Peritoneal Washings
Ognjen Kosarac MD
Dina Mody MD
ENDOMETRIAL ADENOCARCINOMA FIGO TUMOR STAGE
Peritoneal washings, when collected, continue to be considered in the prognosis of endometrial carcinoma. However, controversy exists as to the connection between positive peritoneal washings and adverse impact on prognosis, with further study and follow-up needed. The 2008 International Federation of Gynecology and Obstetrics (FIGO) staging system recommends that positive peritoneal washings should be reported. However, a “positive washing” in the new 2008 FIGO staging system is no longer used to “upstage” the patient.
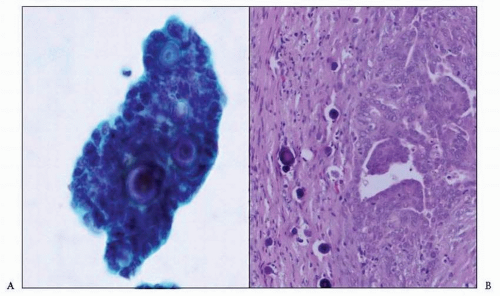
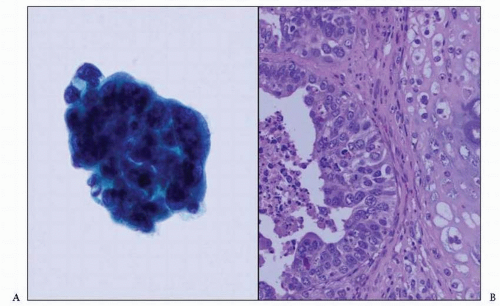
ENDOMETRIAL ADENOCARCINOMA IN PERITONEAL WASHING CYTOLOGY
Peritoneal washings are collected in saline at the time of surgery. Hence, they need to be quickly delivered to the cytology laboratory for processing before serious artifacts and degeneration of the cells set in. Artifacts and degeneration can make interpretation of an already difficult specimen nearly impossible. A negative peritoneal washing consists of a few mesothelial cells, usually in flat sheets, admixed with some blood and blood elements, which can be easily lysed prior to preparation. Peritoneal washings for the most common endometrioid type of endometrial carcinoma show single tumor cells and three-dimensional clusters. Nuclei are enlarged with course chromatin and prominent nucleoli. Cytoplasm is usually scant to moderate. Nuclear pleomorphism is marked in high-grade tumors. Yanoh et al.1 found in their study that patients with endometrial adenocarcinoma and positive peritoneal cytology were exhibiting microscopic features such as high cellularity, scalloped edges of cell clusters, and isolated cells in peritoneal fluids; thus, these microscopic features were associated with the presence of intra-abdominal macroscopic metastatic lesions. Papillary serous (Fig. 12-1) and clear cell types of endometrial adenocarcinoma are more aggressive and spread to the peritoneum more often than endometrioid type. Cytomorphologic features of these tumors are marked nuclear pleomorphism, prominent nucleoli, and abnormal mitoses. Malignant mixed müllerian tumors usually show an adenocarcinoma component only (Fig. 12-2) and rarely a sarcomatous component or a combination of both.2 The differential diagnosis of various subtypes of endometrial adenocarcinoma in peritoneal fluids includes ovarian and primary peritoneal carcinomas, but there are no reliable cytomorphologic features to distinguish among them.
SIGNIFICANCE OF POSITIVE PERITONEAL CYTOLOGY
Endometrial carcinoma malignant cells may appear in the peritoneal cavity by direct extension through the myometrium and serosa, lymphatic and vascular invasion, migration through fallopian tubes, or reflection of multifocal peritoneal occult spread.3,4 The transtubal transport seems to have the greatest attention. In several earlier studies, the presence of tumor cells within the fallopian tubes of patients with endometrial carcinoma was found.5,6 Another more recent study demonstrated that 41% of women with endometrial cancer had malignant cells in the lumen of the fallopian tubes.5
The clinical significance and management of a woman with endometrial carcinoma and positive peritoneal cytology are still controversial. Since 1981, many studies have found that positive cytology is an independent adverse prognostic factor, whereas other studies have not confirmed this finding; thus, postoperative adjuvant chemotherapy was or was not recommended, respectively (Table 12-1).7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33 and 34




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree