Fig. 25.1
Actinic keratosis of the face before (a) and after (b) MAL-PDT
Fig. 25.2
Bowen’s disease of the forearm before (a) and after (b) MAL-PDT
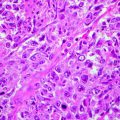
Fig. 25.3
Basal cell carcinoma of the zygomatic area before (a) and after (b) MAL-PDT
Crusts and scales, if any, should be removed with keratolytic agents or a superficial curettage before applying the cream [8].
During light exposure, patients may experience a burning sensation or stinging pain. Cooling of the lesions with a fan or spraying iced water during and soon after the treatment is widely used for reducing pain, but, if an extended irradiation field or severely photodamaged skin has to be treated, the administration of oral analgesics is also necessary [9]. The application of local analgesics like eutectic mixtures of lidocaine/prilocaine prior to irradiation overlapping the incubation period of MAL is not recommended as their high pH might chemically inactivate the photosensitiser [10].
In addition, various inexpensive ALA preparations are on the market and commonly used. However, ALA is included in the European list of orphan drugs to be used only in the photodiagnosis of bladder cancer. Therefore, their use must be authorised by the local Ethical Committee. Other main limitations are that the treatment protocol is not standardised and treatment results are not comparable. A 20 % ALA emulsion (Levulan® Kerastick, Dusa Pharmaceuticals, INC., Wilmington, MA) is registered for the treatment of AKs in the USA but is not yet available in the EU countries.
Therapeutic Applications
Actinic Keratosis (AKs)
A European multicentre randomised prospective study compared MAL-PDT and cryosurgery for AK. A total of 193 patients with 699 lesions received either a single treatment with MAL-PDT (repeated after 1 week in 8 % of cases) or a double freeze-thaw course of liquid nitrogen cryosurgery. The overall complete response (CR) rates after 3 months were not significantly different: 69 % with MAL-PDT and 75 % with cryosurgery. However, the cosmetic outcomes were deemed excellent (no scarring or hypopigmentation) in 96 % of patients treated with MAL-PDT and in 81 % of those treated with cryosurgery, and the difference was statistically significant [7].
A higher overall complete response rate after 3 months was observed with MAL-PDT (91 %) in 204 Australian patients who received another treatment session after 1 week (Table 25.1). CRs with a single treatment session of cryosurgery (68 %) and placebo (30 %) were significantly lower. Cosmetic outcome was rated excellent in 81 % of MAL-PDT patients versus 51 % of patients treated with cryosurgery [11].
Table 25.1
Clinical trials using topical MAL-PDT for treatment of actinic keratoses
Study | Design | Study size | Dosage regimen | Results |
|---|---|---|---|---|
Szeimies et al. [7] | Multicentre randomised prospective study | 193 pts with 699 lesions | MAL-PDT with MAL applied 3 h before broad-spectrum red light (75 J/cm2) vs. single treatment with cryotherapy | CR after 3 months: MAL-PDT, 69 %; cryotherapy, 75 % |
CO: MAL, 96 %; cryotherapy, 81 % | ||||
Freeman et al. [11] | Randomised prospective study | 204 pts | MAL-PDT with MAL applied 3 h before broad-spectrum red light (75 J/cm2) two treatment sessions at weekly intervals vs. single treatment with cryotherapy | CR after 3 months: MAL-PDT, 91 %; cryotherapy, 68 %; placebo, 30 % |
CO: excellent in MAL-PDT, 81 %; cryotherapy, 51 % | ||||
Pariser et al. [12] | Multicentre, randomised, double-blind study | 80 pts | MAL-PDT with MAL applied 3 h before broad-spectrum red light (75 J/cm2) two treatment sessions at weekly intervals vs. placebo | CR at 3 months: MAL, 89 %; placebo,38 % Excellent or good CO >90 % |
Tarstedt et al. [13] | Randomised multicentre trial | 211 pts with 413 thin to moderately thick AKs | MAL-PDT with MAL applied 3 h before light-emitting diode system (634 nm), 37 J/cm2; one or two treatment sessions at weekly intervals | CR: 89–93 % thin AK, 70–88 % thicker AK |
Morton et al. [14] | Randomised multicentre, intraindividual (right-left) study | 119 patients with 1,501 lesions | MAL-PDT with MAL applied 3 h before light-emitting diode system (634 nm), 37 J/cm2; one treatment session vs. cryotherapy | CR after 6 months: MAL-PDT, 89.1 %; cryotherapy, 86.1 %. CO better with MAL-PDT |
Dragieva et al. [15] | Randomised double-blind trail (transplant recipients) | 17 pts with a total number of 129 mild to moderate AKs | MAL-PDT with MAL applied 3 h before broad-spectrum red light (75 J/cm2) vs. placebo | CR: 90 % MAL-PDT vs. 0 % placebo |
Similar results (89 % CR) were found in 80 American AK patients treated with two sessions of MAL-PDT in a multicentre, randomised, double-blind, placebo-controlled study. The cosmetic outcome was scored good to excellent in more than 90 % of patients [12].
In an open prospective study, 211 patients with 413 thin to moderately thick AKs were randomised to undergo either a single treatment with MAL-PDT (regimen I; n = 105) or 2 treatments at weekly intervals (regimen II; n = 106). Thirty-seven lesions (19 %) showing an incomplete response 3 months after a single treatment were retreated. All patients were followed up 3 months after the last treatment. The complete response rate for thin lesions after a single treatment was 93 %, which was similar to 89 % after repeated treatment. Response rates were lower for thicker lesions: 70 % versus 84 %, respectively. However, the overall response rate in patients randomised for the single treatment improved after the second treatment: 88 %. The conclusion of this study was that a single MAL-PDT session is effective for thin AK and repeated treatments are recommended for thicker or non-responding lesions [13].
In a randomised multicentre trial using a side-by-side design, 119 patients with 1,501 lesions were treated with MAL-PDT or cryotherapy [14]. Twenty-four weeks after treatment, no significant difference of complete remission rates (MAL-PDT, 89.1 %; cryotherapy, 86.1 %) was seen but patients had a significant better cosmetic result with PDT.
Transplant patients have an increased propensity to develop multiple AKs and an increased transformation rate into invasive squamous cell carcinoma (SCC). Seventeen transplant recipients with a total number of 129 mild to moderate AKs were enrolled in a prospective, randomised, double-blind, placebo-controlled study. Two lesional areas of a patient were randomised for MAL-PDT or placebo cream plus light exposure. MAL-PDT cleared lesional areas in 13 of 17 patients, whereas placebo did not improve treated areas [15]. In an open trial from the same group, 20 transplant recipients and 20 controls with AK or BD underwent either a single or two consecutive treatments of 20 % ALA-PDT [16] and showed similar cure rates after 4 weeks. However, the rates were significantly lower in immunosuppressed patients after 12 and 48 weeks [15, 16]. Table 25.1 summarises the results obtained in the aforementioned studies.
Basal Cell Carcinoma (BCC)
A few multicentre, randomised, prospective and controlled studies of MAL-PDT of both superficial and nodular BCC have been done in the USA, Australia and Europe (Table 25.2). In 59 patients with 350 superficial (thickness <2 mm) BCCs, the complete-clearance response rate was 89 % after 3 months and 79 % after a follow-up of 24–48 months (median, 35 months). Cosmetic outcome was reported as excellent or good in 98 % of cases [17].
Table 25.2
Clinical trials using topical MAL-PDT for treatment of basal cell carcinoma
Study | Design | Study size | Dosage regimen | Results |
|---|---|---|---|---|
Soler et al. [17] | Retrospective study | 350 superficial (thickness <2 mm) BCC | MAL-PDT with MAL applied 3 h before incoherent halogen lamp (50–200 J/cm2) | CR: 89 % after 3 months |
79 % after 24–48 months | ||||
CO excellent or good in 98 % after 24–48 months | ||||
Basset-Séguin et al. [18] | Randomised study | 60 pts with 114 lesions were treated with MAL and 58 with 105 lesions received cryotherapy (2 freeze-thaw cycles) | MAL-PDT with MAL applied 3 h before broad-spectrum red light (75 J/cm2) two treatment sessions at weekly intervals vs. single treatment with cryotherapy | CR at 5 years: MAL-PDT, 78 %; cryotherapy, 80 % |
CO excellent in MAL-PDT, 60 %; cryotherapy, 16 % | ||||
Foley [19] | Double-blind controlled study | 66 pts with nodular BCC | MAL-PDT with MAL applied 3 h before broad-spectrum red light (75 J/cm2) 2–4 treatment sessions depending on response vs. placebo | CR: 73 % MAL-PDT vs. 21 % placebo |
CO excellent or good in 98 % | ||||
Rhodes et al. [20] | Prospective, randomised, multicentre study | 97 patients, 50 with 53 lesions treated with MAL-PDT and 47 with 52 lesions treated by excision surgery | MAL-PDT with MAL applied 3 h before broad-spectrum red light (75 J/cm2) 2–4 treatment sessions depending on response | CR at 5 years: MAL-PDT, 76 %; surgery, 96 % |
CO good to excellent in: MAL-PDT, 87 %; surgery, 54 % | ||||
Szeimies et al. [21] | Multicentre, randomised, controlled, open study | 196 pts with s-BCC | MAL-PDT with MAL applied 3 h before light-emitting diode system (634 nm), 37 J/cm2; two sessions, 1 week apart, vs. surgery | CR at 3 months: MAL-PDT, 92.2 %; surgery, 99.2 % |
CR at 12 months: MAL-PDT, 90 %; surgery, 99.2 % | ||||
CO good to excellent in: PDT, 94 %; surgery, 60 % | ||||
Vinciullo et al. [22] | Prospective, multicentre, noncomparative study
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|