Acquisitions Editor: Robert Hurley
Product Manager: David Murphy Jr.
Production Manager: Alicia Jackson
Senior Manufacturing Manager: Benjamin Rivera
Marketing Manager: Lisa Parry
Design Coordinator: Teresa Mallon
Production Services: Maryland Composition/ASI
© 2009 by LIPPINCOTT WILLIAMS&WILKINS, a WOLTERS KLUWER business
530 Walnut Street
Philadelphia, PA 19106 USA
LWW.com
All rights reserved. This book is protected by copyright. No part of this book may be reproduced in any form by any means, including photocopying, or utilized by any information storage and retrieval system without written permission from the copyright owner, except for brief quotations embodied in critical articles and reviews. Materials appearing in this book prepared by individuals as part of their official duties as U.S. government employees are not covered by the above-mentioned copyright.
Printed in the People’s Republic of China
Library of Congress Cataloging-in-Publication Data
ISBN 978-0-7817-8458-0
Surgical reconstruction of the diabetic foot and ankle / Thomas Zgonis.—1st ed.
p. ; cm.
Includes bibliographical references and index.
1. Foot—Surgery. 2. Ankle—Surgery. 3. Diabetes—Surgery. I. Zgonis, Thomas.
[DNLM: 1. Diabetic Foot—surgery. 2. Limb Salvage. 3. Reconstructive Surgical Procedures—methods. WK 835 S9615 2010]
RD563.S88 2010
617.5’85059—dc22
2009003111
Care has been taken to confirm the accuracy of the information presented and to describe generally accepted practices. However, the authors, editors, and publisher are not responsible for errors or omissions or for any consequences from application of the information in this book and make no warranty, expressed or implied, with respect to the currency, completeness, or accuracy of the contents of the publication. Application of the information in a particular situation remains the professional responsibility of the practitioner.
The authors, editors, and publisher have exerted every effort to ensure that drug selection and dosage set forth in this text are in accordance with current recommendations and practice at the time of publication. However, in view of ongoing research, changes in government regulations, and the constant flow of information relating to drug therapy and drug reactions, the reader is urged to check the package insert for each drug for any change in indications and dosage and for added warnings and precautions. This is particularly important when the recommended agent is a new or infrequently employed drug.
Some drugs and medical devices presented in the publication have Food and Drug Administration (FDA) clearance for limited use in restricted research settings. It is the responsibility of the health care provider to ascertain the FDA status of each drug or device planned for use in their clinical practice.
To purchase additional copies of this book, call our customer service department at (800) 6383030 or fax orders to (301) 223-2320. International customers should call (301) 223-2300.
Visit Lippincott Williams&Wilkins on the Internet: at LWW.com. Lippincott Williams&Wilkins customer service representatives are available from 8:30 am to 6 pm, EST.
10 9 8 7 6 5 4 3 2 1
Dedication
To my parents, grandparents, beautiful wife Kristen, and daughters Labrini and
new addition to our family Ioanna Zgonis.
With love
JAMES THOMAS AND RICHARD J. DE ASLA
2 Preoperative and Perioperative Management of the High-Risk Patient with Diabetes Mellitus
ADAM S. LANDSMAN
3 Utility of Nuclear Medicine Imaging in the Diabetic Foot
MOLLY A. SCHNIRRING-JUDGE
4 Elective Surgery for the Neuropathic Diabetic Foot
JOHN M. GIURINI, JEREMY J. COOK, AND EMILY A. COOK
5 Diabetic Lower Extremity Edema and Venous Insufficiency: Differential Diagnosis and Management
CHARLES A. ANDERSEN AND NITEN SINGH
6 Vascular Assessment and Reconstruction of the Ischemic Diabetic Extremity
CHARLES A. ANDERSEN AND NITEN SINGH
7 Surgical Treatment of Chronic Nerve Compression in the Patient with Diabetic Neuropathy
A. LEE DELLON
8 Surgical Management and Stepwise Approach to Diabetic Foot Infections
PHILIP BASILE AND BARRY I. ROSENBLUM
9 Bioengineered Alternative Tissues for the Surgical Management of Diabetic Foot Ulceration
JOHN S. STEINBERG, BRUCE WERBER, AND PAUL J. KIM
10 Negative Pressure Wound Therapy for the Complicated Diabetic Foot Wounds
LUKE C. JEFFRIES, ROBERTO H. RODRIGUEZ, RONALD BELCZYK, AND THOMAS ZGONIS
11 Skin Grafting Techniques for Open Diabetic Foot Wounds
THOMAS S. ROUKIS
12 Local Random Flaps for Soft Tissue Coverage of the Diabetic Foot
PETER A. BLUME AND JONATHAN J. KEY
13 Muscle Flaps for Soft Tissue Coverage of the Diabetic Foot
JOHN J. STAPLETON, THOMAS ZGONIS, GARY PETER JOLLY, AND THANOS BADEKAS
THOMAS ZGONIS, JOHN J. STAPLETON, AND IOANNIS PAPAKOSTAS
15 Free Flaps for Soft Tissue Coverage of the Diabetic Foot
DEOWALL CHATTAR-CORA, STANLEY A. OKORO, AND DOUGLAS T. CROMACK
16 Equinus Deformity and the Diabetic Foot
PAUL J. KIM AND THOMAS J. CHANG
17 Surgical Reconstruction of the Failed Tendo-Achilles Lengthening
NEAL M. BLITZ
18 Surgical Reconstruction and Stepwise Approach to Acute Charcot Neuroarthropathy
BRADLEY M. LAMM
19 Surgical Reconstruction and Stepwise Approach to Chronic Charcot Neuroarthropathy
WILLIAM P. GRANT AND GLENN M. WEINRAUB
20 Intramedullary Nail Fixation for Reconstruction of the Hindfoot and Ankle in Charcot Neuroarthropathy
ALAN R. CATANZARITI AND ROBERT W. MENDICINO
21 Surgical Management of Malunions and Nonunions of the Diabetic Neuropathic Lower Extremity
PATRICK R. BURNS AND RICK L. SCANLAN
22 Bone Grafting and Orthobiologics for Reconstruction of the Diabetic Lower Extremity
JOHN JOSEPH ANDERSON
23 Bone Growth Stimulation in Complex Diabetic Reconstructive Surgery
JOHN JOSEPH ANDERSON AND THOMAS ZGONIS
24 Revisional and Reconstructive Surgery for the Diabetic Foot and Ankle
THOMAS ZGONIS, JOHN J. STAPLETON, VASILIOS D. POLYZOIS, AND ENZO J. SELLA
25 Diabetic Neuropathic Forefoot, Midfoot, and Hindfoot Osseous Trauma and Dislocations
LUIS E. MARIN, LAWRENCE A. DIDOMENICO, VINCENT J. MANDRACCHIA, AND THOMAS ZGONIS
26 Diabetic Neuropathic Pilon and Ankle Osseous Trauma and Dislocations
LUIS E. MARIN, LAWRENCE A. DIDOMENICO, EMMANOUIL D. STAMATIS, AND THOMAS ZGONIS
27 Surgical Management of Postoperative Infections and Complications
LAURENCE G. RUBIN AND CHARLES M. ZELEN
28 A Stepwise Approach to Diabetic Foot and Ankle Amputations
BORA RHIM, BABAK BARAVARIAN, AND THOMAS ZGONIS
29 Rehabilitation and Therapeutic Footwear for the Reconstructed and Amputee Patient
ARMIN KOLLER
Charles A. Andersen, MD, FACS
Chief of Vascular/Endovascular/Limb Preservation Surgery Service
Department of Surgery
Madigan Army Medical Center
Tacoma, Washington
John Joseph Anderson, DPM, FACFAS
Chief of Surgery
Gerald Champion Regional Medical Center
Alamogordo, New Mexico
Thanos Badekas, MD
Director of Orthopedic Foot and Ankle Surgery
Athineon Hospital
Director of Department of Orthopaedics, Police Health Division
Past President, Hellenic Foot and Ankle Society
Athens, Greece
Babak Baravarian, DPM, FACFAS
Chief of Foot and Ankle Surgery
Santa Monica/UCLA and Orthopedic Hospital
Assistant Clinical Professor, UCLA School of Medicine
Director, University Foot and Ankle Institute
Los Angeles, California
Philip Basile, DPM, FACFAS
Clinical Instructor of Surgery
Harvard Medical School
Co-Director, Harvard Podiatric Reconstructive and Research
Fellowship
Beth Israel Deaconess Medical Center
Boston, Massachusetts
Chief of Podiatry
Department of Surgery
Mount Auburn Hospital
Cambridge, Massachusetts
Ronald Belczyk, DPM
Clinical Instructor of Orthopaedic Surgery
Division of Podiatric Medicine and Surgery
Fellow in Reconstructive Foot and Ankle Surgery
The University of Texas Health Science Center at San Antonio
San Antonio, Texas
Neal M. Blitz, DPM, FACFAS
Chief of Foot Surgery
Department of Orthopaedic Surgery
Bronx-Lebanon Hospital Center
Bronx, New York
Peter A. Blume, DPM, FACFAS
Clinical Assistant Professor of Surgery, Anesthesia, and
Orthopedics/Rehabilitation
Yale School of Medicine
Director of North American Center for Limb Preservation
New Haven, Connecticut
Patrick R. Burns, DPM, FACFAS
Clinical Assistant Professor of Orthopaedic Surgery
Division of Foot and Ankle Surgery
University of Pittsburgh School of Medicine
Director of Podiatric Surgical Training
University of Pittsburgh Medical Center South Side Hospital
Pittsburgh, Pennsylvania
Alan R. Catanzariti, DPM, FACFAS
Director of Residency Training
Division of Foot and Ankle Surgery
The Western Pennsylvania Hospital
Pittsburgh, Pennsylvania
Thomas J. Chang, DPM, FACFAS
Clinical Professor and Past Chairman of Podiatric Surgery
California College of Podiatric Medicine at Samuel Merritt College
Oakland, California
Deowall Chattar-Cora, MD
Department of Orthopedic Surgery
Division of Plastic and Reconstructive Surgery
University of Texas Health Science Center at San Antonio
San Antonio, Texas
Plastic and Reconstructive Surgery of Puerto Rico
San Juan, Puerto Rico
Emily A. Cook, DPM
Clinical Instructor, Surgery
Harvard Medical School
Harvard Podiatric Reconstruction and Research Fellow
Beth Israel Deaconess Medical Center Boston, Massachusetts
Jeremy J. Cook, DPM
Clinical Instructor or Surgery
Harvard Medical School
Harvard Podiatric Reconstruction and Research Fellow
Beth Israel Deaconess Medical Center
Boston, Massachusetts
Douglas T. Cromack, MD
Assistant Professor of Orthopedic Surgery
Division of Plastic and Reconstructive Surgery
University of Texas Health Science Center at San Antonio
San Antonio, Texas
Richard J. de Asla, MD
Co-Director of Foot and Ankle Division
Department of Orthopaedic Surgery
Massachusetts General Hospital
Instructor, Harvard Medical School
Boston, Massachusetts
Professor of Plastic Surgery and Neurosurgery
Johns Hopkins University
Director of Dellon Institutes for Peripheral Nerve Surgery
Baltimore, Maryland
Lawrence A. DiDomenico, DPM, FACFAS
Adjunct Professor and Director of Reconstructive Rearfoot and
Ankle Surgical Fellowship
Ohio College of Podiatric Medicine
Cleveland, Ohio
John M. Giurini, DPM, FACFAS
Associate Professor of Surgery
Harvard Medical School
Chief of Podiatric Surgery
Department of Surgery
Beth Israel Deaconess Medical Center
Boston, Massachusetts
William P. Grant, DPM, FACFAS
Instructor of Surgery
Eastern Virginia Medical School
Norfolk, Virginia
Fellowship Director, Diabetic Limb Salvage
Tidewater Foot and Ankle Center
Virginia Beach, Virginia
Luke C. Jeffries, DPM
Former Reconstructive Foot and Ankle Surgery Fellow and Clinical
Instructor
Department of Orthopaedic Surgery
Division of Podiatric Medicine and Surgery
The University of Texas Health Science Center at San Antonio
San Antonio, Texas
Private Practice
Exeter, New Hampshire
Gary Peter Jolly, DPM, FACFAS
Clinical Professor of Surgery
Des Moines University, College of Podiatric Medicine and Surgery
Des Moines, Iowa
Director of Reconstructive Foot and Ankle Surgery
New Britain General Hospital
New Britain, Connecticut
Jonathan J. Key, DPM, FACFAS
Clinical Assistant Professor of Orthopaedics and Rehabilitation
Yale University School of Medicine
New Haven, Connecticut
Paul J. Kim, DPM
Assistant Professor of Podiatric Medicine and Surgery
Midwestern University
Glendale, Arizona
Armin Koller, MD
Chief of Technical Orthopaedics
Mathias-Hospital
Rheine, Germany
Bradley M. Lamm, DPM
Head of Podiatry
Director of Podiatric Residency Program
Rubin Institute for Advanced Orthopedics
International Center for Limb Lengthening
Sinai Hospital of Baltimore
Baltimore, Maryland
Adam S. Landsman, DPM, PhD, FACFAS
Assistant Professor of Surgery
Harvard Medical School
Beth Israel Deaconess Medical Center, Division of Podiatric Surgery
Boston, Massachusetts
Vincent J. Mandracchia, DPM, MHA, FACFAS
Clinical Professor of Podiatric Medicine and Surgery
Des Moines University
Senior Vice President and Chief Medical Officer
Department of Surgery, Foot and Ankle Surgery
Broadlawns Medical Center
Des Moines, Iowa
Luis E. Marin, DPM, FACFAS
Director of Podiatric Surgical Residency Program
Palmetto General Hospital
Hialeah, Florida
Robert W. Mendicino, DPM, FACFAS
Chief of Foot and Ankle Surgery
The Western Pennsylvania Hospital
Pittsburgh, Pennsylvania
Vasilios D. Nicolaides, MD
Fourth Department Head, Orthopaedic Surgery
KAT General Hospital
Athens, Greece
Stanley A. Okoro, MD, FACS
Division of Plastic and Reconstructive Surgery
University of Texas Health Science Center at San Antonio
San Antonio, Texas
Ioannis Papakostas, MD, PhD, MSc
Department of Orthopaedic Surgery
Thiva General Hospital
Thiva, Greece
Vasilios D. Polyzois, MD, PhD
Chief of Orthopaedic Traumatology
KAT General Hospital
Athens, Greece
Bora Rhim, DPM
Clinical Instructor, VA Medical Center
Staff Physician, University Foot and Ankle Institute
Los Angeles, California
Roberto H. Rodriguez, DPM
Former Reconstructive Foot and Ankle Surgery Fellow, Clinical
Instructor, and Assistant Professor
Division of Podiatric Medicine and Surgery
Department of Orthopaedic Surgery
The University of Texas Health Science Center at San Antonio
San Antonio, Texas
Barry I. Rosenblum, DPM, FACFAS
Assistant Clinical Professor, Surgery
Harvard Medical School
Director of Podiatric Surgical Residency
Beth Israel Deaconess Medical Center
Boston, Massachusetts
Chief of Limb Preservation Service, Vascular, and Endovascular
Surgery Service
Department of Surgery
Madigan Army Medical Center
Tacoma, Washington
Laurence G. Rubin DPM, FACFAS
Private Practice
Richmond, Virginia
Rick L. Scanlan, DPM, FACFAS
Chief of Podiatry Section
Faculty of Podiatric Surgical Training Program
University of Pittsburgh Medical Center South Side Hospital
Pittsburgh, Pennsylvania
Molly A. Schnirring-Judge, DPM, FACFAS
Director of Podiatric Clerkship Program
Department of Surgery
St. Vincent Charity Hospital
Cleveland, Ohio
Enzo J. Sella, MD
Associate Clinical Professor of Orthopaedics and Rehabilitation
Yale University School of Medicine
Co-Director of Foot and Ankle Clinics
Yale New Haven Hospital
Section Chief of Orthopaedics
St Raphael Hospital
New Haven, Connecticut
Niten Singh, MD
Chief of Endovascular Surgery
Vascular/Endovascular/Limb Preservation Surgery Service
Department of Surgery
Madigan Army Medical Center
Tacoma, Washington
Emmanouil D. Stamatis, MD
Department of Orthopaedic Surgery
401 General Army Hospital
Athens, Greece
John J. Stapleton, DPM
Former Reconstructive Foot and Ankle Surgery Fellow and Clinical
Instructor
Department of Orthopaedic Surgery
Division of Podiatric Medicine and Surgery
The University of Texas Health Science Center at San Antonio
San Antonio, Texas
Associate of Foot and Ankle Surgery
VSAS Orthopaedics
Allentown, Pennsylvania
Clinical Assistant Professor of Surgery
Pennsylvania State College of Medicine
Hershey, Pennsylvania
John S. Steinberg, DPM, FACFAS
Assistant Professor of Plastic Surgery
Georgetown University Hospital
Washington, DC
James L. Thomas, DPM, FACFAS
Associate Professor of Orthopaedic Surgery,
Department of Orthopaedic Surgery,
West Virginia University School of Medicine,
Morgantown, WV
Glenn M. Weinraub, DPM, FACFAS
The Permanente Medical Group
Department of Orthopaedic Surgery
Fremont/Hayward, California
Clinical Associate Professor
Midwestern University, School of Podiatric Medicine
Glendale, Arizona
Bruce Werber, DPM, FACFAS
Associate Professor
Midwestern University
Glendale, Arizona
Charles M. Zelen, DPM, FACFAS
Clinical Assistant Professor of Internal Medicine
University of Virginia School of Medicine
Podiatry Section Chief
Department of Surgery
Carilion Medical Center
Podiatry Section Chief
Department of Orthopedics
HCA Lewis Gale Hospital
Roanoke, Virginia
Thomas Zgonis, DPM, FACFAS
Associate Professor, Department of Orthopaedic Surgery
Chief, Division of Podiatric Medicine and Surgery
Director, Podiatric Surgical Residency and Reconstructive Foot and
Ankle Fellowship
The University of Texas Health Science Center at San Antonio
San Antonio, Texas
Contemporary medical management of diabetic patients has become increasingly dependent on the expertise of clinicians from multiple disciplines. Education and prevention remain the foundation of care; however millions of people in this country, and round the world live with diabetes every day. While we pray for a cure, as clinicians we will continue to face the many sequelae of this terrible disease. In this text Dr. Zgonis and his distinguished panel of contributing authors have eloquently articulated a detailed, logical, and pragmatic methodology for evaluating and treating diabetic pathology of the foot and ankle. The title, Surgical Reconstruction of the Diabetic Foot and Ankle may lead the reader to infer that this is purely a surgical text. My primary goal in penning this foreword is to accurately convey the truly comprehensive nature of this tome.
It is important to understand the background that inspired Dr. Zgonis to embark on this project. Through the leadership of Dr. Zgonis, our institution has assembled dozens of faculty from over 14 disciplines to form a center of excellence for the treatment of diabetic foot and ankle disease.
This text is a natural progression of his efforts to raise awareness and educate both patients and clinicians about a patient centric, integrated multi-disciplinary approach to the clinical and surgical care of the diabetic patient. The authors cover a broad foundation of topics including: pre/perioperative care, use of diagnostic imaging, negative pressure wound therapy, management of post operative complications, and a stepwise approach to foot and ankle amputations and infections. The evaluation and treatment of the diabetic neuropathic foot is extensively covered, particularly the surgical reconstruction of acute and chronic neuroarthropathy, nonunions, malunions, and management of acute trauma in the neuropathic extremity.
Equal attention is given to the ischemic extremity with in depth discussion of vascular insufficiency, vascular reconstruction, and the entire range of treatment options for soft tissue coverage. Advances in surgical techniques and fixation have improved limb salvage rates for diabetic patients. The contributing authors provide a compelling overview of revisional and reconstructive surgery for the foot and ankle with an emphasis on external fixation.
For students and experienced clinicians alike, Surgical Reconstruction of the Diabetic Foot and Ankle will improve the quality of care and patient outcomes by providing a comprehensive stepwise approach for managing even the most complicated diabetic patients.
Daniel W. Carlisle, MD
Chairman and Orthopaedic Residency Program Director
University of Texas Health Science Center at San Antonio
It is with a certain respect, appreciation, and honor to write this preface for my first edition of the Surgical Reconstruction of the Diabetic Foot and Ankle. I feel obligated to thank many individuals throughout my academic journey that have helped me achieve my goals and also publish this unique textbook. I also want to thank my family for their continuous support and share with you my personal background and heritage.
Being raised in a Greek-American family, I had the opportunity to spend most of my childhood in a very small village in the northern part of Greece called Rodia, a suburb of Grevena, Greece. During that time, my parents remained mostly in the United States while my sister and I started school in Greece. My grandfather was the most influential person in my life since he taught me so many things through an era of poverty, hard work, and lack of education. Growing up in a village with a little more than 500 people and with the influence of my grandparents, I learned the three most important values in life that were taught to me by my grandfather: faith, family, and education. Up to this date, I always remember and sometimes still hear his voice about the meaning of life.
After high school, I eagerly returned back to where I was born in the United States and joined my family in Boston, Massachusetts. I can still vividly remember the difficulty of adjusting to a new environment and most importantly the challenges that I had to face with the language barrier and education. Throughout all these years, I tried to accomplish all of my degrees and training and also portray to my grandfather that I was still working very hard and was very appreciative of his daily teachings and wisdom that created and shaped my personality and work ethic.
Accepting a position as an Assistant Professor within the Department of Orthopaedics, Division of Podiatric Medicine and Surgery at the University of Texas Health Science Center (UTHSC) in San Antonio, Texas, was one of my biggest turning points in my academic career. My podiatric surgical residency director (Dr. Clinton Lowery) at the University of Pittsburgh Medical Center in Pittsburgh, Pennsylvania and reconstructive foot and ankle fellowship directors (Drs Jolly and Blume) at the New Britain General Hospital, New Britain, Connecticut and Yale New Haven Hospital, New Haven, Connecticut were some of my colleagues that encouraged me to return to academics and focus on teaching, research and service to the public and the profession. This move was made possible with the help and leadership of Dr. Lawrence Harkless who personally guided me throughout my tenure at UTHSC – San Antonio, Texas which is now led by the chairman of the department of orthopaedics Dr. Daniel W. Carlisle.
I am also obligated and honored to mention Dr. Polyzois’ family and their contribution to my academic journey. Dr. Demetrios Polyzois who is the current president of the Hellenic College of Orhopaedic Surgeons and his son Dr. Vasilios Polyzois who serves as the chief of orthopaedic traumatology at KAT General Hospital in Athens, Greece are two individuals who have taught me so much in diabetic limb salvage through the use of external fixation methods. Their friendship, professionalism, and astute experience in the use of external fixation have made me return to Greece on a yearly basis and also take time to visit the small village where I grew up in memory of my grandparents.
My goal in an academic environment with a very large diabetic population in need of diabetic foot treatment was to establish a Center of Excellence where all patients were seen and treated by all specialties. As diabetes mellitus has now been described by many as an epidemic and with more lower extremity amputations being performed as a result of diabetes related complications, the need of awareness and patient and health care education were my goals through the first edition of this reconstructive book.
A multidisciplinary team of authors has been gathered to share their expertise and approach to some of the most difficult case scenarios in dealing with the diabetic foot and ankle. The importance of a major health care system or academic institution is also emphasized throughout the textbook. Topics that address the diabetic patient’s vascular status, infection, medical management, trauma, soft tissue coverage, and reconstruction are presented by many specialists in the field of their expertise. Being in an academic institution, I always teach the students, residents, and fellows that the diabetic foot represents a direct image of the patient’s overall health status.
In conclusion, I hope that this textbook will raise awareness to the public and health care professionals and to also help guide you through the most challenging reconstructive cases in patients with diabetes mellitus. Education, prevention, and continuous teamwork by all specialties will only bring promising results to this devastating disease and its related complications.
TZ
I would like to thank the Acquisitions Editor, Robert Hurley; Managing Editor, Dave Murphy; Director of Marketing, Sharon Zinner; Production Editor, John Larkin; Design Manager,Teresa Mallon; and all the members of the Production Services group involved with this text for their great support and guidance throughout the project.
TZ
INTRODUCTION
Over the past two decades, a gradual trend toward an increasing aggressiveness in diabetic limb salvage has been seen worldwide. The reasons for this are at a minimum twofold. The first is the improved technology and surgical techniques available to treat diabetic foot complications. These have allowed for earlier and more accurate diagnosis of pathology, as well as more alternatives in wound healing and definitive surgical care. The other likely reason is the increased awareness of the problem at hand. It is now known that as late as 2005, 7% of the U.S. population was estimated to have diabetes, a total of nearly 20.8 million people. Of this number, almost 6.2 million were not aware that they had diabetes, and it is estimated that an additional 1.5 million people will be diagnosed with diabetes yearly (1,2). More specific to limb salvage, it is known that following lower extremity amputation in the diabetic patient, there is a 1-year mortality rate between 11% and 41%; the 5-year rate is between 39% and 68% (3). Most and Sinnock (4) found in 1983 that amputation occurred at an age-adjusted rate of 15 times higher in the diabetic population. The overall estimated rate was 59.7 per 10,000 in the diabetic population, with this rate increasing to 101.4 per 10,000 in diabetic patients 65 years and older (4–6). Also, even for healed diabetic foot ulcers, there is a recurrence rate of 34%. The recurrence rate increases to 61% at 3 years and up to 70% at 5 years (7).
Possibly the most challenging aspect of limb salvage in the diabetic foot is the multifactorial causation of the presenting pathology. Indeed, it has been shown that for patients admitted to the hospital for diabetic foot complications, less than 14% received adequate lower extremity evaluations (8). Some form of structured organization or system is best suited to address the multiple factors involved, which include a compromised immune system, peripheral vascular disease, peripheral neuropathy, and numerous other medical conditions that may be present (9). A “micro system of care” has been described by Nelson et al (10). This is defined as a “system of policies, staff, and technology within the overall healthcare system or medical center that focuses on a specific patient population with a narrow need or condition” (9,10). Within this “system” exists the multidisciplinary approach to limb salvage in the diabetic patient. In the multidisciplinary setting, the various risk factors can all be addressed, including neuropathy, ischemia, and infection. Local factors such as high pressures producing ulceration can be addressed and the “basics” of limb salvage can be accomplished, including patient assessment, medical management/stabilization, wound care, treatment of infection and ischemia, foot-sparing surgery, and prevention (11). Acute problems can also be more efficiently managed and coordinated by providing the medical center with a link to a multidisciplinary team of specialists, with subsequent reduction in hospital length of stay, morbidity, and loss of limb (11,12). This allows standardization of the management approach in a more efficient manner. When done in the setting of an academic medical center, this approach also provides for the utilization of the existing infrastructure to design and implement clinical research trials and more coordinated educational venues (12).
A careful review of the literature reveals that the multidisciplinary approach to the diabetic foot, especially in the academic setting, is not new. This method has proven to be very effective in a variety of ways. Improved outcomes and decreased rates of lower extremity amputation as well as reduced lengths of hospital stay have been shown to occur with a multispecialist approach (11). The utilization of the best available professional expertise has been shown to be a cost-effective delivery of care and also reduces amputation rates and hospital length of stay (13–15). This approach is especially beneficial in the inpatient setting, in which one study showed that at any given time approximately 25% of inpatients have diabetes and of these approximately 20% have some form of foot pathology that required acute care or follow-up management upon discharge (16). Ziran et al (17) reported improved outcomes when patients with osteomyelitis were followed by a team, including an orthopaedic surgeon and a musculoskeletal infectious disease specialist. Wrobel et al (18) showed that patients within the Veterans Administration (VA) system receiving care at facilities with high levels of feedback coordination and programming had significantly lower rates of amputation. Robbins et al (9) found that after implementing a team approach protocol, the rate of major amputations decreased from 2.15 in 2001 to 1.42 in 2004. DeNamur et al (19) reported on 19 diabetic patients undergoing limb salvage in cases of varying complexity. All patients studied were either scheduled for, or at risk for, a major amputation. Eighteen of the 19 patients avoided major amputation after undergoing intervention via a multidisciplinary team approach at a teaching institution. Limb salvage rates of 65%, 72%, and 81% with multidisciplinary treatment strategies have been reported in three separate studies with 3-year follow-up (7,20,21).
A multidisciplinary setting is also beneficial in the outpatient setting in the treatment of diabetic foot pathology and the follow-up of the limb salvage patient. Utilizing this approach, Keyser (22) reported an 88% rate of healing of initial diabetic foot ulcers in an outpatient wound care program and a 93% salvage rate of the contralateral limb after unilateral major lower extremity amputation. There is some evidence to suggest that outpatient screening may result in more distal amputation by discovering foot pathology earlier (9). Holstein et al (23) found that with the establishment of a multidisciplinary diabetic foot clinic, there resulted a 75% reduction in the incidence of major amputations.
The multidisciplinary team approach has also been shown to be significantly effective regarding the cost of healthcare provided when treating diabetic foot pathology and pursuing limb salvage. Ortegon et al (24) showed that the combination of effective diabetic foot care and intensive glycemic control reduced the rate of amputation by approximately 58%. Their study also revealed a cost per quality-adjusted life year gained of $12,165. Other studies have also shown limb salvage to be cost-effective as the more proximal an amputation is performed, the higher the respective rehabilitation and prosthetic costs (25,26). When these data are combined with reduced length of stay figures, the economic impact is obvious. Clinical practice guidelines (CPGs) for treating diabetic foot pathology can also contribute significantly to effective management and cost containment by promoting timely consults and referrals by the appropriate specialty (27,28). Secondary to the wide range of specialty care and ancillary services available in a major academic healthcare environment, CPGs are ideally suited to provide efficient management of the limb salvage patient and can be easily implemented and followed.
The multispecialty team approach to diabetic limb salvage is the most important tool to ensure adequate inpatient and outpatient care in a cost-effective and well-managed setting. It should be the standard of care in major academic healthcare institutions and any facility providing diabetic limb salvage services.
SPECIALTY CARE INVOLVED IN THE MULTIDISCIPLINARY TEAM SETTING
The multidisciplinary team approach to limb salvage allows for the identification of the classification, duration, and level of control of diabetes and promotes the investigation of any cardiovascular risk factors and other diabetes-related complications (16). Secondary to the fact that distal foot amputation is favored as opposed to major amputation in diabetic patients who have significant comorbidities, an array of specialists may be required for patients undergoing the limb salvage process. It has been estimated that at least 50% of amputations can be prevented within the diabetic population by providing a coordinated effort to include aggressive treatment of early lesions, arterial revascularization as needed, a reduction in risk factors, patient education, and proper outpatient care (11). This can be accomplished by the “talents of numerous specialists committed to preserving the extremities of patients with diabetes being brought together in a cohesive unit that cannot only provide efficient coordination of services for the acutely infected or ischemic patient, but also which can provide ongoing outpatient management focused on prevention, education, and early intervention.” Frykberg has identified intrinsic and extrinsic risk factors for the diabetic foot (11). These include not only neuropathy and ischemia, but also age, weight, nephropathy, disorders of visual acuity, decreased joint mobility, structural deformity, high plantar pressures, etc. These factors clearly delineate the need for multispecialty involvement.
The establishment of the multidisciplinary team is the most critical step in providing comprehensive, efficient, and cost-effective treatment in the diabetic limb salvage effort. The following list is the core group of specialists and personnel used in the academic healthcare medical center setting that are necessary to provide a coordinated process of care that is patient-centered: podiatrist, orthopedist, internist, endocrinologist (diabetologist), infectious disease specialist, cardiologist, nephrologist, vascular surgeon, ophthalmologist, plastic surgeon, nursing staff, nutritionist, interventional and noninterventional radiologist, and pedorthist/orthotist. This list certainly can be modified or expanded on, depending on the respective healthcare center setting in which the multidisciplinary approach is being used. In addition, psychiatry and a pain medicine specialist can be very beneficial. A number of ancillary services are also critical to complete the multidisciplinary approach. The following is a compact summarized breakdown of the respective areas that can be covered by the individual specialties and services.
- Podiatrist: A podiatric surgeon can often function as the “gatekeeper” of the team (Fig. 1.1). This role can also be accomplished by the internist or orthopedist with a dedicated foot and ankle practice. The gatekeeper role is extremely important in assuring that proper and timely consults and referrals are accomplished. The podiatrist can function in a number of areas, such as patient education, as well as prevention and offloading and care of ulcerations, including meticulous wound care, débridement of necrotic tissue, and prompt abscess drainage (13). The podiatric surgeon may also engage in the definitive surgical management in the limb salvage pathway, including major reconstructive procedures, various plastic surgical techniques, and even prophylactic diabetic foot surgery in some cases.
- Orthopedist: An orthopaedic surgeon with a dedicated foot and ankle practice may function in a similar role as the podiatric surgeon, including both preventative care and definitive surgical care for limb salvage.
- Internist: Many times the internal medicine specialist is the initial provider to the diabetic patient undergoing limb salvage. They are essential in the control of hyperglycemia, hypertension, and renal and cardiac disease. Noninterventional management of lower extremity ischemia at times may be undertaken by the internist, including the use of anticoagulants or thrombolytic therapy (12). Pharmacologic agents such as bisphosphonates may also be used in the setting of the Charcot foot.
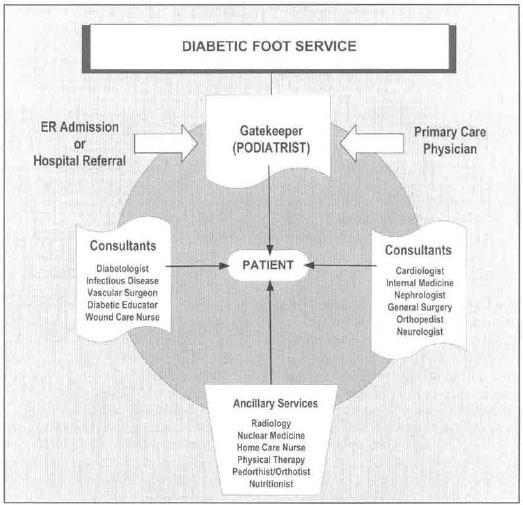
Figure 1.1 The important role of the multidisciplinary team approach to diabetic limb salvage. (From Frykberg RG, Zgonis T, Armstrong DG, et al. Diabetic foot disorders. A clinical practice guideline [2006 revision]. J Foot Ankle Surg 2006;45(5):S-17, Fig. 5, with permission.)
- Endocrinologist: Subspecialty care by the endocrinologist can prove very beneficial, especially in the difficult to control hyperglycemic limb salvage patient.
- Infectious disease specialist: The role of the infectious disease specialist has evolved and expanded in the treatment of diabetic lower extremity infections, especially with the emergence of many antibiotic-resistant organisms and the potential for multiorganism involvement in the diabetic patient. Appropriate antibiotic selection and dosage is crucial in the operative and nonoperative treatment of osteomyelitis as well as soft tissue infections, especially in patients with immunopathy or those who are on immuno-suppressive medications.
- Cardiologist: Cardiovascular risk factor management must be undertaken for successful limb salvage. Patients with valvular disease or those who have undergone valve replacement present unique problems in the surgical management of the limb salvage patient.
- Nephrologist: End-stage renal disease is not uncommon in this patient population. Management of the patient on renal dialysis or the post–renal transplant patient can be complicated, including the adjustment of pharmacologic agent dosing (in particular, antibiotics) and the management of immunosuppressive agents.
- Vascular surgeon: Since insufficient vascular perfusion almost always results in a nonhealing wound, the vascular specialist assumes a critical management role in diabetic limb salvage (12). The incidence of peripheral arterial occlusive disease in diabetic patients is fourfold that of nondiabetic patients and is obviously noted to be a key component in the causal pathway to amputation (28). Sumpio et al (12) showed that when a multidisciplinary approach to limb salvage was used, the number of surgical procedures for aortoiliac occlusive disease, including aorto-bifemoral, axillafemoral, ileofemoral, or femoral-femoral bypasses more than doubled. A significant increase in infrainguinal reconstructions also occurred, as well as a relative decline in numbers of major amputations. The vascular specialist may not only be involved in the perfusion of an ischemic limb, but may also address the less common scenario of venous insufficiency and its impact on limb salvage.
- Ophthalmologist: Retinopathy and disturbances of visual acuity can have a negative impact on balance and gait.
- Plastic surgeon: Wound coverage is an integral part of limb salvage. Besides providing wound coverage, plastic surgical repair may help avoid inelastic scar tissue over wounds, which is many times the result of secondary wound healing. In particular, different forms of local flaps result in greater exposure and visualization and may eliminate the need for additional incisions (12). This role also may be performed by the orthopaedic or podiatric surgeon with the proper training and experience in this area.
- Nursing staff: Nursing input is invaluable in the limb salvage effort. Important areas of contribution range from wound care and patient and family education to discharge planning and home healthcare.
- Nutritionist: Achievement of adequate dietary demands must be met not only to achieve strict glycemic control, but also to accomplish expedient wound healing (protein level, sufficient vitamin intake, etc.).
- Interventional and noninterventional radiologists: Expert diagnostic imaging for osteomyelitis and in the ischemic extremity is absolutely necessary. A dedicated musculoskeletal radiologist is usually available in the academic healthcare medical center setting and may add invaluable information with a variety of imaging techniques. Timely angiographic studies and other interventional techniques are of obvious necessity to assure a successful limb salvage procedure when vascular perfusion is compromised.
- Pedorthist/Orthotist: Pedorthic/orthotic care is not only paramount in the postoperative treatment of the limb salvage patient, but is also extremely important when employed as a preventative tool. Significant decrease in plantar foot pressures are known to occur with the use of various types of insoles (custom total contact, accommodative, etc.) as well as by shoe modifications such as rocker bottom soles. Therapeutic shoe wear may often help in accommodating foot deformity from Charcot neuroarthropathic changes.
Additional specialty areas of psychiatry, pain management and geriatric medicine may complement the multidisciplinary team when dealing with issues of depression, fear, anger, and intractable neuropathic pain and in the ever-growing numbers of geriatric diabetic patients.
- Ancillary services: Important services that complement the preceding specialists are a vital part of the team approach. These include, but are not limited to, clinical laboratory services, vascular laboratory services, physical therapy, transplant service, intensive care units and well-trained and experienced cast technicians for applying total contact casts, etc. Although not always found in the academic healthcare setting, hyperbaric oxygen units may also be beneficial.
All of these specialties and services are integral in the multidisciplinary approach to limb salvage. As mentioned, at times there may be overlap in services or one role may be able to be filled by more than one specialty. Regardless, the individual healthcare provider must be qualified and the team approach must always be patient centered.
To this end, dedicated diabetic foot clinics in academic centers have a number of advantages. One such benefit, true of any dedicated center, is a devoted focus and awareness given to the problem. This typically results in an ability to coordinate the expertise required for comprehensive treatment. In an academic setting, most relevant services are under one roof. In theory, this should result in improved efficiency not only in delivering care but also in limiting the number of return visits required by patients, which in turn, improves compliance. Generally, the culture of an academic setting fosters a greater emphasis on research. Such centers have established institutional review boards (IRB) overseeing safety and ethical research practice. Also, other helpful resources such as patient recruitment, advertising, and biostatistics tend to be more available. This ethos combined with a system that sees large volumes of patients with similar pathology provides an ideal environment for promoting clinical studies. Finally, academic centers are the preferred referral centers in most regions when care of the medically complex patient is required. Managing the multisystemic effects of diabetes is labor intensive. In major academic centers, often, the day-to-day management of inpatient care for this difficult population falls on residents and fellows and their efforts cannot be overstated. Daily wound inspections, dressing changes, débridements, lab data gathering, performing timely blood cultures, and routine medication management are examples of the tasks typically performed by the house staff.
CASE REPORT
A 65-year-old diabetic woman presented to clinic with a 2-year history of a progressive varus deformity of the left foot and ankle secondary to diabetic Charcot neuroarthropathy. The patient ambulated with weight bearing to the lateral malleolus and had been treated with extensive wound care and bracing for a chronic nonhealing ulcer over the distal lateral malleolus for 13 months (Fig. 1.2). Previous diagnostic imaging and bone biopsy confirmed osteomyelitis of the distal fibula. Bone cultures showed multiple organisms, including methicillin-resistant Staphylococcus aureus. Besides diabetes mellitus, this patient’s past medical history included peripheral vascular disease now status post–femoral-popliteal bypass of the left side, status post–aortic valve replacement, hypertension, end-stage renal failure now on renal dialysis, and coronary artery disease. Secondary to her chronic infection, nonhealing ulcer, and nonbraceable deformity, amputation had been recommended to her by other surgeons.
After proper clinical evaluation, it was determined that this patient would be a potential limb salvage candidate and she was coadmitted to the podiatry and internal medicine service secondary to her coexisting medical problems. Preoperative work-up was accomplished including the input of vascular surgery (to assure patency of her graft), nephrology (to manage her renal disease and provide inpatient dialysis), cardiology (to manage her anticoagulant therapy secondary to her valve replacement and associated risk factors), radiology (to review old and new imaging studies), and infectious disease (to assist with antibiotic choice and dosage). Clinical, cardiac, and vascular laboratory services were used. After surgical clearance was achieved, limb salvage was undertaken. Talectomy was performed along with tibiocalcaneal arthrodesis and distal lateral malleolus and ulcer resection (Fig. 1.3). Fixation was achieved with an external ring fixator, which provided good stability and allowed the arthrodesis to heal with a plantigrade foot (Fig. 1.4). Postoperative care included extensive patient and family education by nursing team members and follow-up pedorthic and orthotic care.

Figure 1.2 Intraoperative picture showing the severe left Charcot ankle fracture-dislocation with evidence of osteomyelitis. Patient presented with several comorbidities including coronary arterial disease and end stage renal disease. Patient was cleared by all medical services before her limb salvage procedure.
CONCLUSION
Foot ulcers are a major cause of morbidity and cost in the diabetic population. Therefore, prevention should be of paramount importance. If an ulcer develops, then treatment must be initiated at the earliest possible stage and implemented with a comprehensive understanding of the risk factors that preceded its development. We believe, and the literature supports, that a multidisciplinary approach is the most effective method of prevention and healing of diabetic foot ulcers with regard to both outcomes and cost. Education, prophylactic measures, and early intervention are the principles driving this effort. To this end, the expertise of a multitude of specialists is coordinated to provide care in both the outpatient and inpatient settings.

Figure 1.3 Intraoperative picture showing the resection of the ankle osteomyelitis and the acute talectomy procedure.

Figure 1.4 Intraoperative picture showing the tibio-calcaneal arthrodesis with the use of a multiplane circular external fixator for compression and long-term stability.
REFERENCES
- Frykberg RG. Prevention of lower extremity amputation in diabetes. Presented at the American Professional Wound Care Association National Conference 2006, April 2006, Philadelphia.
- National Diabetes Information Clearinghouse (National Diabetes Statistics). Available at: diabetes.niddk.nih.gov/dm/pubs/statistics/index.htm. Accessed August 3, 2007.
- Frykberg RG. Prevention of lower-extremity amputation in diabetic patients. Diabetic Microvascular Complications Today May/June 2006;27–30.
- Most RS, Sinnock P. The epidemiology of lower extremity amputations in diabetic individuals. Diabetes Care 1983;6:87–91.
- Palumbo PJ, Melton LJ. “Peripheral Vascular Disease and Diabetes” in Diabetes in America, data compiled 1984(NIH publ. No. 85–1468), US Government Printing Office, Washington, DC, 1985.
- Bild DE, Selby JV, Sinnock P. Lower extremity amputation in people with diabetes: epidemiology and prevention. Diabetes Care 1989;12:24.
- Apelqvist J, Larsson J, Agardh CD. Long-term prognosis for diabetic patients with foot ulcers. J Intern Med 1993;233:24–31.
- Edelson GW, Armstrong DG, Lavery LA, et al. The acutely infected diabetic foot is not adequately evaluated in an inpatient setting. Arch Intern Med 1996;156:2373–2378.
- Robbins JM, Nicklas BJ, Augustine S. Reducing the rate of amputations in acute diabetic foot infections. Cleve Clin J Med 2006;73:679–683.
- Nelson EC, Batalden PB, Mohr JJ, Plume SR. Building a quality future. Front Health Serv Manage 1998;15:3–32.
- Frykberg RG. Team approach toward lower extremity amputation prevention in diabetes. J Am Podiatr Med Assoc 1997;87:305–312.
- Sumpio BE, Aruny J, Blume PA. The multidisciplinary approach to limb salvage. Acta Chir Belg 2004;104:647–653.
- Van Gils CC, Wheeler LA, Mellstrom M. Amputation prevention by vascular surgery and podiatry collaboration in high risk diabetic and non-diabetic patients. The Operation Desert Foot experience. Diabetes Care 1999; 22:678–683.
- Gibbons G, Marcaccio E, Burgess A, et al. Improved quality of diabetic foot care, 1984 vs 1990. Reduced length of stay and cost, insufficient reimbursement. Arch Surg 1983;128:576–581.
- Apelqvist J. Wound healing in diabetes. Outcome and costs. Clin Podiatr Med Surg 1998;15:21–39.
- Wraight PR, Lawrence SM, Campbell DA. Creation of a multidisciplinary, evidence based, clinical guideline for the assessment, investigation and management of acute diabetes related foot complications. Diabetic Med 2005;22:127–136.
- Ziran BH, Rao N, Hall RA. A dedicated team approach enhances outcomes of osteomyelitis treatment. Clin Orthop Rel Res 2003;414:31–36.
- Wrobel JS, Charns MP, Diehr P, et al. The relationship between provider coordination and diabetes-related foot outcomes. Diabetes Care 2003;26: 3042–3047.
- DeNamur C, Pupp G. Diabetic limb salvage: a team approach at a teaching institution. J Am Podiatr Med Assoc 2002;92:457–462.
- Thomson FJ, Veves A, Ashe H, et al. A team approach to diabetic foot care: the Manchester experience. Foot 1991;2:75–82.
- Edmonds ME, Blundell MP, Morris ME. Improved survival of the diabetic foot: the role of a specialized foot clinic. Q J Med 1986;232:763–771.
- Keyser JE. Diabetic wound healing and limb salvage in an outpatient wound care program. South Med J 1993;86:311–317.
- Holstein P, Ellitsgaard N, Olsen BB. Decreasing incidence of major amputations in people with diabetes. Diabetologia 2000;43:844–847.
- Ortegon MM, Redekop WK, Niessen LW. Cost-effectiveness of prevention and treatment of the diabetic foot: a Markov analysis. Diabetes Care 2004;27: 901–907.
- Ollendorf DA, Kotsanos JG, Wishner WJ, et al. Potential economic benefits of lower-extremity amputation prevention strategies in diabetes. Diabetes Care 1998;21:1240–1245.
- Pinzur MS, Stuck R, Sage R, et al. Benchmark analysis on diabetics at high risk for lower extremity amputation. Foot Ankle Int 1996;17:695–700.
- Frykberg RG, Zgonis T, Armstrong DG, et al. Diabetic foot disorders: a clinical practice guideline (2006 revision). J Foot Ankle Surg 2006; 45 (5 suppl):S1–S66.
- Pecoraro RE, Reiber GE, Burgess EM. Pathways to diabetic limb amputation. Basis for prevention. Diabetes Care 1990;13:513–521.
INTRODUCTION
In the year 2000, it was estimated that the prevalence of diabetes would rise from 2.8% to 4.4% by 2030 (1). This is an alarming prediction in light of the high number of complications that are associated with this disease. The US Health and Nutrition Survey further demonstrated that 28.5% of those with diabetes develop peripheral neuropathy, 9.5% develop signs of peripheral arterial disease, and 7.7% develop foot ulcers; approximately three times the frequency observed in non-diabetic individuals (2). As a result of these complications, there were approximately 29,000 diabetics admitted to U.S. hospitals with a diagnosis of cellulitis or infected ulcers, 84,000 admitted for other cellulitis or abscesses of the foot, 217,000 admitted for ulcerations of the lower extremity, 66,000 admitted for osteomyelitis, 134,000 admitted for chronic non-healing ulcers, and 79,000 admitted for lower limb atherosclerosis with ulcers or gangrene in 2002 (3). A staggering percentage of these individuals undergo surgical intervention while in the hospital. Even more are treated as outpatients for less complex problems as well as elective procedures. These numbers do not include the thousands of patients with diabetes admitted for Charcot reconstructions, and other conditions not included in the preceding statistics.
Among patients who develop ulcerations, Apelqvist et al (4) found that 24% required surgery in the form of an amputation at some level, costing an average of $44,790 (for surgery and hospitalization). Other studies have also demonstrated surgical amputation rates in 16% of the cases where ulcers developed (5). Ultimately, when you combine all of the different diabetes-specific complications as well as the nondiabetes-related reasons that people with diabetes may need surgery, it represents millions of cases in the United States alone.
When surgical reconstruction is necessary for diabetic patients, the inherent risks of surgery may be increased if their diabetes is not managed both preoperatively and perioperatively. There are many risks associated with surgery, and these are magnified in patients with diabetes, particularly if they are poorly controlled, and have a history of cardiovascular, renal or other systemic comorbidities. The situation becomes even more complex in the presence of infections or gangrene, and/or when complex reconstructive surgery is needed.
High-risk diabetic patients fall into two broad categories; those who are acutely high risk, and those who are chronically high risk. However, before the specific steps necessary to prepare a high-risk patient for surgery are considered, it is worthwhile to review the optimally prepared patient, along with the barriers in achieving that state.
PREOPERATIVE MANAGEMENT
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree