Principles of Chemotherapy
Carl E. Freter
SINGLE AGENTS
The term “chemotherapy” was coined by Paul Ehrlich in the early 20th century in a search for compounds to act as “magic bullets” in the treatment of bacterial infections. Compounds believed to be useful in the treatment of cancer are described in ancient pharmacopeia. An interesting example is provided by arsenical compounds described in traditional Chinese medicine; arsenicals were subsequently a component of “Fowler solution” advocated in 1856 for the treatment of chronic myelogenous leukemia (CML), and also shown to have activity in Hodgkin lymphoma. Renewed interest in these compounds occurred in 1996 with the description by Chinese investigators of major activity of arsenic trioxide in acute promyelocytic leukemia (APL),1 and its subsequent investigation in other malignancies.2
Alkylating agents, the first class of “modern” cancer chemotherapy drugs, were born of the observation that “mustard gas” developed as a military antipersonnel weapon in World War II caused lymphoid and bone marrow suppression. Dramatic responses of advanced lymphomas to nitrogen mustard treatment, and the development of antifolates by Sidney Farber in childhood leukemia, both in the mid-1940s, ushered in the era of “modern” chemotherapy.3
Chemotherapeutic agents were first used individually, with the hope that all malignant cells would be sensitive and thus eliminated. The recognition that bone marrow toxicity was dose-limiting resulted in the design of therapeutic regimens around the kinetics of bone marrow recovery. Although this approach led to responses, and occasionally complete remission, progression of disease remained inevitable in the vast majority of malignancies. It was not long before the failures of this approach were realized, which motivated the development of combination therapy.
Single agents continue, however, to have an important place in treatment, and cure may be possible with single agent treatment in a few selected malignancies. The early exciting experience with methotrexate in choriocarcinoma,4 and cyclophosphamide in Burkitt5 lymphoma demonstrated the curative potential of a single-agent therapy in these diseases. Hairy cell leukemia can be “cured” (or at least a lengthy remission produced) with α interferon, or one of the purine analogues such as 2-CDA, or Pentostatin.6 Another important application of single agents is the sequential use of drugs with differing mechanisms of action and patterns of resistance. In the setting of metastatic breast cancer, the sequential use of a taxane (paclitaxel or docetaxel), capecitabine, vinorelbine, gemcitabine, pemetrexed, and other drugs can achieve disease control, often over long periods with acceptable toxicity and quality of life.7 Because palliation becomes the goal when cure is not possible, solid tumors will often be treated with single agents when initial therapy fails. Single agent hormonal therapy for metastatic breast or prostate cancer often produces excellent responses and disease control, sometimes for prolonged periods.
COMBINATION CHEMOTHERAPY
Cancer Cell Growth Kinetics and Drug Resistance
The principles of combination chemotherapy have been developed empirically but have also been strongly guided by the study of cancer cell growth kinetics and mechanisms of cancer cell resistance to chemotherapy. From a different perspective, the study of cancer cell growth kinetics and mechanisms of chemotherapy resistance have been powerful tools for understanding how chemotherapy fails. In the 1960s, Skipper and colleagues8 used experimental murine leukemia models to define the concept of logarithmic cancer cell growth and the complementary concept that a given dose of chemotherapy would produce a given log cell kill independent of the total number of cells in the tumor. In reality, cancer cell growth is not purely logarithmic, particularly for solid tumors.9,10,11 Instead, it is a complex function of heterogeneous growth kinetics, cell death, and genetic instability leading to mutations potentially affecting drug resistance, production of paracrine or autocrine growth factors, and the capacity for invasion and metastases. To more accurately model the known growth characteristics of solid tumors, the Gompertzian model of tumor growth following a sinusoidal curve was developed in which the doubling time increases steadily as the tumor grows larger; that is, the tumor grows progressively more slowly. The Norton-Simon model12,13 (see Chapter 2) based upon Gompertzian growth predicts that the log kill will be greater for very small cancers than for very large cancers. In this model cell kill is dependent on the size of the tumor, and therefore its position on the Gompertzian growth curve; a larger tumor with a smaller growth fraction will have a smaller fractional cell kill for a given dose of chemotherapy. The Norton-Simon model favors, particularly for smaller tumors, multiple sequential single agents at high doses and a “crossover intensification” concept, that is, alternating regimens over more than one cycle to achieve better response of small tumors.
The Goldie-Coldman model,14 (see Chapter 3) based on Luria and Delbruck’s studies of mutation rates of resistance
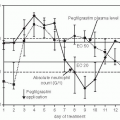
in bacteria to bacteriophage killing15 mathematically models genetic resistance of cancer cells to chemotherapy drugs. A fundamental concept of this model is that chemotherapy resistance mutations occur in cell populations of 103 to 106 cancer cells, substantially lower than the limit of clinical detection, which is about 109 cells or 1-cm3 mass. The probability of a tumor having resistant cells is based on both the tumor mass and the mutation rate of the cells in the tumor. The Goldie-Coldman hypothesis predicts that to most effectively overcome spontaneous drug resistance multiple active agents should be given over the shortest time as early in the growth of the cancer as possible. It also predicts that multiple agents given simultaneously will be superior to sequential single agents at higher doses. These principles have also given rise to the related concepts of dose intensity and dose density. The concept of dose intensity refers to the total dose of an agent administered during a fixed time and was formalized in calculations applied to various chemotherapy regimens by Hryniuk et al.16,17 Increases in dose intensity have often involved increasing doses in fixed regimens in the same time, sometimes with growth factor support. The concept of dose density involves increasing the dose per unit time (in mg/m2/week), and generally involves shortening the dosing interval to achieve this.
in bacteria to bacteriophage killing15 mathematically models genetic resistance of cancer cells to chemotherapy drugs. A fundamental concept of this model is that chemotherapy resistance mutations occur in cell populations of 103 to 106 cancer cells, substantially lower than the limit of clinical detection, which is about 109 cells or 1-cm3 mass. The probability of a tumor having resistant cells is based on both the tumor mass and the mutation rate of the cells in the tumor. The Goldie-Coldman hypothesis predicts that to most effectively overcome spontaneous drug resistance multiple active agents should be given over the shortest time as early in the growth of the cancer as possible. It also predicts that multiple agents given simultaneously will be superior to sequential single agents at higher doses. These principles have also given rise to the related concepts of dose intensity and dose density. The concept of dose intensity refers to the total dose of an agent administered during a fixed time and was formalized in calculations applied to various chemotherapy regimens by Hryniuk et al.16,17 Increases in dose intensity have often involved increasing doses in fixed regimens in the same time, sometimes with growth factor support. The concept of dose density involves increasing the dose per unit time (in mg/m2/week), and generally involves shortening the dosing interval to achieve this.
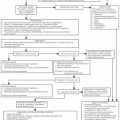
Combination chemotherapy has developed both empirically and rationally using the principles of cancer cell growth kinetics and drug resistance into a set of guiding principles governing the development of effective combination chemotherapy regimens.18,19 These principles of combination chemotherapy are listed in Table 4.1.
(1) All drugs must be active as single agents. (2) Drugs should be chosen for nonoverlapping toxicity. This allows for spreading toxicity over multiple organ systems allowing adequate recovery for cyclic chemotherapy and avoiding critical toxicity to any single organ. (3) Drugs should be chosen for different or synergistic mechanisms of action. This enables attacking cancer cells simultaneously at multiple different target molecules or biochemical pathways. It also helps in overcoming drug resistance at any single target or pathway. (4) Drugs should have different mechanisms or patterns of resistance. Drug resistance occurs through different mechanisms both spontaneously and through the selection pressure of exposure of cancer cells to different drugs or classes of drugs. Using drugs with different mechanisms of resistance enables cancer cells developing resistance to one drug to be attacked by other drugs to which resistance has not yet developed. (5) Drugs should be given in optimum dose and schedule in a cyclic fashion to optimize dose intensity/dose density. This allows maximum cell kill with a given drug dose and avoids both “kinetic” chemotherapy failure and drug resistance. (6) Drug doses should be individually titrated in individual patients to end-organ toxicity (bone marrow, GI tract, skin, nervous system, etc.) This now nearly universal feature of chemotherapy regimens provides for adequate recovery from toxicity to allow cyclic chemotherapy to proceed at maximum tolerated doses on the planned chemotherapy schedule.
Table 4-1 Principles for Combination Chemotherapy Regimens | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
The MOPP regimen for Hodgkin lymphoma20 is the prototypic combination chemotherapy regimen employing these principles, and it changed a uniformly fatal disease treatable with single agents into a cancer with a stable shoulder on the survival curve consistent with cure.20 Application of these chemotherapeutic principles has led to the development of combination chemotherapy regimens for an expanding list of cancers potentially curable with chemotherapy alone as shown in Table 4-2.
Alternating Non-cross-Resistant, Dose Intense, and Dose Dense Combination Chemotherapy
Hodgkin lymphoma has the advantage of having several active chemotherapy regimens containing different drugs (MOPP and ABVD) and has afforded opportunities to test the predictions of the Goldie-Coldman and Norton-Simon hypotheses. The Goldie-Coldman hypothesis predicts that alternating MOPP and ABVD (alternating non-cross-resistant therapy) would result in exposure of cancer cells to more effective agents per unit time and be superior to either regimen alone. A randomized trial of MOPP versus ABVD versus alternating MOPP/ABVD indeed demonstrated both improved complete remission and survival in favor of the alternating regimen.21 Similarly, a hybrid MOPP/ABV regimen was shown to be superior to
MOPP followed by ABVD.22 A caveat to these results, however, is decreased doses of MOPP drugs delivered in large trials.
MOPP followed by ABVD.22 A caveat to these results, however, is decreased doses of MOPP drugs delivered in large trials.
Table 4-2 Cancers Potentially Curable with Chemotherapy Alone | ||||||||
|---|---|---|---|---|---|---|---|---|
|
These concepts have also been evaluated in breast cancer. A regimen using alternating cycles of CMFVP and VATH in comparison with Cyclophosphamide Doxorubicin Floorouracic (CAF) or Vinblastine Doxorubicin Thiotepa Halotestin (VATH) alone, demonstrated no superiority of the alternating regimen.23 Alternating versus sequential adjuvant therapy has been examined in breast cancer using doxorubicin and CMF, comparing four cycles of doxorubicin followed by eight cycles of CMF versus two cycles of CMF alternating with one cycle of doxorubicin, with the same total dose of drugs in both arms. Disease-free and overall survival were superior in the sequential arm,24 more consistent with the Norton-Simon model. The concept of dose dense therapy was supported in a Cancer and Leukemia Group B trial of adjuvant therapy in node-positive breast cancer. Patients were randomized to receive AC followed by paclitaxel, each for four cycles or sequential single agent A, C, and paclitaxel for four cycles. Patients were also randomized to receive therapy on 3-week intervals or 2-week intervals with Granulocyte Colony Stimulating Factor (GCSF) support. The 2 week (dose-dense) schedule was associated with improved disease-free and overall survival, with no difference between the concurrent or sequential schedules.25 Studies of alternating regimens in small cell lung cancer have likewise demonstrated some survival benefit in extensive and limited stage disease.26,27,28 Taken together, these results indicate that the Goldie-Coldman and Norton-Simon hypotheses have provided a framework for hypothesis-driven clinical investigation, which has in many cases led to improved therapy. The challenges remain of improving treatment results, decreasing short-and long-term toxicities (second malignancies and organ damage), and overcoming drug resistance and kinetic treatment failure.
An emerging area of cancer biology that represents a potentially new mechanism of chemotherapy failure is the recognition of cancer-specific stem cells that may have different growth kinetics, biologic properties, and drug sensitivity than their progeny. Strategies for eradication of these cancer stem cells may be a key to curative therapy in a variety of now incurable malignancies.29,30,31,32
ROUTES OF ADMINISTRATION
Intravenous, Oral
Most chemotherapeutic agents are available only in an intravenous preparation, requiring venous access. Venous access, whether temporary during chemotherapy administration or by surgically implanted intravascular devices, must be chosen carefully with respect to the anticipated duration, complexity, types of drugs (vesicants or nonvesicants), and anticipated need of fluid replacement, blood products, and antibiotics. Patient preference and quality of life issues also play a role. Venous access devices are a major source of morbidity and (rarely) mortality in cancer patients owing primarily to infectious and thrombotic complications, as well as extravasation of chemotherapeutic agents.33,34 Patient education, meticulous attention to aseptic technique, and frequent examination for signs of infection or thrombosis are essential to the care of patients with these devices. Thrombosis prophylaxis with Coumadin, heparins, or other agents is an increasingly common standard of care for surgically implanted externalized or internal devices (see Chapter 27).35
A number of agents are available in oral form, making intravenous access unnecessary. Besides their standard use in various chemotherapy regimens, oral agents, because of their simplicity and convenience, have an important role in palliative therapy, where quality of life issues are paramount.36 The use of oral agents may be limited in patients with functional or anatomical barriers to their ingestion and absorption.
Appendix 1 indicates which agents can be given orally.
Intraperitoneal Therapy
Direct intraperitoneal instillation of chemotherapy drugs offers a 2- to 5-fold, and higher, depending on the drug, concentration advantage over systemic intravenous administration. This exposes tumor cells to both higher peak drug concentrations and area under the concentration-time curve drug levels.37 Intraperitoneal therapy is usually accomplished through a surgically implanted intraperitoneal catheter, which may be either exteriorized or subcutaneous. Nuclear medicine scans are sometimes used to demonstrate a freely communicating peritoneal space free of walled-off adhesions, which is a requirement for optimal therapy. Intraperitoneal therapy is ideally suited to the treatment of small-volume, diffuse intraperitoneal disease, and has thus been largely used in ovarian cancer,38 with less common application in intraperitoneal gastrointestinal malignancies or mesothelioma.39 Drugs used in intraperitoneal therapy include cisplatin, carboplatin, 5-fluorouracil (5-FU), and paclitaxel. Recently, a large trial of intraperitoneal cisplatin and paclitaxel in optimally debulked stage III ovarian cancer reported a significant survival benefit,40 suggesting its incorporation into standard treatment (see also Chapter 36).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree