Principles of Orthopaedic Pharmacology
Carol D. Morris
Numerous orthopaedic conditions are amenable to pharmacologic intervention. This chapter will summarize the basic science principles behind the most commonly used drugs in orthopaedic practice.
Antibacterials
Detailed knowledge of the most likely organism(s) causing a specific infection matched with the spectrum of the antibacterial is essential to maximize the therapeutic effect while minimizing resistance. Therefore, in general, antibac-terials are most effective when they are directed against a single pathogen for a short period of time and potentially harmful when directed against multiple pathogens for a long period of time.
Classification by Mechanism of Drug Action
Inhibition of cell wall synthesis: penicillins, cephalospo-rins, imipenem, vancomycin
Penicillins (amoxicillin, piperacillin) are inactivated by β-lactamase and are thus ineffective against Staphylococcus aureus.
Semisynthetic penicillins (nafcillin, oxacillin, dicloxacillin) are active against β-lactamase—producing S. aureus.
Cephalosporins: cephalothin, cephalexin, cefazolin, cephamandole, ceftriaxone
Semisynthetic penicillins and cephalosporins are more effective than vancomycin against infections caused by methicillin-sensitive strains of S. aureus.
Inhibition of protein synthesis: doxycycline, azithromycin, erythromycin, clindamycin, gentamicin
Clindamycin is active against anaerobes and most gram-positive cocci except enterococci, but it selects for Clostridium difficile.
Aminoglycosides are used against gram-negative bacilli; they are associated with renal and auditory toxicity.
Interference with DNA metabolism: quinolones, metro-nidazole
Quinolones are primarily active against gram-negative bacteria.
Metronidazole is effective against all anaerobes and many parasites by exploiting their inability to metabolize oxygen free radicals.
Antimetabolites: trimethoprim, sulfonamides
Mimic essential nutrients to block replication
Combination of trimethoprim and the sulfonamide sulfamethoxazole blocks folic acid synthesis with a wide spectrum of activity.
Clinical Applications
Surgical prophylaxis
In general, antibacterial prophylaxis is indicated in
procedures with a high inherent infection rate or when the prevalence of infection is low but such an infection would have catastrophic results.
For most elective orthopaedic procedures, the potentially offending pathogens are actually relatively limited: S. aureus, Staphylococcus epidermidis, aerobic streptococci, and anaerobes.
For maximum benefit, the antimicrobial should be administered within 1 hour preceding the incision.
Open fractures
Antimicrobials should be given as soon as possible.
Risk of infection in open fractures depends on the severity of soft tissue injury.
S. aureus and gram-negative bacilli are the most common pathogens causing infections after open fractures.
Certain environmental exposures require specific coverage:
Farm-related exposures: penicillin for Clostridium perfringens
Soil: clindamycin or metronidazole for anaerobic microorganisms
Fresh water: third-generation cephalosporin or quinolone for Pseudomonas species
Osteomyelitis
β-lactam agents, aminoglycosides, and doxycycline are able to achieve serum-level concentrations in acutely infected bone.
Clindamycin is able to treat organisms such as S. aureus that have the ability to evade antimicrobials following macrophage ingestion.
Anticoagulants
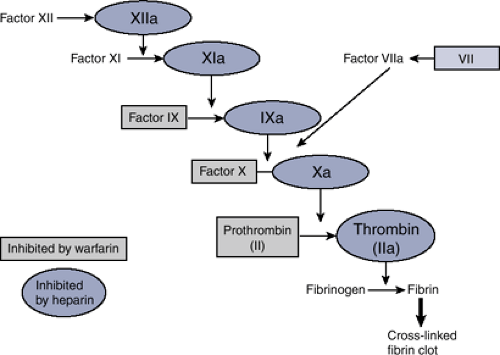
Approximately 2 million deep venous thromboses (DVT) are diagnosed each year in the United States; of these, 200,000 to 600,000 (10% to 30%) propagate to pulmonary emboli (PE). Many pharmacologic agents used for DVT prophylaxis and treatment intervene at steps along the clotting cascade with the goal of preventing fibrin formation, the end product of the cascade (Fig. 18-1).
Aspirin
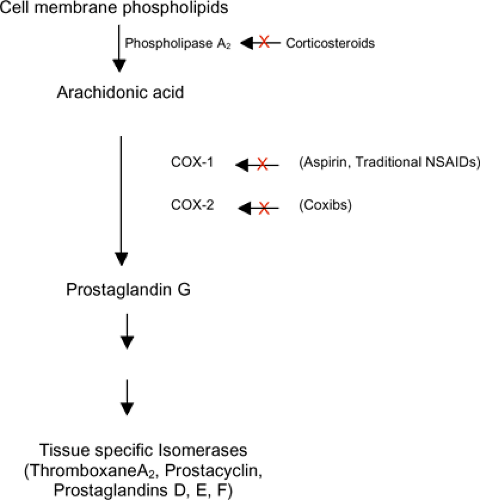
Irreversibly binds cyclooxygenase (COX-1 and COX-2), thereby blocking arachidonic acid from forming prostaglandins (Fig. 18-2)
In platelets, aspirin suppresses thromboxane A2 production; thromboxane A2 triggers platelet aggregation via phospholipase C.
Clinically, aspirin has little if any role in prophylaxis of venous thromboembolism.
Warfarin
Warfarin is a vitamin K antagonist of vitamin K oxidoreductase (VKOR), the enzyme responsible for the activation of vitamin K.
Coagulation factors II, VII, IX, and X require vitamin K for activation.
In the absence of active vitamin K, inactive clotting factors accumulate, leading ultimately to decreased fibrin formation.
The anticoagulant effect is measured by the prothrombin time (PT) and the international normalized ratio (INR) target of 2 to 3.
Heparin
Heparin binds antithrombin (AT), exposing AT’s active site and increasing the affinity of AT for active clotting factors.
Clinically, heparin has unpredictable pharmacokinetics.
Heparin-induced thrombocytopenia (HIT) is a condition in which patients become thrombocytopenic and prothrombotic simultaneously.
Fixed low-dose subcutaneous heparin (i.e., 5,000 U) has limited efficacy for venous thromboembolism.
Effects of heparin can be reversed with intravenous protamine.
Low-molecular-weight heparins (LMWHs)
Exert effect by the same mechanism that heparin does
Pharmacokinetic profile is very predictable and therefore monitoring is largely unnecessary except in renal insufficiency and weight extremes.
Appears to be as efficacious as warfarin in orthopaedic patients
Dalteparin, enoxaparin, tinzaparin, and nadroparin are approved by the U.S. Food and Drug Administration (FDA).
No antidote exists, but protamine can neutralize up to 60% of effect.
Factor Xa inhibitor (Fondaparinux)
Chemically unrelated to heparin and LMWH, but has similar mechanism
No known antidote
Anti-Inflammatory Agents
Most musculoskeletal conditions are characterized by some inflammatory component. Pharmacological agents to manage the symptoms of inflammatory conditions are the most frequently prescribed medicines in the United States.
Nonsteroidal Anti-inflammatory Drugs (NSAIDs; Table 18-1)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree