Premature Rupture of the Membranes
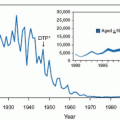
Premature rupture of the fetal membranes (PROM) is one of the most common problems in obstetrics, complicating approximately 5% to 10% of term pregnancies and up to 30% of preterm deliveries. Although the etiology of premature rupture of the membranes is often not clinically evident, a degree of consensus has arisen regarding management options. Considerations in selecting management in a particular patient are gestational age and patient demographics. The clinician is confronted by a complex set of diagnostic and management options including use of amniocentesis, ultrasound, and biophysical testing and corticosteroids, tocolytics, and antibiotics. Of major importance in deciding on the management is the marked improvement in survival of low-birth-weight infants.
DEFINITIONS
PROM is usually defined as rupture at any time before the onset of contractions. Because “premature” also carries the connotation of preterm pregnancy, we use the word preterm to refer to gestational age of less than 37 weeks to avoid confusion. Thus, preterm PROM (PPROM) refers to PROM prior to 37 weeks’ gestation. The latent period is defined as the time from membrane rupture to onset of contractions. It is to be distinguished from latent phase designating the early phase of labor before the active phase. Various terms have been used to describe presumed maternal or perinatal infections related to PROM. During labor, designations have included “fever in labor,” “intrapartum fever,” “chorioamnionitis,” “amnionitis,” “intraamniotic infection” and “intrauterine infection.” The degree of temperature used to define “fever” has varied. After delivery, maternal infection is referred to as “endometritis” or “postpartum infection.” These diagnoses are usually based on fever, uterine tenderness, and exclusion of other sources of fever. In neonates, the most common term used to report infection was neonatal sepsis, but this may mean strictly a positive blood culture or simply clinical signs or symptoms of sepsis.
INCIDENCE
The incidence of PROM ranges about 5% to 10% of all deliveries, and preterm PROM occurs in approximately 1% of all pregnancies. Approximately 70% of cases of PROM occur in pregnancies at term, but in referral centers, more than 50% of cases may occur in preterm pregnancies. PROM is the clinically recognized precipitating cause of about one third of all preterm births. Despite some progress in prolonging the latent period after preterm PROM and possible prevention of recurrence (such as by use of progesterone or by treating bacterial vaginosis), PPROM remains a leading contributor to the overall problem of premature birth.
ETIOLOGY
In the vast majority of cases, the etiology is not clinically evident. With term PROM, the cause may be physiologic weakening of the membranes. Clinical conditions such as cervical incompetence and polyhydramnios have been identified as risk factors evident in some cases of PROM.
A scholarly review of the etiology of PPROM identified numerous potential causes in any given case. These included: a generalized decrease in tensile strength of membranes, local defects in the membranes, decreased amniotic fluid collagen and a change in collagen structure, uterine irritability, apoptosis, collagen degradation, and membrane stretch. The Maternal-Fetal Medicine (MFM) Network found that risk factors for PPROM were previous PPROM, positive fetal fibronectin at 23 weeks, and short cervix (<25 mm) at 23 weeks.
Substantial evidence is available to show that subclinical infection may be a cause of PROM, not merely its result. Support for a role of infection is provided by studies showing an association between clinically diagnosed bacterial vaginosis and preterm birth/preterm premature rupture of the membranes. Some genital bacteria elaborate enzymes such as proteases, phospholipases, and collagenases that may act to weaken the membranes. When amniotic fluid is obtained by amniocentesis in cases of PPROM, positive cultures are found in approximately 30% if the specimen is properly handled for aerobes, anaerobes, and genital mycoplasmas.
In a large case-control study, three factors were associated with preterm PROM in a multifactorial analysis. These were previous preterm delivery (odds ratio [OR] = 2.5; 95% confidence interval [CI] = 1.4−2.5), cigarette smoking (stopped during pregnancy: OR = 1.6; 95% CI = 0.8−3.3; continued during pregnancy, OR = 2.1; 95% CI = 1.4−3.1), and bleeding (first trimester: OR = 2.4; 95% CI = 1.5−3.9; third trimester, OR = 6.5; 95% CI = 1.9−23; more than one trimester, OR = 7.4; 95% CI = 2.2−26). This study enrolled controls at the same gestational age as cases (thus correcting for the decreasing frequency of coitus closer to term) and found no association between coitus and PROM. Recent coitus is probably not a cause of PROM.
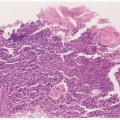
Investigations into the placental histology have provided correlates with clinical outcomes in cases of preterm premature rupture of the membranes. Overall, acute inflammation was seen in 43%, vascular lesions were seen in 20%, inflammation plus vascular lesions in 20%, normal findings in 14%, and “other” findings in 3% (Fig. 16.1). When acute inflammation was seen in the placenta (either by itself or mixed with vascular lesions), birth less than 26 weeks was more common, and delivery for suspected or proved clinical infection was also more common.
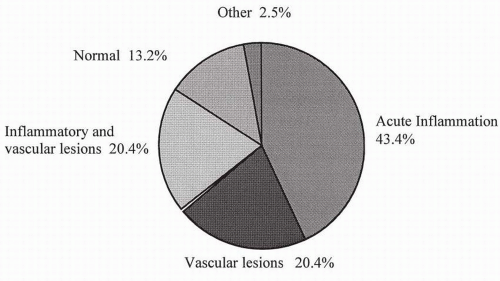 FIGURE 16.1 Placental histology in 235 cases of premature PROM. ((See Arias F, Victoria A, Cho K, et al. Placental histology and clinical characteristics of patients with preterm premature rupture of membranes. Obstet Gynecol 1997;89:265-271.) |
COMPLICATIONS AND CONSEQUENCES OF PROM
Onset of Labor
At term, the onset of labor occurs within 24 hours after membrane rupture in 80% to 90% of patients. Among patients with PROM prior to term, latent periods occur longer; latent periods of more than 24 hours occur in 60% to 80%, of more than 72 hours in about 15% to 25%, and of 7 days or more in 20% to 40%. There is an inverse relationship between gestational age and the proportion of patients with latent periods longer than 3 days. For pregnancies between 25 and 32 weeks, 33% had latent periods longer than 3 days, whereas for pregnancies of 33 to 34 and 35 to 36 weeks, the corresponding values were 16% and 4.5%, respectively.
Effect of Tocolytic Drugs
The value of tocolytics in PPROM remains controversial. None of eight prospective trials showed a decrease in neonatal morbidity, whether tocolysis was used prophylactically (for all patients in admission regardless of uterine activity) or therapeutically (for patients who developed uterine contractions). Only three of the eight showed a prolongation of the latency period; an additional study showed a prolongation for gestation less than 28 weeks. In three of these studies steroids were used; in another three studies antibiotics were used.
A comparison of short-term versus long-term tocolysis in preterm PROM at 26 to 35 weeks showed an adverse effect of “long-term tocolysis.” Patients with preterm PROM at 26 to 35 weeks were randomized to receive either an intravenous _-mimetic drug for less than 48 hours versus until delivery. All patients received corticosteroids, and group B streptococci (GBS) and gonococci were treated. There was no significant difference in the latent period or in neonatal infection, but there was a significant increase in both chorioamnionitis and endometritis with long-term tocolysis. Accordingly, use of tocolytics in patients with preterm PROM remains controversial, but the bulk of the evidence shows no benefit. However, if tocolytics are used, such as during transfer to a tertiary care center or obtaining benefits of corticosteroids, the course of tocolytics should be limited to less than 48 hours.
Respiratory Distress Syndrome, Infections, and Other Complications
The risks of PROM have generally been viewed as those of infection versus those of prematurity. The most common clinically evident complication among pregnancies with PROM before 37 weeks is respiratory distress syndrome (RDS), which, in general, is found in 10% to 40% of neonates. Bona fide neonatal sepsis is documented in less than 10%, and amnionitis (based on clinical criteria) occurs in approximately 3% to 30%. Subclinical infection, based on positive amniotic fluid culture or histologic inflammation of the cord or membranes, is seen much more often, in up to 80% at very early gestational ages with PPROM. Endometritis develops in up to 30%. Abruption after PROM is reported in 4.0% to 6.0% of cases, severalfold higher than the rate of 0.5% to 1.0% in the general population. Pulmonary hypoplasia is a serious fetal complication occurring in preterm PROM. Pulmonary hypoplasia is more common when there is very early preterm PROM, especially when this occurs in the presence of prolonged PROM and with severe oligohydramnios. There is nearly a 100% probability of lethal pulmonary hypoplasia when PROM occurs before 23 weeks and when there is severe oligohydramnios. With later gestational age at the onset of preterm PROM, the likelihood of pulmonary hypoplasia decreases. Notably with preterm PROM more than 24 to 26 weeks, even with oligohydramnios, pulmonary hypoplasia is rare. When preterm PROM occurs less than 25 weeks with severe oligohydramnios lasting more than 14 days, the likelihood of lethal pulmonary hypoplasia is estimated to be 80%. At the other extreme, when preterm PROM occurs at more than 25 weeks and when there is either no severe oligohydramnios or severe oligohydramnios for less than 5 days, then the predicted probability of lethal pulmonary hypoplasia is only 2%. These data provide important information for counseling patients with mid-trimester PROM.
RECURRENCE
The reported recurrence rate for PPROM is up to 32% for patients who had PPROM in an index pregnancy. Based on these data, the risk of recurrence is considerable, prompting patient education and close follow-up in subsequent pregnancies. Progesterone therapy appears to be effective in reducing the risk of recurrent preterm birth caused by PROM or preterm labor. Some studies have shown a decrease in recurrent preterm births caused by PROM by treating bacterial vaginosis.
EVALUATION
Diagnosis
The initial evaluation is likely to reveal amniotic fluid egressing from the vagina. The differential diagnosis of rupture of membranes includes loss of mucus plug, vaginal discharge associated with infection, and urinary loss. If the patient is not going to be delivered immediately, then a digital examination should be deferred as examination may introduce bacteria into the uterus and shorten the latent phase. A sterile speculum exam may demonstrate pooling of fluid in the posterior vaginal vault. Direct observation of fluid leaking from the cervical os confirms ruptured membranes. The normal pH of the vagina is between 4.0 and 4.7 in pregnancy, whereas the pH of the amniotic fluid is 7.1 to 7.3. Nitrazine paper changes to a dark blue from yellow with a pH above 6.5. Nitrazine paper to diagnose amniotic fluid in the vagina has an overall accuracy of approximately 93%, but false-positive results can result from blood, semen, alkaline urine, bacterial vaginosis, and trichomoniasis.
The diagnosis of PROM may also be confirmed by observing arborization or “ferning” of dried amniotic fluid on a slide. This method has an overall accuracy of diagnosis of PROM of approximately 96%. False positives occur with contamination by semen or cervical mucus. False negatives can result from a dry swab, contamination with blood at a 1:1 dilution, or not allowing sufficient time for the fluid to dry on the slide. Amniotic fluid arborization is unaffected by meconium at any concentration and is unaffected by pH alteration.
Ultrasound examination has been used widely, since oligohydramnios suggests PROM, but there have been no evaluations of its sensitivity and specificity. A multicenter clinical trial compared fetal fibronectin detection with standard tests for detection of rupture of membranes at term. Fetal fibronectin showed an excellent sensitivity (98.2%) but a low specificity, leading to speculation that fetal fibronectin in cervicovaginal secretions may be a marker for impending labor, even without frank rupture of the membranes. An immunoassay for placenta alpha microglobulin 1 (abundant in amniotic fluid, but barely detectable in normal cervicovaginal secretions) has been approved for detecting PROM. Initial reports have found a high diagnostic accuracy.
When the diagnosis of ruptured membranes is unclear by these tests, a transabdominal dye injection is sometimes performed. Indigo carmine blue (1 mL diluted in 9 mL of sterile normal saline solution) is injected into the amniotic fluid, and a sponge is placed into the vagina and inspected 30 minutes later for the dye. Methylene blue should not be used because of reported methemoglobinemia in the fetus. This test is invasive, and the accuracy of diagnosis is not established.
TABLE 16.1 ▪ MARKERS OF INTRA-AMNIOTIC INFECTION IN 110 PATIENTS WITH PPROM | ||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||
Fetal Maturity
Determination of the fetal age and maturity status is useful in developing a treatment plan. The patient’s history and early milestones of the pregnancy should be used. Ultrasound examination of the fetus can be limited because of the decreased fluid surrounding the fetus, and some measurements, especially of the abdomen and head, may be altered with oligohydramnios after PROM. As part of the overall decision process as to delivery, assessment of fetal lung status may be incorporated, for example, if gestational age is 32 to 34 weeks or if there is uncertainty regarding gestational age because of possible growth restriction. Amniotic fluid may be collected by amniocentesis or by collection from the vaginal pool. Vaginal pool collection is less accurate for lecithin/sphingomyelin (L/S) ratio determination. Whereas phosphatidylglycerol (PG) production by vaginal bacteria has been described, there has been an excellent correlation between PG detection in amniotic fluid obtained vaginally and transabdominally.
Cervical Status
In addition to documentation of ruptured membranes, the sterile speculum exam can evaluate the degree of cervical dilation and can exclude the possibility of a fetal extremity or umbilical cord prolapsing through the cervix. Endovaginal ultrasound may be used safely in patients with preterm PROM as it does not increase the risk of infection.
Infection
When the diagnosis of PROM is made, a rectovaginal culture should be taken for GBS unless the GBS status is already known. Appropriate antibiotics (usually i.v. penicillin G) for prevention of GBS infection should be given pending culture results (see Chapter 1).
All patients with preterm PROM should be evaluated for possible evidence of chorioamnionitis. Physical exam includes maternal or fetal tachycardia, uterine tenderness, and detection of a purulent, foul-smelling discharge. Temperature elevation is often a late sign of chorioamnionitis, especially in preterm PROM. In Table 16.1, we show the positive and negative predictive values of several tests for intrauterine
infection in PPROM. Most of these tests have modest performance characteristics, thus limiting their clinical utility. Amniocentesis may be performed to evaluate for an intrauterine infection, for example, if there are suggestive clinical signs of infection. Because of the high likelihood of subclinical infection and the association of intrauterine infection with cerebral palsy, there is a growing enthusiasm for early detection of subclinical infection. Accordingly, amniocentesis may become more widely used. Analyses of amniotic fluid for possible infection include Gram stain, glucose concentration, and culture. Gram stain does not identify colonization with genital mycoplasmas. A low amniotic fluid glucose predicts a positive amniotic fluid culture. When the glucose is greater than 20 mg per dL, the likelihood of a positive culture is less than 5%; when glucose is less than 5 mg per dL, the likelihood of a positive culture approaches 90%. Although not widely available, an elevated interleukin 6 (IL-6) in amniotic fluid may be the most sensitive predictor of intrauterine infection. A biophysical profile of 6 or less has been shown in several studies to correlate with intrauterine infection. Most newborns who are delivered after clinical chorioamnionitis do not show clinical infection, possibly because of common use of empiric antibiotic therapy.
infection in PPROM. Most of these tests have modest performance characteristics, thus limiting their clinical utility. Amniocentesis may be performed to evaluate for an intrauterine infection, for example, if there are suggestive clinical signs of infection. Because of the high likelihood of subclinical infection and the association of intrauterine infection with cerebral palsy, there is a growing enthusiasm for early detection of subclinical infection. Accordingly, amniocentesis may become more widely used. Analyses of amniotic fluid for possible infection include Gram stain, glucose concentration, and culture. Gram stain does not identify colonization with genital mycoplasmas. A low amniotic fluid glucose predicts a positive amniotic fluid culture. When the glucose is greater than 20 mg per dL, the likelihood of a positive culture is less than 5%; when glucose is less than 5 mg per dL, the likelihood of a positive culture approaches 90%. Although not widely available, an elevated interleukin 6 (IL-6) in amniotic fluid may be the most sensitive predictor of intrauterine infection. A biophysical profile of 6 or less has been shown in several studies to correlate with intrauterine infection. Most newborns who are delivered after clinical chorioamnionitis do not show clinical infection, possibly because of common use of empiric antibiotic therapy.
TREATMENT CONSIDERATIONS
The overall approach to management of PROM takes into consideration neonatal survival at the gestational age when rupture occurs. Management may be divided into four different phases of pregnancy. During the second trimester, neonatal survival is nil, leading numerous specialists to adopt a policy of expectant management or induction. Early in the third trimester, neonatal survival rises markedly, but there is still considerable morbidity associated with delivery at this gestational age. In the mid-third trimester, neonatal survival is high, but there is still considerable morbidity, whereas in the late third trimester (at or near term) neonatal mortality and morbidity are low. Neonatal outcome is one of the driving features in determining clinical management. Leakage of amniotic fluid into the lower genital tract occurs not uncommonly after amniocentesis, but in the vast majority of cases, membranes reseal and the outcome is good.
Diagnosis of Infection after PROM
Both invasive and noninvasive tests have been assessed. As shown in Table 16.1, none of these tests is ideal, particularly because of their modest positive predictive values.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree