Type of lesion
Single lesion (e.g., a small tumor)
Localized lesion (e.g.. metameric lesion)
Generalized lesions (e.g., multiple skin metastasis)
Pictures required
Close-up
✓
✓
✓
Medium view
✓
✓
✓ (not essential)
Distant view
x
✓ (helps to determine symmetry/asymmetry)
✓
Since visual clues are fundamental for diagnosis, pictures should be able to show such clues as well. Distribution, configuration, and close-up look are important elements to evaluate when looking at a skin ailment [3].
Distribution
It is important to show the location of the lesion(s) in an anatomical area. Lesions can be generalized (i.e., generalized herpes zoster in an immunosuppressed cancer patient) [4], segmental, sun- exposed area, etc.
Pictures should include some noninvolved area; for unilateral lesions, a far view involving the contralateral side should be taken to give information on symmetry (i.e., the lineal distribution of a metastasis in one arm should be capturing the contralateral arm, for comparison).
For multiple small lesions (like nevi or multiple carcinomas), it is convenient to capture a far view of the area, taking care to previously mark them with a number or a circle (Fig. 19.1).


Fig. 19.1
Patient with 2 basal cell carcinomas in the face. Eyes are covered for convention (a). The lesions are identified in the clinical picture in order to associate its relative dermoscopic (DMS) image (b,c)
For these far views, no macro is needed and the user of a backdrop is fundamental to avoid distractions.
The perception of depth that perspective gives is an important attribute. For 35 mm film, a lens of around 100 mm focal length allows distortion-free images in most clinical situations, but a shorter focal length of around 50–60 mm will be needed for full-length photographs or when working in a confined space [5].
Configuration
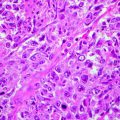
It refers to the arrangement of the lesions with respect to one another. In oncology, for example, metastasis can have linear, zosteriform (Fig. 19.2), or perilesional distribution and paraneoplastic manifestations can mimic inflammatory diseases [6].


Fig. 19.2
Zosteriform distribution of metastatic prostate cancer
Medium-distance views are required usually with macro. The presence of a backdrop is usually required. Always try to capture distinctive elements like typical representative lesions, particular configuration, or distribution patterns. (Always include a recognizable body landmark so that the location is obvious. For example, for lesions on the abdomen, include the umbilicus in the medium-distance shot.)
Primary lesion is a close-up view that requires macro. In this case, the use of backdrop is unnecessary. It requires though a perfect balance of the flash, in order to avoid shadows and bright spots in the center. Pictures are usually taken perpendicularly to the skin. Oblique views might be required to show the trimensional aspects of a tumor. For lesions with a crust, it is better to take the picture with and without, to put in evidence, the hidden elements (Fig. 19.3). The presence of a ruler leaves evidence of the size.
Fig. 19.3
Lesion with crust (a). The dermoscopic image with the crust gives little information (b). Once the crust is taken out (c), abnormal vessels suggest a squamous cell carcinoma, later confirmed by excisional biopsy
Use macro feature at distances within the 30–60 cm range.
For dermoscopy registry, two views should be taken: a far view (leaving under focus the ruler incorporated in the dermoscope) and close-up. If the clinician wants to take both polarized and immersion fluid dermoscopy, it is best to take the polarized first (with no immersion fluid) and later the second (to avoid the need to remove the fluid in between pictures).
For single lesions, take a medium view to identify location (Fig. 19.4). New photographic softwares include body location features that allow framing images by location thus making this medium view unnecessary. It would be advisable to take close-up shots from more than one angle and also to include oblique shots. Shots with and without flash may be taken and the best shot selected for filing.
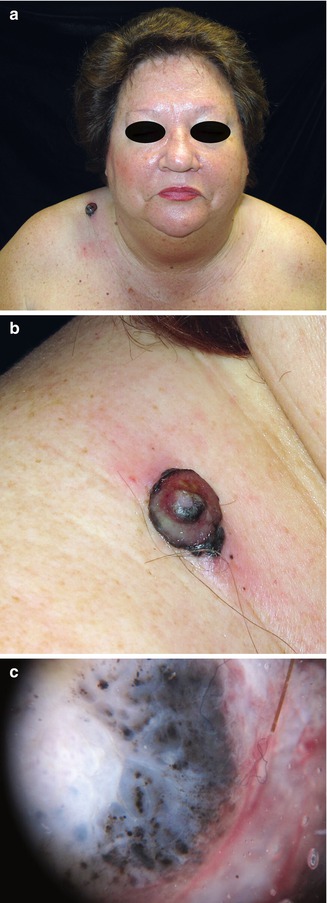
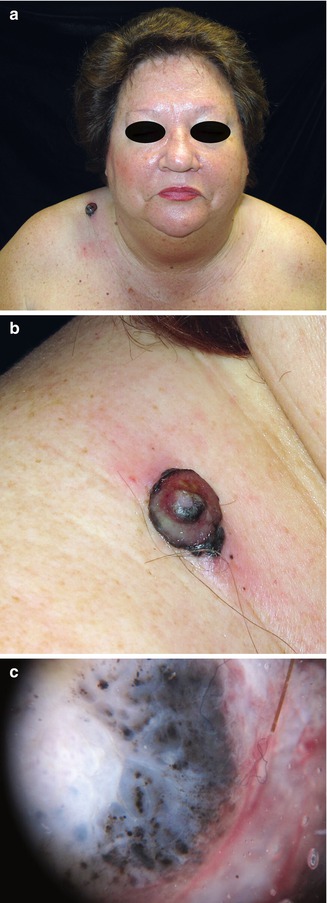
Fig. 19.4
(a) Far, (b) medium, and (c) dermoscopy view of a lesion in the right shoulder of a 61-year-old woman with a malignant melanoma
Consistency
Take pictures following the same frame of reference. This will allow you to have comparable pictures even when they are taken in different time periods. There are photographic equipments (Canfield, Microcaya) useful for face photography that allow to take before and after pictures that can be later superimposed with digital softwares. This is a feature that can be useful to measure the extent of improvement of photodamaged areas.
Have the patient close his/her eyes when taking a face picture in order to have eyes always shut (Fig. 19.5). Try to keep the same distance from the patient, same background and same anatomical position. If you get into the routinary and systematic way of working, pictures will be comparable in follow-ups.