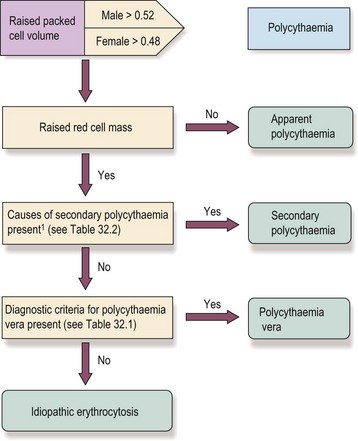
32 In simple terms, polycythaemia (or erythrocytosis) means an increase in red cell count, haemoglobin and packed cell volume (PCV) above the normally accepted levels. Polycythaemia due to an absolute increase in red cell mass may occur as a myeloproliferative neoplasm (polycythaemia vera (PV) ) or secondary to hypoxia or an abnormal focus of erythropoietin secretion. In ‘apparent polycythaemia’ the raised haemoglobin and PCV are not accompanied by a significantly raised red cell mass; usually the plasma volume is relatively reduced (Fig 32.1). Fig 32.1 Red cell mass and plasma volume in normality, true polycythaemia and apparent polycythaemia. The initial decision to investigate further is taken on the basis of a persisting raised PCV (haematocrit) or haemoglobin level. If true polycythaemia is confirmed by measurement of red cell mass and plasma volume then the next step is to determine whether this is primary or secondary. The full sequence of investigations is not required in all cases. For example, in a patient with known respiratory disease causing chronic hypoxia, a degree of polycythaemia is predictable and does not require investigation (Fig 32.2). Clinical features. The raised red cell mass and total blood volume with associated hyperviscosity causes the symptoms and signs of the disease. Common complaints include headaches, dizziness, lethargy, sweating and pruritus (the latter particularly after a hot bath). Most importantly, there is an increased risk of arterial and venous thrombosis, particularly strokes. Paradoxically, a combination of hyperviscosity and platelet dysfunction may cause a bleeding tendency. The increased cell turnover can lead to gout (Fig 32.3). Patients are characteristically plethoric and may have rosacea (Fig 32.4). Palpable splenomegaly may be present.
Polycythaemia
Introduction
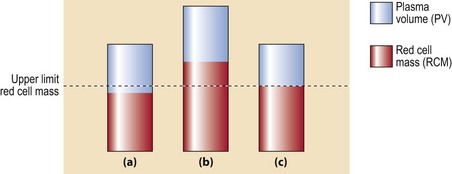
(a) Normal red cell mass (RCM) and plasma volume (PV). (b) True polycythaemia: there is a significant increase in RCM and total blood volume. (c) Apparent polycythaemia: RCM and PV are at the upper and lower limits of the normal range with a resultant increased haematocrit.
An approach to the patient with polycythaemia
Clinical syndromes
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Polycythaemia