgenol 186:96–103, 2006.
There is controversy in the literature as to the usefulness of administering glucagon before the CT colonography exam, we have found it to be helpful.6,7 Glucagon relaxes the colon, thereby potentially allowing greater distention and reducing spasm and patient discomfort. However, it is expensive and has some risks. Therefore, we do not routinely use glucagon.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree