INTRODUCTION
SUMMARY
The classification of malignant lymphomas has been a contentious issue during the past 50 years, undergoing numerous changes during its evolution. The recent World Health Organization (WHO) classification of lymphoid neoplasms has gained worldwide acceptance by both pathologists and oncologists. It provides a list of distinct diseases that are defined by a combination of morphologic, phenotypic, genetic, and clinical features, and attempts to correlate each disease with a cell of origin. Because the classification of lymphomas requires the integration of such diverse information, the diagnosis has become more complex compared to other solid malignancies. As a result, several ancillary studies have become useful in the diagnosis of lymphomas, which require special handling of biopsy material when a diagnosis of lymphoma is suspected. The WHO classification identifies three major categories of lymphoid malignancies: B-cell neoplasms, T and natural killer (NK) cell neoplasms, and Hodgkin lymphoma. Two major categories are identified within the B-cell and T/NK-cell neoplasms: precursor neoplasms and peripheral or mature neoplasms. Unlike previous lymphoma classifications, the WHO classification does not group different lymphomas by clinical outcome or histologic grade. It recognizes that each disease has distinctive clinical features and response to treatment and may have a spectrum of clinical aggressiveness that may correlate with histologic grade or gene expression patterns. The WHO classification recognizes that several of the diseases it describes are heterogenous and likely include two or more distinct diseases that cannot be identified based on current data, and remains open to incorporate new data as they become available. One such source of new data for classifying lymphoma is the study of gene expression profiling by complementary DNA microarray technology, which is providing new insights into the classification of diseases such as diffuse large B-cell lymphoma and chronic lymphocytic leukemia. Proteomic approaches will add further texture to the molecular taxonomy of lymphoma classification.
Acronyms and Abbreviations
ABC, activated B cell; ALCL, anaplastic large cell lymphoma; ALK, anaplastic lymphoma kinase; DLBCL, diffuse large B-cell lymphoma; EBV, Epstein-Barr virus; FISH, fluorescence in situ hybridization; GCB, germinal center B cell; IGH, immunoglobulin heavy chain; LP, lymphocyte predominant; MALT, mucosa-associated lymphoid tissue; NF-κB, nuclear factor-κB; NK, natural killer; PCR, polymerase chain reaction; PTCL, peripheral T-cell lymphoma; REAL, Revised European-American Lymphoma; WHO, World Health Organization; ZAP-70, zeta-associated protein of 70 kDa.
HISTORICAL ASPECTS OF LYMPHOMA CLASSIFICATION
The classification of malignant lymphoma has been fraught with controversy during much of the 20th century, with much needed consensus reached during the past two decades. A detailed discussion of the history of lymphoma classification is beyond the scope of this chapter and can be found elsewhere.1
From Thomas Hodgkin’s description in 1832 of what became known as Hodgkin’s disease2 to the first half of the 20th century, several types of lymphomas with distinctive morphologic and clinical features were described using a variety of terms, including lymphoma, lymphosarcoma, reticulum cell sarcoma, and giant follicular lymphoma.1 However, many of the terms were not used uniformly, resulting in significant misunderstanding, particularly between pathologists and clinicians. Starting in the 1930s, several attempts were made to classify lymphomas and provide some uniformity of diagnosis, culminating in the Rappaport classification, initially published in 1956, which divided lymphomas based on growth pattern, cell type, and stage of differentiation.3,4 Most importantly, this classification demonstrated clinical relevance, showing that lymphomas with a nodular pattern had a better prognosis than diffuse lymphomas.
In the 1960s and 1970s, an explosion of studies on the immune system had a profound effect on our understanding of lymphocyte biology and had a consequent effect on our understanding of malignant lymphomas. Normal lymphocytes could now be classified into distinct lineages (B, T, and natural killer [NK]), which could be determined by expression of lineage-specific surface antigens and eventually by genetic analysis of B- and T-cell receptors.5,6 Several new lymphoma classification schemes were developed to incorporate the new immunologic data, the most important being the Kiel classification7 (used primarily in Europe) and the Lukes and Collins classification8 (used primarily in North America). By the 1970s, at least five classification schemes were widely used in different parts of the world. At the same time, clinical studies were beginning to show that some patients with aggressive lymphomas could be cured with combination chemotherapy.9 Oncologists needed to interpret results of clinical trials performed in different institutions, a situation made difficult by the use of different classification schemes that were not easily translated among themselves.
The problem was addressed by the United States National Cancer Institute, which convened a large group of investigators to determine which classification scheme was best at predicting clinical outcome of lymphoma. None of the classification schemes was identified as predicting clinical outcome better than the other schemes. Therefore, pathologists were advised to continue using one of the six classification schemes studied, and a “Working Formulation” was developed so that oncologists could translate clinical data derived in different institutions using different classification schemes.10 Lymphomas were divided into 10 categories based solely on morphologic features. To help clinicians deal with a large number of lymphoma subtypes, the lymphomas were further grouped into three clinical prognostic groups (clinical grades). Although the Working Formulation was not intended to be a standalone classification scheme, it was used as such by many institutions, particularly in North America.
However, increasing phenotypic and genotypic data were further defining several distinctive lymphoma subtypes. The Working Formulation lumped different lymphomas into broad categories that were obscuring the distinctive features of the newly described entities. The Working Formulation categories were based solely on morphologic features and were not able to incorporate new immunologic and molecular genetic data that were recognizing new types of lymphomas.
In the 1980s and 1990s, several new lymphoma entities were identified based on new immunologic and molecular genetic data. Although attempts were made to incorporate these new entities into the existing classification schemes,11 problems with uniformity between different institutions persisted. A desire to eliminate the continued confusion ultimately led to a new approach to lymphoma classification proposed by the International Lymphoma Study Group that used all available information, including morphology, immunophenotype, genetic and clinical features, to define a list of distinctive entities that could be uniformly diagnosed by hematopathologists. The proposal was published in 1994 and was known as the Revised European-American Lymphoma (REAL) classification.12 Importantly, this classification identified entities that had distinctive clinical features and could be reproducibly diagnosed by expert hematopathologists.13
WORLD HEALTH ORGANIZATION CLASSIFICATION
In the late 1990s, a new World Health Organization (WHO) classification for lymphoproliferative disorders was being developed, based on the REAL classification. First published in 2001 (and revised in 2008), the WHO classification represented a consensus between an international group of more than 50 experienced hematopathologists, including contributions from a clinical advisory committee of hematologists and oncologists experienced in treating lymphomas.14 The WHO classification (Table 96–1) identified several major categories, including precursor lymphoid neoplasms, mature B-cell neoplasms, mature T- and NK-cell neoplasms, and Hodgkin lymphoma.
|
Distinctive lymphoma entities were identified based upon a combination of morphologic, immunophenotypic, genetic, and clinical features. The 2008 WHO classification includes several provisional entities and categories of unclassifiable neoplasms with features intermediate between two distinct entities. This allows the classification to retain flexibility so that new data that further identify distinct diseases within these entities can be incorporated. In distinction from the Working Formulation, lymphomas were not classified based on clinical outcome. The WHO classification agreed that each type of lymphoma that was identified by pathologic and clinical features could have a spectrum of clinical aggressiveness, and that lumping distinct entities into groups based on clinical outcome would inhibit the development of targeted therapeutic approaches. Therefore, the WHO classification represents a complete change from the Working Formulation, with the emphasis on pathologic classification rather than classification based on survival characteristics.
Genome-wide expression studies have been instrumental in further delineating distinctive subtypes of lymphomas of clinical relevance. Using complementary DNA microarray technology, the expression of thousands of genes at the mRNA level can be studied simultaneously and compared to other tumor samples.15 Such studies have (1) defined more than one distinct entity in what was previously characterized as a morphologically homogeneous category, (2) identified distinct gene expression patterns that each encompasses a disease that may demonstrate morphologic heterogeneity, and (3) identified new surface molecules and signaling pathways that could provide targets for new therapeutic approaches. The impact of the new gene expression profiles is detailed in the sections on separate lymphomas below.
The WHO classification attempts to correlate each lymphoma to normal lymphocyte biology by postulating a cell of origin for each neoplasm. This correlation is particularly well-suited for B-cell lymphomas in which several distinct stages of normal B-cell development can be identified (Fig. 96–1) but is not as satisfying for T and NK neoplasms. Briefly, B-cell development begins in the marrow with precursor B lymphoblasts that differentiate into naïve B cells that circulate in the blood. The lymph node is the primary site where B cells encounter antigen, where naïve B cells colonize primary follicles and in mantle zones of secondary follicles (Figs. 96–2,96–3,96–4). Upon antigen stimulation, these cells undergo blast transformation and enter the germinal center reaction in the late primary immune response and the secondary immune response. In the germinal center, cells downregulate BCL2 (Fig. 96–5) and initially transform into intermediate-size cells (follicular B blasts), then into large centroblasts, and finally into small centrocytes (Figs. 96–6 and 96–7).16 Cells that survive the germinal center upregulate BCL2 and either differentiate into short-lived plasma cells through an immunoblast stage or differentiate into memory cells that populate follicular marginal zones or recirculate in the blood. Several B-cell lymphomas can be correlated with these stages of development (Fig. 96–8) and are mentioned in the sections on separate lymphomas below.
Figure 96–1.
Stages of B-cell development. Precursor B lymphoblasts in the marrow differentiate into mature B cells that circulate in blood and colonize mantle zones of lymphoid follicles. Upon antigen stimulation, the cells can differentiate directly into immunoblasts (early primary immune response) or enter the germinal center reaction (late primary and secondary immune responses). In the germinal center, cells undergo blast transformation and progress to form large centroblasts, followed by small centrocytes. These cells differentiate into either antibody-secreting plasma cells through an immunoblast stage or memory B cells that can recirculate or localize to the marginal zones of lymphoid follicles.
Figure 96–3.
Same reactive lymph node as in Fig. 96–2 but stained with an antibody to CD20 (B-cell marker), showing B cells predominantly localized to the follicles.
Figure 96–4.
Same reactive lymph node as in Fig. 96–2 but stained with an antibody to CD3 (T-cell marker), showing T cells predominantly localized to the interfollicular areas.
Figure 96–5.
Same reactive lymph node as in Fig. 96–2 but stained with an antibody to the antiapoptotic protein BCL2. Note the negative staining of the germinal centers where most of the cells will die during the maturation process.
Figure 96–8.
B-cell neoplasms correlate with different stages of development. ABC-DLBCL, activated B-cell type diffuse large B-cell lymphoma; ALL/LBL, acute lymphoblastic leukemia/lymphoblastic lymphoma; BL, Burkitt lymphoma; CLL, chronic lymphocytic leukemia; FL1, follicular lymphoma, grade 1; FL3, follicular lymphoma, grade 3; GC-DLBCL, germinal center type diffuse large B-cell lymphoma; MCL, mantle cell lymphoma; MZL, marginal zone lymphoma.
PRACTICAL CONSIDERATIONS IN THE DIAGNOSIS OF LYMPHOMA
Determining a benign from malignant lymphoid infiltrate often can be difficult because malignant lymphocytes in many lymphomas closely resemble their benign counterparts. Therefore, diagnosis commonly rests on demonstrating a combination of an abnormal architectural pattern, an abnormal immunophenotype, and evidence of lymphoid monoclonality. As a result, several ancillary special studies have become instrumental in the diagnosis and classification of lymphoma, requiring special handling of the biopsy material (Table 96–2). Whenever a diagnosis of lymphoma is considered clinically, the surgeon should perform an open biopsy of the largest involved lymph node. The lymph node should be removed intact whenever possible, because assessment of architecture is extremely important in the diagnosis and classification of lymphomas. The lymph node should be sent immediately to the pathology laboratory in the fresh state, at which time the pathologist allocates the tissue for fixation for routine histology and for special studies.
| Method | Applications | Type of Tissue Needed |
|---|---|---|
| Routine histology | Examination of routine sections will allow diagnosis of lymphoma in certain situations. In the remaining cases, the diagnosis will require the use of ancillary studies | Formalin-fixed |
| Immunohistochemistry | Immunophenotyping for lymphoma classification; can demonstrate B-cell clonality (light-chain restriction) and unique antigen expression in some cases | Formalin-fixed |
| Automated flow cytometry | Demonstration of B-cell clonality by surface immunoglobulin (Ig) light-chain restriction; immunophenotyping for lymphoma classification | Fresh tissue (single cell suspensions) |
| Polymerase chain reaction analysis | Demonstration of B- and T-cell clonality by Ig and T-cell receptor analyses; demonstration of lymphoma specific translocations (example: BCL2 gene rearrangements) | Frozen tissue Can be performed on paraffin tissue, but may not yield amplifiable DNA in some cases |
| Cytogenetics | Demonstration of clonality; Demonstration of lymphoma-specific translocations | Sterile fresh tissue |
| Fluorescent in situ hybridization | Demonstration of lymphoma-specific translocations | Fresh tissue Can be performed on paraffin tissue, but yield is variable |
Automated flow cytometry on single-cell suspensions prepared from tissue samples is extremely helpful in demonstrating B-cell clonality by surface immunoglobulin light chain restriction. It also determines the expression pattern of surface markers helpful in subclassifying lymphomas, particularly lymphomas of small B cells.17 A wide variety of antibodies that can be used on formalin-fixed tissue now are available, allowing accurate diagnosis and subclassification of lymphoma in most cases.
Molecular genetic techniques to determine B- or T-cell monoclonality or lymphoma-specific chromosomal translocations include polymerase chain reaction (PCR), Southern blot, fluorescence in situ hybridization (FISH), and cytogenetic analysis.18 PCR and FISH can be performed on formalin-fixed tissue. Results from molecular genetic testing should be interpreted in conjunction with the morphologic and immunophenotypic data, as some benign reactive lymphoid proliferations show evidence of lymphoid monoclonality.19
The diagnosis of lymphoma has become more complex than the diagnosis of other malignancies because diagnosis of lymphoma rests on correlation of morphologic features with immunophenotype and genetic data in many cases. Because of the complexity of diagnosis and the relative infrequency of lymphoma in general pathology practice, a second review by a hematopathologist with expertise in lymphoma pathology is recommended. The second review can have a significant impact on the clinical management of patients.20
Whereas open biopsy of an involved lymph node is the most useful diagnostic procedure, core-needle biopsies and fine-needle aspiration can play a role in limited situations. Core-needle biopsy might be helpful in the diagnosis of deep-seated disease in the abdomen, allowing the patient to avoid a laparotomy. However, a definitive diagnosis by core biopsy is not always possible, necessitating an open biopsy. Fine-needle aspiration is not helpful in primary diagnosis of lymphoma,21 but it may be helpful in detecting recurrence of a previously diagnosed lymphoma or in ruling out a nonhematolymphoid lesion causing lymphadenopathy. Although automated flow cytometry can be used in conjunction with cytologic examination to provide additional information for lymphoma diagnosis and classification, tissue biopsy generally is required before commencement of therapy.
PRECURSOR B- AND T-CELL LYMPHOMAS/LEUKEMIAS
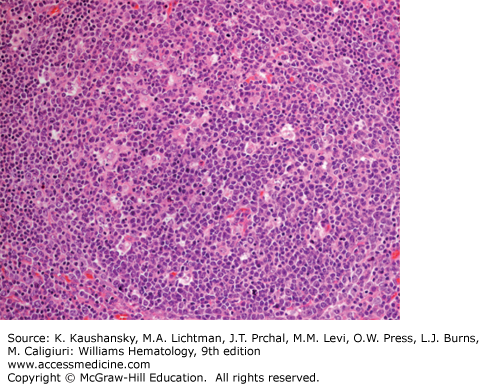
Lymphoblastic leukemia/lymphoma represents a malignancy of lymphoblasts, either of B or T lineage. They can present in the marrow (leukemia) or with predominant tissue involvement (lymphoma), but they are considered single-disease entities. Most cases of acute lymphoblastic leukemia are of B lineage, whereas most cases of lymphoblastic lymphoma are of T lineage, with the mediastinum being a common site of involvement. The morphologic features are the same regardless of site or lineage, consisting of small- to intermediate-size cells with finely dispersed nuclear chromatin, inconspicuous nucleoli, and scant cytoplasm (Fig. 96–9). Assessment of lineage and distinction from minimally differentiated acute myeloid leukemia require immunophenotypic data and may require molecular genetic analysis of B- and T-cell receptors. Lymphoblastic neoplasms are distinguished from other lymphomas by the expression of terminal deoxynucleotide transferase, which is specifically expressed at the lymphoblast stage of development.
The 2008 WHO classification includes several categories of B-lymphoblastic leukemia/lymphoma characterized by recurrent genetic abnormalities.14
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree