3 Practical Application of Chinese Dietetics A General Applications of Chinese Dietetics B Specific Applications of Chinese Dietetics for Specific Conditions Nutrition has played an important role in China’s traditional medical system for many centuries and continues to do so. Chinese physicians have always regarded food as medicine. Eating a balanced diet was how the body was kept in harmony. Changing weather conditions throughout the year were taken into account by adjusting the diet accordingly and choosing the appropriate ingredients. Today, nutrition is still firmly rooted in public awareness in China and is regarded as an essential element in achieving a long and fulfilled life. The Chinese diet is a preventive diet. External climate factors determine daily food choices. In times of extreme cold, dishes using acrid spices provide increased nourishment for the body. In winter, the emphasis is on warming and hot dishes, while in times of extreme external heat, the body is calmed with cooling dishes. Such a preventive diet can be practiced in other parts of the world and can be followed by most people. It requires no special expertise other than a general understanding of Chinese nutritional principles. Healing diets that address imbalance, however, require a clear diagnosis and development of a therapy strategy by a professional TCM practitioner. In essence, diet influences all functions and processes in the body. A few other proven indications for Chinese nutrition should also be mentioned here: Chinese nutrition has nothing to do with rigid diets or instructions that have to be followed dogmatically. On the contrary, enjoyment involving all the senses is a vital part of any diet. Nor does it mean that from now on all one’s meals have to be eaten with chopsticks, or that the fridge has to be stocked with bamboo sprouts, Chinese (napa) cabbage, and tofu. The principles of Chinese nutrition can be applied to any cuisine or cooking style. The only knowledge that is required is an understanding of the thermal and energetic principles of foods, spices, and cooking methods, and an awareness of the adjustments to be made for seasons, climate effects, physical constitution, and individual sensitivities. Basic knowledge of Chinese nutrition enables anyone to manage their health by choosing the right foods and developing healthy eating habits. This primarily requires a knowledge of the thermal nature of foods (see the tables at the back of this book, p. 220) to respond appropriately to seasonal changes, climate factors such as cold, dampness, and summer heat, or extreme physical or emotional strain. However, people new to TCM, even when in good health, quickly start asking questions about their own constitution, individual food choices, different interactions, dietary habits, etc. People interested in prevention through diet can benefit from consulting a qualified TCM practitioner who can give specific advice. The confidence a practitioner can instill for the individualized application of Chinese nutrition at home makes such a consultation a worthwhile investment. Important: Nutritional therapy designed to heal illness must always be based on an informed diagnosis by a qualified TCM practitioner. Therapy must consider both the possibilities and the limitations of nutritional healing. Dietary therapy is commonly used in conjunction with other methods of Chinese medicine. Experienced TCM practitioners can also achieve excellent results by combining TCM with the diagnosis and therapy of Western medicine and naturopathy—all to the patient’s advantage. When prescribing a preventive diet, acknowledge your patients’ individual preferences to achieve the greatest possible compliance. In cases where a healing diet is appropriate, a patient’s distinct preferences can provide valuable therapeutic clues to patterns of disharmony. A patient’s constitution should be at the center of any decisions made about dietary prescriptions. Dietary recommendations always need to be adapted to the seasons and bioclimatic factors. Chinese nutrition requires more time than other treatments and thus a little patience. Let your patients know that tangible results might not be felt or seen for weeks or months, but that, once achieved, these results can last a lifetime. Inform your patients that dietary therapy is a great opportunity for developing healthy and beneficial eating habits that will keep them in good health for years to come. Suggestions for giving dietary advice – An individual diet plan with a list of all foods that are appropriate for the patient; – General basic information about energetic principles, healthy eating habits, different cooking methods, supplementing the center burner, etc. – Copies of recipes for specific preparations, such as the Master Soup, congees, medicinal wines (see p. 33, 117, 160). This makes your own work easier, takes less time, and enables patients to explore the information at their own pace at home. The main application for Chinese nutrition is prevention and general healthy living. Mild states of disharmony that are common in everyday life, for example those caused by bioclimatic factors such as cold or heat, or brought on by times of stress, can be balanced with appropriate preparation and choice of foods. Choosing foods in accordance and harmony with the seasons protects the body against disorders and helps it to live in tune with natural rhythms. Example During the cold seasons (fall and winter in the Northern hemisphere), one should increase the intake of warm or hot foods with pronounced yang character. Fruits and salads—foods that are mostly yin—are not recommended during the colder months, because they cool down the energetics of the body even further, instead of warming it and protecting it from external cold. Therapy always first requires a diagnosis based on the principles of TCM. The appropriate choice of foods provides a foundation for further treatment methods such as acupuncture and herbal therapy. Dietary therapy adjusted to the individual’s symptoms creates a good basis for additional treatments, resulting in quicker and more effective improvement. Chinese practitioners find it hard to understand why most doctors in the Western world utilize only one treatment at a time, for example acupuncture, instead of making full use of all treatments available and coming up with a comprehensive treatment strategy. In traditional Chinese hospitals, a patient’s individual diet plan is part of a holistic treatment concept. Example The treatment of insomnia, which aims to drain yang, will not prove successful through acupuncture alone if patients continue to stimulate their yang by consuming warm or hot foods. Examples are coffee, hot spices, garlic, onions, and lamb. By ignoring dietary recommendations, the patient essentially works against the acupuncture treatment rather than with it. Abstaining from foods containing yang and giving preference to yin foods, on the other hand, supports the acupuncture treatment and promotes success. Qi vacuity can appear in any of the networks. The most common causes for general qi vacuity are vacuity of spleen qi, kidney qi, and lung qi. Symptoms Fatigue, exhaustion, lack of appetite, lack of concentration, abdominal bloating; soft, sloppy stool; tendency to diarrhea, tendency to feel cold and to shiver, aversion to cold, lowered resistance, frequent backaches in the lumbar vertebral column, frequent urination with clear urine, large amounts of urine, nocturia (excessive night time urination), dyspnea (shortness of breath), premature ejaculation, reduced sexual desire, impotence.
A General Applications of Chinese Dietetics
Practical Guidelines for Giving Nutritional Advice
The Role of Chinese Nutrition in Traditional Chinese Medicine (TCM)
General Indications for Chinese Dietetics
 Daily general regeneration and balancing of qi, blood (xue), body fluids (jin ye), and spirit (shen).
Daily general regeneration and balancing of qi, blood (xue), body fluids (jin ye), and spirit (shen).
 Specific supplementation of qi, yang, yin, and especially blood (xue) and body fluids (jin ye).
Specific supplementation of qi, yang, yin, and especially blood (xue) and body fluids (jin ye).
 Stabilizing, invigorating, or calming the spirit (shen).
Stabilizing, invigorating, or calming the spirit (shen).
 Preserving essence (jing) with high-quality foods and regular eating habits.
Preserving essence (jing) with high-quality foods and regular eating habits.
 Supplementing and balancing the organ networks and the bowels and viscera (zang fu organs).
Supplementing and balancing the organ networks and the bowels and viscera (zang fu organs).
 Supplementing, regenerating, and moving defense qi (wei qi).
Supplementing, regenerating, and moving defense qi (wei qi).
 Supplementing and balancing the spleen/pancreas and stomach organ networks.
Supplementing and balancing the spleen/pancreas and stomach organ networks.
 Balancing disturbing effects brought on by weather or other external factors.
Balancing disturbing effects brought on by weather or other external factors.
 Harmonizing the body with the seasons.
Harmonizing the body with the seasons.
 Supplementing the center burner in children.
Supplementing the center burner in children.
 Treating patterns of disharmony in children.
Treating patterns of disharmony in children.
 Prevention during pregnancy by strengthening qi, particularly blood (xue) and body fluids (jin ye).
Prevention during pregnancy by strengthening qi, particularly blood (xue) and body fluids (jin ye).
 General regeneration after childbirth, especially in cases of exhaustion.
General regeneration after childbirth, especially in cases of exhaustion.
 Specific treatment of constitutional disorders.
Specific treatment of constitutional disorders.
 Treating disorders caused by dampness and phlegm.
Treating disorders caused by dampness and phlegm.
Don’t Worry about Dogmatism
Tips for Giving Nutritional Advice
 The following tips help you achieve compliance in your patients, which is so crucial to the success of dietary advice!
The following tips help you achieve compliance in your patients, which is so crucial to the success of dietary advice!
 To give competent and professional dietary advice, you should have a sound knowledge of the principles of Chinese nutrition (both preventive and healing diets) and should be trained in TCM diagnosis.
To give competent and professional dietary advice, you should have a sound knowledge of the principles of Chinese nutrition (both preventive and healing diets) and should be trained in TCM diagnosis.
 During the initial consultation, you can assess your patient’s constitution by paying attention to certain criteria and then deepen your observations by asking your patient specific questions.
During the initial consultation, you can assess your patient’s constitution by paying attention to certain criteria and then deepen your observations by asking your patient specific questions.
 Let your patients tell you about their eating habits, food preferences, etc.
Let your patients tell you about their eating habits, food preferences, etc.
 Ask your patients about their digestion.
Ask your patients about their digestion.
 Communicate the results of your observations to your patients and explain in detail the diet plan that will accompany them in the following weeks.
Communicate the results of your observations to your patients and explain in detail the diet plan that will accompany them in the following weeks.
 Clearly mark all foods that are good for the patient with a “+,” and foods that are bad for the patient with a “–”;
Clearly mark all foods that are good for the patient with a “+,” and foods that are bad for the patient with a “–”;
 Make recommendations about eating habits and food preparation (tailored to the diagnosis) during the initial consultation.
Make recommendations about eating habits and food preparation (tailored to the diagnosis) during the initial consultation.
 Provide your patient with written information. This includes:
Provide your patient with written information. This includes:
 Length of initial consultation: between 20 and 100 minutes.
Length of initial consultation: between 20 and 100 minutes.
 Arrange a second appointment three to six weeks later.
Arrange a second appointment three to six weeks later.
 Possible follow-up questions can be answered over the phone (have a phone consultation schedule).
Possible follow-up questions can be answered over the phone (have a phone consultation schedule).
 During the second consultation, answer any questions and clear up any uncertainties. Have the patient describe any noticeable successes or results.
During the second consultation, answer any questions and clear up any uncertainties. Have the patient describe any noticeable successes or results.
General Nutritional Recommendations (for sharing with patients)
 Please take the following to heart:
Please take the following to heart:
 Use high-quality, clean, and unprocessed foods, organically grown whenever possible.
Use high-quality, clean, and unprocessed foods, organically grown whenever possible.
 Create a pleasant, relaxed atmosphere in which you can enjoy your meals.
Create a pleasant, relaxed atmosphere in which you can enjoy your meals.
 Eat with pleasure.
Eat with pleasure.
 Eat regularly, between three to five times a day.
Eat regularly, between three to five times a day.
 Do not rush your meals and chew each bite well (between 10 and 15 times)!
Do not rush your meals and chew each bite well (between 10 and 15 times)!
 Eat breakfast like a king, lunch like an emperor, and dinner like a beggar.
Eat breakfast like a king, lunch like an emperor, and dinner like a beggar.
 Stop eating when it tastes best!
Stop eating when it tastes best!
 Drink only small amounts of liquids during meals; too much liquid with meals, or right before and right after a meal can weaken your digestive fire.
Drink only small amounts of liquids during meals; too much liquid with meals, or right before and right after a meal can weaken your digestive fire.
 When putting together a meal, take into account your individual constitution.
When putting together a meal, take into account your individual constitution.
 Choose foods that are appropriate for the season (choosing locally grown foods that are in season is often a good way).
Choose foods that are appropriate for the season (choosing locally grown foods that are in season is often a good way).
 When following a vegetarian diet, ensure your diet contains enough energetically warming foods; increase the use of acrid spices in cold weather.
When following a vegetarian diet, ensure your diet contains enough energetically warming foods; increase the use of acrid spices in cold weather.
 Please avoid the following:
Please avoid the following:
 Too much raw or cold food and tropical fruits: These are energetically too cool, reduce the energy of the center burner, and if consumed, regularly, can cool the kidney organ network.
Too much raw or cold food and tropical fruits: These are energetically too cool, reduce the energy of the center burner, and if consumed, regularly, can cool the kidney organ network.
 Ice-cold beverages: They block stomach and spleen/pancreas qi flow and weaken spleen qi and spleen yang.
Ice-cold beverages: They block stomach and spleen/pancreas qi flow and weaken spleen qi and spleen yang.
 Too much dairy: Dairy products are energetically too cool. They weaken the spleen/pancreas network and cause dampness and phlegm.
Too much dairy: Dairy products are energetically too cool. They weaken the spleen/pancreas network and cause dampness and phlegm.
 Exhausting discussions or other distractions during a meal (TV, radio, reading): They can block the flow of qi in the center burner and cause food stagnation.
Exhausting discussions or other distractions during a meal (TV, radio, reading): They can block the flow of qi in the center burner and cause food stagnation.
 Too much oily, fatty food: Blocks the flow of qi and causes heat, dampness, and phlegm.
Too much oily, fatty food: Blocks the flow of qi and causes heat, dampness, and phlegm.
 Too much sugar, sweet flavors: Causes heat, dampness and phlegm.
Too much sugar, sweet flavors: Causes heat, dampness and phlegm.
 Too much alcohol: Causes damp heat, promotes formation of phlegm and hurts jing, along with a number of other unpleasant effects.
Too much alcohol: Causes damp heat, promotes formation of phlegm and hurts jing, along with a number of other unpleasant effects.
 Too much meat: Causes dampness and phlegm.
Too much meat: Causes dampness and phlegm.
 Late evening meals: Block the flow of qi, cause food obstruction, weaken the spleen/pancreas network, and lead to weight gain.
Late evening meals: Block the flow of qi, cause food obstruction, weaken the spleen/pancreas network, and lead to weight gain.
 Overly opulent meals: Block flow of qi, cause food stagnation, burden the spleen/pancreas network, cause dampness and phlegm and lead to weight gain.
Overly opulent meals: Block flow of qi, cause food stagnation, burden the spleen/pancreas network, cause dampness and phlegm and lead to weight gain.
 Excessive and prolonged fasting: Weakens the center burner, as well as yin, blood (xue), and jing.
Excessive and prolonged fasting: Weakens the center burner, as well as yin, blood (xue), and jing.
Application Areas
Application Goal: Prevention
Application Goal: Therapy
General Qi Vacuity
Tongue: | Pale, swollen |
Pulse: | Vacuous, weak |
Causes
General: | Stress, overexertion, lack of sleep, too many negative emotions such as worries, anxiety, fear, brooding; too much sexual activity; in women, too many births spaced too closely; external cold; chronic illnesses. |
Diet: | Too much thermally cold food, yin products, or raw foods; irregular eating habits; too much dairy; too many tropical fruits, frozen foods, denaturalized foods, canned foods, or ice-cold beverages; hasty eating; eating too late in the day. |
Prevention
 Nutritional Therapy
Nutritional Therapy
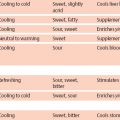
Thermal nature | Neutral, warming, sometimes hot |
Cooking method | Warming |
Flavor | Neutral–sweet, warm–sweet, neutral–acrid, warm–acrid, neutral–salty, warm–salty, occasionally also hot |
Grains | Oats, millet, corn, rice, short-grain (sweet, glutinous) rice, spelt |
Meat | Poultry, lamb, beef, game (venison) |
Fish | Oysters, trout, lobster, salmon, anchovies |
Vegetables | Fennel, carrots, leeks, chestnuts |
Spices | Acrid and hot, ginger, garlic, coriander |
Nuts and seeds | Hazelnuts, black sesame, walnuts |
Legumes | Lentils |
Tip: Have a substantial, warming breakfast, for example warm millet porridge or oatmeal, and at least one or two warm meals daily, for example Master Soup, stews.
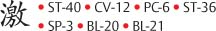
Supplement spleen qi
Supplement kidney qi
General Yang Vacuity
Yang vacuity can present similar symptoms as qi vacuity, because yang vacuity is always preceded by protracted qi vacuity and the transition between the two is not clearly delineated.
Symptoms
Primarily cold symptoms, such as cold, pale extremities, general weakness, severe mental and physical exhaustion, lack of drive, general loss of strength, as well as water retention in form of edemas. Women can encounter menstrual disorders, missed periods, and diarrhea.
Tongue: | Pale, swollen, with tooth impressions |
Pulse: | Vacuous, weak |
Prevention
 Basically the same as for qi vacuity. However, more foods with strong yang character can be used.
Basically the same as for qi vacuity. However, more foods with strong yang character can be used.
Cooking method | Warming, grilled, fried |
Meat | Beef, poultry, lamb, game (especially venison) |
Also | Fennel, walnuts, chestnuts, corn, raisins, cherries, peaches, leeks, acrid spices |
| Master Soup and stews with warming meat and vegetables. |
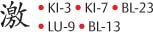
Supplement kidney yang
Supplement spleenyang
General Yin Vacuity
Yin vacuity is a deeper disorder of the body and can affect each of the organ networks. Syndromes seen frequently in practice are yin vacuity of the liver, heart, lung, and kidney networks. Yin vacuity can damage the substance of the organ network involved.
Symptoms
Thirst, dry mouth, hot soles of the feet, especially at night, possibly hot hands, burning sensation behind the chest bone, night sweat, possibly weight loss. Symptoms that occur due to pseudo-yang as a result of yin vacuity: Restlessness, agitation, nervousness, sleep disorders, dizziness, internal heat sensation; dry, hard stool; easily startled, emotional instability, susceptibility to stress, lack of resiliency.
Tongue: | Red, chapped |
Pulse: | Rapid, thin. |
Causes
General causes: Long chronic illnesses, depletion of body fluids, for example due to extreme fever; protracted blood loss; excessive sexual activity; excessive drug use or medication abuse; extreme emotional strain such as worry, grief, fear; overexertion and overwork; sleep deprivation due to nighttime work; hectic and stressful lifestyle that creates internal heat and exhausts body fluids.
Dietary causes: Excessive intake of extremely warming foods, especially acrid spices that dry out the body fluids and hurt the yin. Additional factors are excessive intake of coffee, high-proof alcoholic beverages, poor and irregular diet.
Prevention
 Nutritional Therapy
Nutritional Therapy
 Avoid:
Avoid:
Heat; foods with yang characteristics; the flavors hot–bitter, warm–bitter, hot–acrid, warm– acrid; hot and warm foods or beverages, especially coffee, black tea, red wine; garlic, ginger, acrid spices; high-proof alcohol.
Yin foods with neutral–sweet and refreshing– sweet flavor.
Meat/fish | Pork, oysters |
Vegetables | Cooling, refreshing vegetables, spinach, tomatoes, seaweed |
Grains | Spelt, corn, rice, wheat |
Fruit | Apples, pears, blackberries, citrus fruit, strawberries, bananas, grapes |
Dairy products | Butter, cheese, yogurt, milk |
Soy products | Tofu, soy milk |
Beverages | Red fruit juices, citrus juices, wheat beer |
Replenish yin by supplementing spleen yin, kidney yin, and liver yin

Yin Repletion (Excess) and Dampness
Yin repletion is often caused by a poor, insufficient diet. Consuming too many yin products cools the body, harms spleen qi, and causes dampness. This syndrome can worsen due to a weak spleen and can, over time, lead to phlegm disorders. Yin repletion reduces the body’s yang energy.
 Symptoms
Symptoms
Lack of drive; fatigue; slowed movements and language; cold hands; feeling of heaviness inside the body, as well as in the arms and legs; dull headache which the patient often describes as a “feeling like I am wearing a helmet”; tendency to diarrhea, bloating, water retention in arms, legs, and face; a melancholic disposition, sometimes depression; obesity.
Causes
General causes: General factors that can cause spleen qi vacuity and general yang vacuity, such as overexertion, lack of sleep.
Dietary causes: Irregular intake of food; rushed meals eaten under stress; main meal in the late evening; too much raw food, salads and dairy products that produce too much dampness and phlegm.
Prevention
 Successfully dealing with the stresses and challenges of everyday life while staying healthy requires a healthy and supportive diet. Healthy eating habits should be developed to sustain the energy necessary for facing the demands of daily life and establishing a balanced state of health.
Successfully dealing with the stresses and challenges of everyday life while staying healthy requires a healthy and supportive diet. Healthy eating habits should be developed to sustain the energy necessary for facing the demands of daily life and establishing a balanced state of health.
 Avoid:
Avoid:
Yin foods; damp foods, especially dairy products; raw fruit and vegetables; excess sweet flavors; hasty, irregular meals; main meal in the late evening; inadequate breakfast; too much fat and oil.
 Recommended:
Recommended:
Moderately warming foods and cooking methods. For dampness and phlegm, especially bitter–warm flavors, but also sweet– warm, warm–salty, warm–refreshing, as well as all neutral flavors. Moderate intake of hot foods.
Also: | Ginger, cardamom, leeks, pears, cherries, carp, millet. |
For additional recommendations, see also “Strengthening the Inner Center,” page 42.
Yang Repletion (Excess) Conditions
Yang repletion displays different levels of intensity and is a commonly found pattern of disharmony in medical practice. It is important to differentiate real yang repletion from “pseudo-yang” repletion or “empty heat.” Real yang repletion is a short-term surplus of yang. “Pseudo-yang” repletion is the appearance of yang repletion symptoms caused by the absence of yin, which can lead to an increased appearance of yang character.
Draining yang can initially alleviate both patterns. If the cause is complete yin vacuity, as is the case with “pseudo-yang” repletion, yin needs to be replenished along with draining yang in order to establish lasting harmony.
 Symptoms
Symptoms
Red complexion, hyperactivity, restlessness, anxiety, loud voice, boisterous laugh, dominating personality, irritability, and tendency to outbursts of anger. Body feels hot, thirst, tendency to get headaches, dizziness, tinnitus (ringing in the ears), headache in the temporal region (shao yang headache due to upbearing liver yang), bitter taste in mouth (liver fire), excessive perspiration, high blood pressure, episodes of voracious appetite with a tendency to weight gain (stomach heat).
Causes
General causes: The majority of yang symptoms are caused by a relative yang surplus and result from a yin vacuity of the affected bowel (zang organ). Emotional strains such as stress, a hectic lifestyle, and suppressed emotions such as rage, anger, and frustration harm the organ network of heart and liver. The longer an emotional imbalance persists, the more the organs are impaired. The liver phase is especially sensitive and can suffer deep-seated damage from protracted stagnation of liver qi when qi flow is blocked due to suppressed emotions. This creates a precarious balance that can easily be upset by even minor yang effects such as stress or the wrong diet (high-proof alcohol, acrid spices), invoking symptoms of ascendant liver yang (gan yang shang kang) and liver fire (gan huo shang yan)
Dietary causes: Green tea, mineral water, wheat beer, tofu, mung beans, dandelion, Belgian endive hearts, peppermint tea, cow’s milk, yogurt, cheese, farmer’s cheese, cottage cheese, buttermilk. Patients often prefer acrid flavors to relax the body and loosen any existing emotional blockages, or excessively sweet flavors to counteract frustrations and grief. Acrid–warm flavors and acrid–hot flavors, like all thermally hot foods, can cause heat-related symptoms. Bitter–hot, as well as all other hot flavors can dry out body fluids and deplete the body’s yin. These heat symptoms often appear in combination with hot, viscous phlegm and frequently result from excessive consumption of very oily or fatty foods. The liver organ network is especially sensitive to heat and fatty, oily foods (junk food).
Prevention
 Nutritional Therapy
Nutritional Therapy
 Avoid:
Avoid:
All energetically hot foods and beverages, especially acrid spices such as curry, ginger, garlic, and pepper. Onions, high-proof alcohol, warming cooking methods like frying, grilling. Decrease consumption of thermally warm foods and meat (abstain from meat for four to six weeks, especially lamb, beef, poultry, pork). Decrease intake of coffee, red wine, and salt.
 Recommended:
Recommended:
Yin foods with neutral–sweet, cool–sweet, cold– sweet, neutral–sour, cool–sour, cold–sour flavor. Vegetables: Tomatoes, spinach, cucumbers, celery Grains: Wheat, barley Fruit: Apples, pears, citrus fruit, raspberries, gooseberries
Blood Vacuity (Xue Xu)
Blood vacuity is an important syndrome in Chinese pathophysiology and is very commonly found in practice. Blood vacuity is often at the root of many gynecological disorders. Men have more qi in their blood and thus tend to suffer more from qi problems.
General: | Pale skin, pale lips, sensation of dizziness inside head, dull complexion, numbness, fatigue, dry hair and skin. |
Liver blood vacuity (gan xue xu): | Blurred vision, sleep disorders, dry and brittle nails, muscle weakness, muscle cramps, sensation of “pins and needles” or falling asleep of the limbs, sensitivity of eyes to light, psychological, mental, and gynecological symptoms, lack of drive, nervousness, emotional frailty, low self-esteem, heart palpitations, menstrual disorders such as painful menstruation or absence of menstruation (dysmenorrhea or amenorrhea). |
Chronic blood vacuity symptoms are general dryness: Dry skin, dry hair, possibly hair loss, and brittle nails. Blood vacuity can create favorable conditions for liver wind, causing dry skin conditions accompanied by severe itching and blisters on alternating parts of the body.
Tongue: | Pale, small; dry tongue body |
Pulse: | Thin, fine or rough |
Pathogenesis
TCM believes that blood is primarily formed in the spleen. Blood vacuity can therefore be caused by spleen vacuity. Blood formed in the spleen with help from the lungs becomes “spirited” with qi and jing from the kidneys as it circulates. Not until then does blood from the spleen have the necessary energy. Good blood formation also requires balanced lung and kidney energy. The liver plays an important role as a storage organ for blood. This means that any blood vacuity eventually leads to liver disharmony with liver blood vacuity (gan xue xu). Particularly damaging to the blood is liver heat, which sets blood into restless motion. Protracted heat can dry out and damage blood (xue).
Therapy
Strengthen blood
Supplement spleen qi
Enrich liver blood
 Nutritional Therapy
Nutritional Therapy
 Avoid:
Avoid:
Warming cooking methods and thermally hot foods. All bitter foods, especially the flavors bitter–hot and bitter–warm. Acrid–hot and acrid– warm flavors, since these dry out blood. Black tea, hot chocolate, acrid spices such as garlic, ginger, pepper, curry, cinnamon, etc. Energetically hot drinks such as coffee, high-proof alcohol, yogi tea (chai).
 Recommended:
Recommended:
Cooking method | Cooling |
Flavor | Sweet–neutral, sweet–warm, sour–neutral, sour–cool |
Grains | Oats, amaranth, short-grain (glutinous) rice, rice |
Vegetables | All thermally neutral and refreshing vegetables like red beets, red cabbage, carrots, spinach, fennel |
Meat | Chicken, chicken liver, beef, beef stock, beef liver, veal liver, lamb liver (liver preferably from organically raised animals or aninmals living in the wild) |
Fish | Oysters, mussels, squid (octopus), perch, eel |
Fruits | Red grapes, sweet cherries, longans (a type of lychee), plums, apricots |
Nuts and seeds | Sesame, sunflower seeds |
Beverages | Red beet juice, sweet cherry juice, plum juice, red tea (e.g., rosehip tea, hibiscus), red grape juice, red wine in moderation |
Recommended for liver blood vacuity:
Meat | Chicken, duck, rabbit liver, hare liver, pork liver (liver preferably from organically raised or wild harvested animals) |
Fish | Oysters, shrimps, white fish, bass |
Fruit | Apples, lychees, plums, grapes, longans (similar to lychees) |
Vegetables | Thermally neutral and cooling, green vegetables of the wood phase: beans, broccoli, lamb’s lettuce (miner’s lettuce), lotus root, mangold chard (Swiss chard), spinach, sprouts, tomatoes |
Beverages | Carrot juice, tomato juice |
Grains | Wheat, short-grain (glutinous) rice |
Spices | Watercress, marjoram, parsley root |
Nuts and seeds | Sesame, sunflower seeds |
Other | Egg yolk |
Strengthening Defense Qi (Wei Qi)
Defense qi protects the body against disease. It circulates outside the body channels, mainly on the body’s surface. Defense qi ’s most important function is to provide protection against external pathogenic factors such as wind, cold, heat, and dampness. At the same time, it warms and moistens skin and muscles. Since it circulates below the skin’s surface, defense qi is primarily governed by the lungs. Defense qi prevents pathogens from entering the body by regulating the opening and closing of the skin’s pores. If lung energy is too weak, pores do not close in time, allowing pathogens to penetrate and cause disorders. Lung qi vacuity can result in lowered resistance, which in turn can lead to increased susceptibility to colds. While the lungs are responsible for the control and distribution of defense qi, the center burner also contributes to the production of defense qi, along with the stomach and spleen. If those two organs are in a state of vacuity, qi supply of the whole body is lowered, which then affects quantity and quality of defense qi. Original essence (prenatal) qi from the kidneys also plays a minor role in the production of defense qi.
In summary, there are three energy systems responsible for good defense:
First and foremost, lung qi for governing and distributing defense qi, stomach and spleen qi,aswell as for reproduction, quantity, and quality of defense qi. Secondly, original qi from the essence of liver yang. Thirdly, defense qi is a fleeting and active yang energy. With its role in the opening and closing of pores, it is closely associated with the secretion of body fluids (sweat). During the day, it circulates mostly in the surface yang channels of greater yang (tai yang) lesser yang (shao yang), and yang ming. At nighttime, it flows back into the bowels (zang organs) kidney, heart, lung, liver, and spleen.
Symptoms
General symptoms of qi or yang vacuity include: pale complexion; feeling cold, shivering and aversion to cold; cool and cold extremities; easily physically and emotionally fatigued; general listlessness; spontaneous perspiration (lung qi vacuity). During the acute phase of a cold: chills, a feeling of coldness along one’s back along the greater yang (tai yang) channel, joint pain; runny nose with liquid, clear secretion; sneezing, sensitive to cold, exhaustion (symptoms of a wind–cold attack on the body).
Causes
 Factors that weaken lung qi, for example constitutional weakness, extended periods of sitting in a slumped position (inhibits breathing and thus leads to lung qi vacuity). Smoking, damage to lung qi by external pathogenic factors such as wind–cold or wind–heat, overwork, prolonged grief.
Factors that weaken lung qi, for example constitutional weakness, extended periods of sitting in a slumped position (inhibits breathing and thus leads to lung qi vacuity). Smoking, damage to lung qi by external pathogenic factors such as wind–cold or wind–heat, overwork, prolonged grief.
 Factors that weaken spleen and stomach.
Factors that weaken spleen and stomach.
 Factors that weaken kidney yang and essence.
Factors that weaken kidney yang and essence.
Strengthen bodyyang
Supplement lungqi
Supplement center burner
Supplement kidneyyang
 Nutritional Therapy
Nutritional Therapy
 Avoid:
Avoid:
All foods that can weaken the yang of the body, for example foods with cool or cold thermal nature such as raw foods, salads, cold types of fruit, dairy products, cold beverages.
 During the acute phase of a common cold, avoid all foods that increase the formation of mucus to protect the weakened lung qi from possible phlegm disorders and to avoid straining the spleen (bananas, dairy products, raw foods, and very oily and fatty foods).
During the acute phase of a common cold, avoid all foods that increase the formation of mucus to protect the weakened lung qi from possible phlegm disorders and to avoid straining the spleen (bananas, dairy products, raw foods, and very oily and fatty foods).
 Recommended:
Recommended:
Acrid–warm and acrid–hot flavors that strengthen the metal phase to supplement and support defense qi.
During the acute beginning of a cold, avoid the sour flavor. In Chinese medicine, all citrus fruits are contraindicated for the duration of a cold. The reason is the direction of movement of the sour flavor. It moves inward and thus prevents the already weakened defense qi from coming to the surface and averting the penetrating pathogenic factors. This results in the pores of the skin being insufficiently closed, creating a relatively unobstructed path for entry of pathogenic factors through the skin. The sour flavor makes it possible for pathogenic factors located on the body surface to move into deeper layers. Thus, TCM believes hot lemon juice and large servings of citrus fruits such as oranges and lemons should not be consumed for the duration of a cold.
 In Chinese herbal therapy, huang qi (astragalus) is an important remedy for supplementing defense qi.
In Chinese herbal therapy, huang qi (astragalus) is an important remedy for supplementing defense qi.
 In the early stage of a cold, it is especially productive to treat the symptoms (cold and chills) with the strong yang energy of acrid–warm and acrid–hot flavors. This moves defense qi, opens the pores for a short time to allow the expulsion of pathogenic factors such as cold, dispels external pathogenic cold and wind, clears the body surface, and strengthens yang and defense qi in the body.
In the early stage of a cold, it is especially productive to treat the symptoms (cold and chills) with the strong yang energy of acrid–warm and acrid–hot flavors. This moves defense qi, opens the pores for a short time to allow the expulsion of pathogenic factors such as cold, dispels external pathogenic cold and wind, clears the body surface, and strengthens yang and defense qi in the body.
 Recommended:
Recommended:
Spices | Especially fresh ginger! Also pepper, chili, acrid spiced tea (e.g., yogi tea) |
| Decoction of fresh ginger with green (spring) onions: Simmer thumb-sized pieces of fresh ginger and green onions in 0.5 L (two cups) of water for about 10 minutes. Drink one to two cups of this liquid while warm. |
All foods with yang potential are recommended for strengthening defense qi. Sweet–warm or sweet– hot flavors are especially suitable for supplementing the center burner. Salty–hot and salty–warm flavors can strengthen the kidneys. The body is especially susceptible to pathogenic energy at night, since defense qi circulates deeper in the body during that time, leaving the surface unprotected. Too little sleep and too much nightly activity increase susceptibility to externally caused disorders.
Nutritional therapy can individually strengthen specific organs with certain foods. Aside from generally supplementing yang in the body via the three networks kidney, spleen/stomach, and lung, supplementing lung qi is especially advisable for strengthening the body’s defenses.
Supplementing Lung Qi
 Nutritional Therapy
Nutritional Therapy
Spices | Chili, curry, ginger, pepper |
Beverages | Spiced teas, high-proof alcohol |
Vegetables | Cauliflower, leeks, horseradish, onions, radish, watercress |
Nuts and seeds | Almonds, almond butter |
 Wind–cold disorder, which attacks the lung when there is insufficient defense qi to protect it, can develop into wind–heat, which is characterized by fever; thirst, a preference for cold beverages, headaches, sparse, dark urine, and physical exhaustion. These signs of a wind–heat attack with predominant heat symptoms require immediate adjustment of nutritional therapy. During this phase, acrid–hot and acrid–warm flavors, as well as foods with a hot thermal nature are contra-indicated; cooling foods are recommended. Sour flavors should be avoided to prevent the disorders from moving into deeper layers of the body.
Wind–cold disorder, which attacks the lung when there is insufficient defense qi to protect it, can develop into wind–heat, which is characterized by fever; thirst, a preference for cold beverages, headaches, sparse, dark urine, and physical exhaustion. These signs of a wind–heat attack with predominant heat symptoms require immediate adjustment of nutritional therapy. During this phase, acrid–hot and acrid–warm flavors, as well as foods with a hot thermal nature are contra-indicated; cooling foods are recommended. Sour flavors should be avoided to prevent the disorders from moving into deeper layers of the body.
Dampness and Phlegm Conditions
TCM views dampness and phlegm as important and common pathological factors in the treatment of many disorders.
The motto of traditional Chinese physicians was: “If you’ve treated a disorder for a long period of time without success, always remember phlegm.”
The Western observer associates phlegm disorders mainly with a stuffed up nose and sinuses, sinusitis frontalis, sinusitis maxillaris, and bronchial congestion. In TCM, these are only partial aspects, as the Chinese idea of phlegm disorders incorporates a lot more than just material phlegm: Phlegm can occur in all parts of the body. It slows down the flow of qi and congests the channels, inducing symptoms such as numbness, dull, “foggy” headache, sluggishness, and lack of concentration. A well-known and typical symptom of dampness in the head is the so-called hangover headache caused by too much alcohol resulting in the creation of phlegm.
Pathogenesis
Phlegm is created mainly by a disorder of the spleen/pancreas network. If the spleen is too weak, qi flow slows and transformation and transport of fluids becomes congested. As a result, dampness accumulates. With chronic spleen qi or yang vacuity, dampness collects over a longer period and creates concentrated accumulations of liquid. These eventually thicken into phlegm, especially if subjected to the effects of heat. Since spleen vacuity is always the primary cause of phlegm, therapy needs to focus on strengthening this particular bowel (zang organ)!
Also contributing to the formation of phlegm are the lungs and kidneys. The primary responsibility of the lungs is to distribute and reduce fluids produced by the spleen. If weakened, the lungs are unable to perform this task, resulting in the formation of dampness (swelling and edemas) and phlegm in the nasal and sinus cavities (maxillary sinus and frontal sinus). In the worst case, the lungs themselves become obstructed (bronchitis, pneumonia).
The kidneys, on the other hand, are responsible for the intake and discharge of liquids. If this function is impaired, liquids gather primarily in the lower burner and can lead to formation of edemas. As a rule, good kidney energy (kidney yang) is important for warming and supporting the spleen. Other causes for the formation of phlegm, especially heat phlegm (viscous, yellow phlegm) are external wind–heat disorders that damage the lung, for example acute bronchitis, sinusitis, and hay fever. Heat phlegm can also arise with liver qi stagnation, since heat is formed when the flow of qi is slowed and congested, and heat thickens fluids.
Phlegm Differentiation
 Substantial phlegm: Appears in the form of sputum with disorders of the respiratory system, for example rhinitis, sinusitis, bronchitis, or pneumonia.
Substantial phlegm: Appears in the form of sputum with disorders of the respiratory system, for example rhinitis, sinusitis, bronchitis, or pneumonia.
 Immaterial, “invisible” phlegm: Collects in the channels of the body and obstructs qi flow. Immaterial phlegm can gather subcutaneously and appear in the shape of skin nodules: Lipoma, adenoma, ganglia, or as a goiter. In its hardened form, phlegm turns into gallstones or kidney stones. Phlegm in the joints causes bone deformation or chronic rheumatoid arthritis. Even “plum pit qi” (the sensation of a foreign body in the throat, mei he qi), a condition known in TCM, is another form of phlegm (qi phlegm), triggered mainly by binding depression of liver qi due to emotional causes. Its symptoms can include difficulty swallowing, globus hystericus (“lump in the throat”), or a feeling of oppression in the chest and diaphragm.
Immaterial, “invisible” phlegm: Collects in the channels of the body and obstructs qi flow. Immaterial phlegm can gather subcutaneously and appear in the shape of skin nodules: Lipoma, adenoma, ganglia, or as a goiter. In its hardened form, phlegm turns into gallstones or kidney stones. Phlegm in the joints causes bone deformation or chronic rheumatoid arthritis. Even “plum pit qi” (the sensation of a foreign body in the throat, mei he qi), a condition known in TCM, is another form of phlegm (qi phlegm), triggered mainly by binding depression of liver qi due to emotional causes. Its symptoms can include difficulty swallowing, globus hystericus (“lump in the throat”), or a feeling of oppression in the chest and diaphragm.
Symptoms
General phlegm disorders
 Protracted illnesses that do not improve despite intensive treatment.
Protracted illnesses that do not improve despite intensive treatment.
 Painless lumps beneath the skin that are neither hot nor red and are freely movable (lipoma).
Painless lumps beneath the skin that are neither hot nor red and are freely movable (lipoma).
 A general feeling of heaviness and numbness, sluggishness, chronic fatigue, difficulty concentrating, especially dull headache and recurrent dizziness (Ménière disease).
A general feeling of heaviness and numbness, sluggishness, chronic fatigue, difficulty concentrating, especially dull headache and recurrent dizziness (Ménière disease).
 Frequent infections in children, with stuffy nose, muciferous and purulent bronchitis, and purulent maxillary sinus and frontal sinus infections.
Frequent infections in children, with stuffy nose, muciferous and purulent bronchitis, and purulent maxillary sinus and frontal sinus infections.
 Obesity.
Obesity.
Tip: These symptoms can be increasingly found in children and young adults due to bad dietary habits (fast food, too many sweets, dairy products, and sugary soda pops).
Differentiation of phlegm disorders by location of phlegm collection and symptoms
 Upper burner: Fatigue, lack of concentration, dull pressure in head, dizziness, ringing in the ears (tinnitus), sinusitis frontalis and sinusitis maxillaris, stuffy nose.
Upper burner: Fatigue, lack of concentration, dull pressure in head, dizziness, ringing in the ears (tinnitus), sinusitis frontalis and sinusitis maxillaris, stuffy nose.
 Center burner: Bronchitis, pneumonia, bronciectasis (inflammation of the lungs), cough with copious white or yellow secretion, nausea.
Center burner: Bronchitis, pneumonia, bronciectasis (inflammation of the lungs), cough with copious white or yellow secretion, nausea.
 Lower burner: Fluid deposits in the form of leg or ankle edemas.
Lower burner: Fluid deposits in the form of leg or ankle edemas.
Differentiation by type of phlegm condition and symptoms
 Wind and phlegm: Feeling of dizziness, sensation of numbness in the extremities, aphasia (communication disorder), wind stroke.
Wind and phlegm: Feeling of dizziness, sensation of numbness in the extremities, aphasia (communication disorder), wind stroke.
 Heat phlegm: Yellow, viscous sputum, dry mouth and lips, bronchitis, pneumonia, apathy, nebulous, confused mind, types of schizophrenia, hallucinations, manic depression.
Heat phlegm: Yellow, viscous sputum, dry mouth and lips, bronchitis, pneumonia, apathy, nebulous, confused mind, types of schizophrenia, hallucinations, manic depression.
 Cold phlegm: White, viscous sputum; lack of appetite, feeling of oppression in chest and epigastrium (abdominal wall above umbilicus [belly button]), infection of lungs.
Cold phlegm: White, viscous sputum; lack of appetite, feeling of oppression in chest and epigastrium (abdominal wall above umbilicus [belly button]), infection of lungs.
 Immaterial phlegm: Congestion of the channels, for example wind colic (apoplexy) and sensation of numbness, mostly in elderly people.
Immaterial phlegm: Congestion of the channels, for example wind colic (apoplexy) and sensation of numbness, mostly in elderly people.
Tongue: | Puffy, wet tongue is typical, partly with impression (spleen qi or spleen yang vacuity). Often oily, soft fur appears on a normal, but pale tongue in the retrolingual region. White fur: cold phlegm; yellow fur: heat phlegm. |
Pulse: | Typical slippery pulse, similar to pulse of a pregnant woman. |
Therapy
Strengthen spleen
Transform dampness and phlegm
Strengthen lung and kidneys
For chronic disorders
 Nutritional Therapy
Nutritional Therapy
 Avoid:
Avoid:
Foods that produce copious phlegm, especially dairy products, bananas, very oily and fatty foods, junk foods, too much of the sweet flavors, sugary beverages. An excess of yin foods (take into account season and climate!): raw foods, salads, and cool/cold types of fruit, citrus fruits, and juices. Frozen foods and cooking or heating meals in the microwave should also be avoided.
Caution: Meat and alcohol produce phlegm if consumed excessively. This applies especially to pork and wheat beer.
 Recommended: Strengthen spleen
Recommended: Strengthen spleen
 All foods that strengthen the spleen to deter further production of dampness and phlegm (see “Spleen/Pancreas Qi Vacuity,” p. 69 and “Spleen/Pancreas Yang Vacuity,” p. 69).
All foods that strengthen the spleen to deter further production of dampness and phlegm (see “Spleen/Pancreas Qi Vacuity,” p. 69 and “Spleen/Pancreas Yang Vacuity,” p. 69).
 Millet, rice, and corn are especially beneficial for supplementing and warming the spleen.
Millet, rice, and corn are especially beneficial for supplementing and warming the spleen.
 Soy beans and mung beans are recommended for removing excess moisture from the body.
Soy beans and mung beans are recommended for removing excess moisture from the body.
Flavors and foods that transform dampness and phlegm:
 Heat phlegm (yellow, viscous):
Heat phlegm (yellow, viscous):
 Thermal nature/flavor: bitter–cool, salty–cool, sometimes sweet–cool
Thermal nature/flavor: bitter–cool, salty–cool, sometimes sweet–cool
 Belgian endive hearts, dandelion, soy milk, mung beans, radish, pears, grapes, carp, salt, red marine algae (rhodophyta, also known as dulse), and seaweed.
Belgian endive hearts, dandelion, soy milk, mung beans, radish, pears, grapes, carp, salt, red marine algae (rhodophyta, also known as dulse), and seaweed.
 Cold phlegm (whitish, clear, thin):
Cold phlegm (whitish, clear, thin):
Thermal nature/flavor: bitter–warm, acrid–warm
In moderation, fresh ginger, leeks, garlic, cardamom, cherries.
 Phlegm obstructs qi flow in the meridians:
Phlegm obstructs qi flow in the meridians:
 Moderately acrid flavor can remove the congestions, for example strong spices such as pepper, garlic, ginger.
Moderately acrid flavor can remove the congestions, for example strong spices such as pepper, garlic, ginger.
Tip: With recurrent phlegm conditions, drastically reduce meat, alcohol, dairy products, sweets, and fatty foods. Abstain from these altogether for three to six weeks.
General recommendation for dampness and phlegm: Millet muesli or millet porridge with cinnamon and raisins.
For heat phlegm: Mung beans, mung bean decoction, soy milk, mixed juice of pears and lemons.
For cold phlegm: Ginger tea.
B Application of Chinese Dietetics for Specific Conditions
Network:
• Spleen/Pancreas–Stomach
• Earth Phase
Bowel (Zang Organ): Spleen/Pancreas (Pi), SP
Character
“In charge of economy and nutrition”
The spleen is the material foundation of the body and root of acquired qi. It is responsible for absorption, distribution, transformation, and creation of energy from food.
Role in TCM:
 Governs transformation, transport, and processing of food and energy.
Governs transformation, transport, and processing of food and energy.
 Retains the blood in the blood vessels.
Retains the blood in the blood vessels.
 Governs muscles and extremities.
Governs muscles and extremities.
 Opens at mouth and lips.
Opens at mouth and lips.
 Governs upbearing qi, keeps the organs in place.
Governs upbearing qi, keeps the organs in place.
 Houses the mind (zhi).
Houses the mind (zhi).
Association with the five phases:
 Emotions: Brooding, worries, pensiveness
Emotions: Brooding, worries, pensiveness
 Climate factor: Dampness
Climate factor: Dampness
 Season: Late summer, early fall
Season: Late summer, early fall
 Direction: Center
Direction: Center
 Color: Yellow
Color: Yellow
 Flavor: Sweet
Flavor: Sweet
 Time of day: 9–11 a.m.
Time of day: 9–11 a.m.
Viscera (Fu Organ): Stomach (Wei) ST
Function
“Cooking vessel” for acquired qi
 Most important viscera (Fu organ): Downbears the flow of qi
Most important viscera (Fu organ): Downbears the flow of qi
 Gathers food
Gathers food
 Separates and extracts food
Separates and extracts food
 Downbears
Downbears
 Loves dampness
Loves dampness
 Time of day: 7–9 a.m.
Time of day: 7–9 a.m.
Tasks and Functions of Spleen/Pancreas and Stomach
The stomach and spleen/pancreas are important bowels and viscera (zang fu organs). As the production site of acquired qi, yang, blood (xue), and body fluids (jin ye), they play a key role in TCM therapy. The famous Chinese scholar Li Gao, during the Song dynasty (AD 920–1280), emphasized the importance of the center burner by founding a special school for the “Strengthening of the Center,” which focused primarily on the treatment of the center burner.
The following quote from the Ming Dynasty (AD 1368–1644) also speaks to the significance of the body’s “center”:
Many doctors during that period were of the opinion that no disorder is really curable as long as the network of the center burner is impaired. They perfected strengthening the “inner center” by strengthening the stomach and spleen as a prerequisite for all therapy.
“Zang Fu Governs Transformation and Transport” The bowels and viscera (zang fu organs) spleen/pancreas are largely responsible for transformation and transport of ingested food. Both organs separate food into clear and turbid components. The clear components of food essence are transformed into gu qi (drum qi). Gu qi forms the basis for all acquired qi and for production of blood. According to TCM, most of the qi in our body that can be regenerated is derived from gu qi acquired through stomach and spleen/pancreas. Lack of spleen qi results in energy deficiencies for the entire body.
Key symptoms of spleen qi vacuity:
Chronic fatigue, general immune deficiency, susceptibility to infections, lack of concentration; sloppy, shapeless stool.
Therapy
Therapy principle:
Supplementing qi means also supplementing the spleen. Strengthening blood means also supplementing the spleen.
Governance of Body Fluids and Liquids
Transformation and distribution of fluids requires sufficient spleen qi. Spleen vacuity obstructs the transport of fluids. This can cause accumulation of dampness or phlegm, which can damage a weakened spleen even further. The spleen loves dryness and shuns dampness. Dampness in the body can be caused by external wetness and dampness (damp apartment, rainy fall days), but also by dampness formed on the inside of the body caused by the wrong foods (too many yin foods). Key factors that can weaken the spleen and cause dampness and later formation of phlegm, are excessive consumption of cold beverages, raw foods, salads, fruit and dairy products. Dampness, phlegm, or edemas in the body always requires treating the spleen as part of the therapy.
Symptoms
Edemas, swollen face, sensation of heaviness in the limbs; heavy, dull head; apathy, depression and lack of drive, obesity, sinus congestion (maxillary and frontal sinuses), bronchial congestion, frequent colds (see also “Dampness and Phlegm Conditions,” p. 64)
Signs of healthy spleen qi include well-shaped red lips, a closed mouth, and a good sense of taste. Spleen qi vacuity presents as pale and chapped lips and a continually open mouth. A strong preference for sweet flavors also indicates spleen disharmony.
Production and Retention of Blood
Healthy spleen qi produces sufficient blood and enables it to circulate through the body and stay in its vessels. Spleen qi vacuity can cause more frequent bleeding, because the blood can not be retained in its vessels. Gu qi (drum qi) is extracted from food and then transported by the spleen to the heart. Blood is produced in the heart with help from the original qi of the kidneys. This makes the spleen one of the central organs for the formation of qi and blood. Chronic spleen qi vacuity reduces the production of blood and results in liver blood vacuity.
Symptoms
Night blindness; blurry, distorted vision; light-sensitive eyes; numb limbs; insomnia (shen is anchored in the blood), menstrual disorders, frequent bruises (purpura, petechia, hematuria, excessive menstruation).
Governance of Muscles and Limbs
Gu qi extracted by the spleen from food is distributed to all tissues of the body. This nourishes and warms muscles and limbs and supports mobility. Weak, tired, or atrophied muscles indicate spleen qi vacuity.
Governance of Connective Tissue
The spleen holds the organs in place. Taught and elastic connective tissue is a sign of good spleen qi. Loose connective tissue, cellulite, colon/rectal pro-lapse (tuo gang), or uterus prolapse (zi gong xia chui) indicate weak spleen qi.
Home of the Mind/Thought (Si)
Clear thinking and good concentration indicate strong spleen qi. Spleen vacuity can present as mental symptoms such as fuzzy thinking, problems concentrating, and weak memory
Tip: Mental overexertion can weaken the spleen, which explains a craving for sweets during long periods of intensive studying or other mental work. The sweet flavor is associated with the earth phase and, therefore, with the spleen. Sweet flavor has the strongest supplementing effect of all flavors. In moderation, eating sweet foods during times of intense mental activity (studying, writing) can be beneficial.
| Honey, dates, poppy seed cake or muffins, raisins. |
Special Diet for Spleen/Pancreas–Stomach Network
This network is one of the most important sources of acquired qi and responds very well to dietary supplementation and treatment. The mainstay of every meal should be the sweet flavor of the earth phase. All other flavors should only be used as supplements (see also “Strengthening the Inner Center,” p. 42).
 Sweet foods such as grains, poultry, vegetables, certain types of fruit and dried fruit strengthen qi and moisten body fluids; they strengthen and supplement our “center.”
Sweet foods such as grains, poultry, vegetables, certain types of fruit and dried fruit strengthen qi and moisten body fluids; they strengthen and supplement our “center.”
 Excessive consumption of cold beverages, raw foods, fruit, and dairy products weaken the spleen.
Excessive consumption of cold beverages, raw foods, fruit, and dairy products weaken the spleen.
 Spleen qi vacuity caused by extended periods of mental activity and mental strain should be compensated with appropriate foods of the sweet flavor.
Spleen qi vacuity caused by extended periods of mental activity and mental strain should be compensated with appropriate foods of the sweet flavor.
 Caution: Excessive consumption of refined sugar and denatured sweeteners (so-called simple sugars) causes extreme fluctuations of blood glucose levels and depletes nutrients from the body. Concentrated “healthy” sweeteners such as honey, maple syrup, molasses, or raw cane sugar are also extreme representatives of the sweet flavor and should be consumed in moderation.
Caution: Excessive consumption of refined sugar and denatured sweeteners (so-called simple sugars) causes extreme fluctuations of blood glucose levels and depletes nutrients from the body. Concentrated “healthy” sweeteners such as honey, maple syrup, molasses, or raw cane sugar are also extreme representatives of the sweet flavor and should be consumed in moderation.
 Spleen vacuity causes dampness and phlegm. If present, dietary measures to treat the spleen should be included in treatment.
Spleen vacuity causes dampness and phlegm. If present, dietary measures to treat the spleen should be included in treatment.
Spleen Syndromes and Chinese Nutrition
Spleen qi vacuity (pi qi xu)
Spleen yang vacuity (pi yang xu)
Spleen Qi Vacuity (Pi Qi Xu)
This is probably one of the most common syndromes found in clinical practice and leads patients into the doctor’s office with a variety of different symptoms.
Western diagnosis:
Gastroenteritis, indigestion, malabsorption syndrome, diarrhea, anemia, and inflammatory intestinal disorders.
Symptoms
Chronic fatigue, general exhaustion, susceptibility to infection, lack of appetite, weakness and frailty of limbs, craving sweets; pale, pallid complexion; soft, sloppy stools; sometimes diarrhea.
Spleen Yang Vacuity (Pi Yang Xu)
Spleen yang vacuity can result from protracted spleen qi vacuity or pronounced weakening of the spleen due to cold foods, irregular meal times, and irregular eating habits.
 Treating acute and chronic conditions. This includes disorders of the respiratory system, allergies, acute and chronic gastrointestinal disorders, skin disorders, gynecological disorders, menopausal symptoms, urological disorders, insomnia, psychological instabilities, exhaustion, weight gain, hyperactivity.
Treating acute and chronic conditions. This includes disorders of the respiratory system, allergies, acute and chronic gastrointestinal disorders, skin disorders, gynecological disorders, menopausal symptoms, urological disorders, insomnia, psychological instabilities, exhaustion, weight gain, hyperactivity.
 Recommended:
Recommended: