Miriam Baron Barshak
Pancreatic Infection
Inflammation of pancreatic tissue commonly manifests as severe acute upper abdominal pain and elevated serum levels of pancreatic enzymes. Most episodes of acute pancreatitis (AP) are associated with gallstones or alcohol abuse. Other causes of AP are hypercalcemia, hypertriglyceridemia, anatomic abnormalities, familial syndromes, autoimmune disease, ischemia, pancreatic carcinoma, trauma, endoscopic retrograde cholangiopancreatography (ERCP), and drugs (Table 78-1), among which are antimicrobial agents such as tetracycline, pentamidine, sulfonamides, didanosine, erythromycin, nitrofurantoin, and metronidazole.1 Infection of damaged pancreatic tissue may complicate disease initiated by any of these mechanisms, conferring significant morbidity and mortality risks. Less commonly, many different microorganisms may infect the pancreas directly, with or without inciting a syndrome of AP. This section reviews the infectious agents associated with primary pancreatic infection before focusing on infectious complications of AP. Issues of nonpancreatic infection related to gallstones are addressed in Chapter 77.
Infectious Causes of Acute Pancreatitis
Many organisms have been reported to cause pancreatic disease. Case reports in this area have been reviewed and assessed for adequate documentation of both pancreatitis and infection (Table 78-2).2 The reports of “definite” or “probable” association with pancreatitis described patients with coxsackieviruses, cytomegalovirus (CMV), varicella-zoster virus (VZV), herpes simplex virus 2 (HSV-2), mumps virus, hepatitis B virus, and with infections caused by Mycoplasma, Leptospira, Legionella, Salmonella enterica serotype Typhi, Aspergillus, Toxoplasma, Cryptosporidium, and Ascaris.
TABLE 78-2
Infectious Causes of Pancreatic Disease
Definite* or Probable† Pancreatitis
Ascaris
Aspergillus
Coxsackievirus B, B3, B4
Cryptosporidium
Cytomegalovirus
Hepatitis B virus
Herpes simplex virus 2
Legionella
Leptospira
Mumps virus
Mycoplasma
Salmonella Typhi
Toxoplasma
Varicella-zoster virus
Probable Pancreatic Infection‡ without Acute Pancreatitis
Actinomyces
Candida spp.
Clonorchis sinensis
Coccidioides immitis
Cryptococcus neoformans
Echinococcus granulosus
Entamoeba histolytica
Histoplasma capsulatum
Leishmania donovani
Mucormycosis
Mycobacterium avium-intracellulare
Mycobacterium tuberculosis
Nocardia asteroids
Paracoccidioides brasiliensis
Paragonimus westermani
Pneumocystis jirovecii
Schistosoma haematobium
Strongyloides stercoralis
* Pancreatitis at surgery or autopsy, or radiographic evidence.
† Threefold increase in amylase and/or lipase as well as characteristic symptoms.
‡ Culture of the organism from blood or pancreatic juice, or serologic diagnosis in a characteristic clinical or epidemiologic setting.
From Parenti DM, Steinberg W, Kang P. Infectious causes of acute pancreatitis. Pancreas. 1996;13:356-371.
Among these, ascariasis commonly causes pancreatic-biliary disease in countries with high infection rates; in some tropical areas, ascariasis ranks second to gallstones as a cause of pancreatitis.3 After hatching in the duodenum, Ascaris larvae penetrate the small bowel mucosa, enter the venous circulation, and arrive in the lungs, where they enter the alveolae, ascend the bronchial tree, and are swallowed. In the gastrointestinal tract, they mature into adult worms and then may cause clinical and pathologic AP by migrating across the ampulla of Vater to obstruct the common bile duct or the pancreatic duct.
Other organisms, including Epstein-Barr virus, vaccinia, rubella, adenovirus, and rubeola, have been cited as causes of pancreatic infection in case reports but without adequately rigorous investigation to qualify for definite or probable association with pancreatitis.2
Another group of organisms causes pancreatic infection, forming microabscesses or macroabscesses, but without inducing the signs, symptoms, or pathology of AP (see Table 78-2).2
Thus, pathologic or radiographic evidence of pancreatitis associated with well-documented infection has been noted with viruses, bacteria, fungi, and parasites. However, the frequency with which these organisms contribute to idiopathic pancreatitis is unclear.
Pancreatitis and Human Immunodeficiency Virus Infection
Although human immunodeficiency virus (HIV) itself has not been identified in pancreatic tissue by molecular methods, HIV infection has been associated with an increased risk of clinical pancreatitis. One study reports a 14% incidence of mild to moderately severe AP among patients with HIV between 1993 and 1994, with an inverse correlation between serum pancreatic enzyme level and number of CD4 lymphocytes.4 Etiologies of pancreatitis frequently seen in HIV-infected patients include drugs (e.g., pentamidine, didanosine, and trimethoprim-sulfamethoxazole) and opportunistic infections (e.g., CMV, HSV, and others listed earlier). For the most part, however, the infections (microabscesses or macroabscesses) in these reports were noted incidentally at autopsy, without prior associated symptoms or pathologic evidence of AP. In addition, advanced HIV infection is associated with an increased risk of pancreatic malignancies, including Kaposi sarcoma and lymphoma, which may lead to signs, symptoms, or laboratory abnormalities suggesting pancreatitis. Finally, isolated pancreatic enzyme elevations have been noted in HIV-infected patients lacking other signs or symptoms of pancreatitis.5 In the study discussed earlier,4 the most frequent causes of pancreatitis were gallstones, alcohol or intravenous drug abuse, pentamidine intake, and infections with Pneumocystis jirovecii and Mycobacterium avium-intracellulare complex. Of note, no pancreatic tissue sampling was performed to document the presence of these microorganisms.
Infection Complicating Acute Pancreatitis
Background
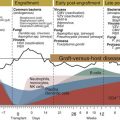
Most pancreatic infections occur as complications of AP initiated by noninfectious causes. Regardless of the inciting event, the pathogenesis of AP involves activation and release of toxic materials, including pancreatic proteolytic enzymes and vasoactive substances (trypsin, cathepsin B, phospholipase, chymotrypsin, elastase, cytokines, and the kallikrein-kinin, coagulation, and fibrinolysis cascades) that injure pancreatic cells and blood vessels. Such damage increases vascular permeability and leads to pancreatic swelling, a condition described clinically as edematous/interstitial pancreatitis. Accounting for 80% of AP cases,6 this disorder usually responds well to supportive care. In more severe disease, liberation of these toxic materials into the surrounding retroperitoneal spaces, lesser sac, and peritoneal cavity causes chemical irritation and contributes to third-space losses of protein-rich fluid, leading to hypovolemia and hypotension. In 20% of AP cases, hypoxia, free radicals, and ongoing release of pancreatic enzymes cause disruption of the pancreatic microcirculation, which leads to more severe pancreatic tissue injury and ultimately pancreatic necrosis. In addition, recruited inflammatory cells release substances such as phospholipase A2, polymorphonuclear cell elastase, interleukins, leukotrienes, and complement factors, which contribute to a systemic inflammatory response syndrome (SIRS) that may include fever, acute respiratory distress syndrome (ARDS), pleural effusions, renal failure, shock, myocardial depression, and metabolic abnormalities.7 Necrotizing pancreatitis is associated with mortality rates of 30% to 40%.8 Twenty percent of the deaths occur during the first week of illness, in the setting of this inflammatory milieu and associated multiple organ failure. Later deaths from AP often occur in association with local and systemic infectious complications.9 Predisposition to infection in severe AP may be related in part to altered immune responses; in one report, aberrant monocyte signaling profiles were identified that could alter immune defenses, including monocyte transmigration.10
Significance of Infection in Acute Pancreatitis
Some reports suggest that infection increases mortality rates. In one series of 114 patients with pancreatic necrosis, intestinal microorganisms were cultured from the necrotic tissue in 39.4% of cases. Mortality rates in patients with less than 50% gland necrosis rose from 12.9% to 38.9% if the necrotic tissue was infected, whereas mortality rates in patients with more than 50% necrosis rose from 14.3% to 66.7% in the presence of infection.11 Of note, other studies have reported that the mortality rates among patients with severe sterile necrosis are equal to those among patients with infected necrosis.12 Nonetheless, the association of mortality with infection in AP in some studies suggests that preventing, identifying, and treating infections might decrease the risks of adverse outcomes. A recent meta-analysis further supports this idea with the finding that among nearly 1500 patients with AP, the absolute influence of organ failure and infected pancreatic necrosis on mortality is comparable, and thus the presence of either indicates severe disease—that is, the relative risk (RR) of mortality doubles when organ failure and infected pancreatic necrosis are both present and indicates extremely severe disease or critical AP.13
Although infection is rare in mild pancreatitis, severe pancreatitis is associated with infection rates as high as 70%.11,14–17 This difference in infection risk has driven extensive efforts to identify patients with severe pancreatitis early in the course of illness. Multiple criteria have been suggested, with some agreement that severe AP is characterized by abnormalities in physiology (an Acute Physiology and Chronic Health Evaluation [APACHE II] score of less than 8 or equivalent for other scoring systems), in conjunction with computed tomographic (CT) evidence of less than 30% pancreatic necrosis, chest radiographic evidence of pleural effusions, and C-reactive peptide (CRP) value less than 150 mg/L.18 Of importance, the risk of infection increases with the extent of necrosis.11,19
Defining Pancreatic Infections
Pancreatic infection nomenclature, derived by consensus at the International Symposium on Acute Pancreatitis in Atlanta in 1992,20 is summarized in Table 78-3. In early AP (the first 3 weeks),12 local infection may arise in necrotic pancreatic and peripancreatic tissue without significant pus collections.21 The incidence of infection increases with the extent of necrosis and with time.22 In one study, 49% of infections in necrotizing pancreatitis developed within the first 2 weeks of illness, whereas 71% of infections developed within the first 3 weeks of illness.12 Another group reported the incidence of infection was highest among patients undergoing surgery 15 to 21 days into illness.11 The contamination rate was 24% within the first week after onset of symptoms and then rose to 36% and 71% within 2 and 3 weeks, respectively.
TABLE 78-3
Definitions Derived from the International Symposium on Acute Pancreatitis, 1992
| TERM | DEFINITION |
| Acute pancreatitis | Acute inflammatory process of the pancreas with variable involvement of other regional tissues or remote organ systems |
| Severe acute pancreatitis | Association with organ failure or local complications, or both, such as necrosis, abscess, or pseudocyst |
| Acute fluid collection | Occurs early in the course of AP, located in or near the pancreas, always lacking a wall of granulation or fibrous tissue; bacteria variably present; occurs in 30%-50% of severe AP; most acute fluid collections regress, but some progress to pseudocyst or abscess |
| Pancreatic necrosis | Diffuse or focal area(s) of nonviable pancreatic parenchyma, typically associated with peripancreatic fat necrosis, diagnosed by computed tomography scan with intravenous contrast enhancement |
| Acute pseudocyst | Collection of pancreatic juice enclosed by a wall of fibrous or granulation tissue that arises as a consequence of AP, pancreatic trauma, or chronic pancreatitis; formation requires 4 or more weeks from onset of AP |
| Pancreatic abscess | Circumscribed intraabdominal collection of pus usually in or near the pancreas, containing little or no pancreatic necrosis, arises as a consequence of AP or pancreatic trauma |
AP, acute pancreatitis.
Note: The use of terms such as phlegmon, infected pseudocyst, hemorrhagic pancreatitis, and persistent acute pancreatitis is explicitly discouraged.
From Bradley EL. A clinically based classification system for acute pancreatitis. Arch Surg. 1993;128:586-590.
Later in the course of AP (weeks 4 to 7), after the serum markers of pancreatitis resolve, pancreatic necrosis liquefies into fluid collections; sterile necrosis thus develops into pancreatic pseudocysts, whereas infected necrosis matures into pancreatic abscesses in about 3% of patients with necrotizing pancreatitis.11,15 Pseudocysts may subsequently become superinfected and develop into abscesses as well. Pancreatic abscess typically is seen with fever, abdominal pain, and leukocytosis in patients recovering from recognized pancreatic disease. In general, more systemic toxicity and mortality occur with infected necrosis than with pancreatic abscess. Specifically, mortality rates of 26% to 32.1% have been reported for infected necrosis versus 12% to 22.2% for abscess.12,21
Diagnosis of Pancreatic Infection
Identifying infection in AP can be difficult because patients with extensive necrosis of pancreatic and peripancreatic tissue frequently display a sepsis-like syndrome without a septic focus. Such patients may develop physiologic abnormalities indistinguishable from those associated with infection, including systemic organ failure syndrome involving the lungs, kidneys, liver, and cardiovascular systems. In one study,23 60% of AP patients developed fever; in 22%, the fever was related to pancreatitis per se; in 33%, it was attributed to extrapancreatic infections; and in 45%, it was due to infected pancreatic necrosis. Imaging by CT can aid in diagnosing infected pancreatic necrosis only if gas is seen in and around areas of pancreatic necrosis. Several laboratory parameters have been evaluated as markers of pancreatic infection; the most promising of these is procalcitonin, a 116 amino-acid propeptide of calcitonin, but more data from larger studies must be obtained.24,25 A recent study addressed the value of routine clinical tests (white blood cell [WBC] and CRP) in predicting the development of infected pancreatic necrosis in severe AP. The authors reported that if CRP and WBC values were below cutoff values (81 mg/L for CRP and 13 × 109/L for WBC), the risk for infected necrosis was approximately 1.4%. The authors suggest that invasive testing to diagnose infection may be unnecessary in this subset of patients.26 In most patients, however, tissue sampling must be undertaken to detect infection; Gram stain and culture of pancreatic tissue sampled by CT-guided fine-needle aspiration (FNA) provides high diagnostic sensitivity and specificity with minimal risk of introducing infection or disseminating organisms by intestinal puncture.12 This procedure is recommended for patients with necrotizing AP and persistent systemic toxicity or organ failure, or both, in the first 7 to 14 days. Similarly, culture of material retrieved by FNA of collections, seen by CT or ultrasound imaging, allows diagnosis of pancreatic abscess. Such collections may spread from the pancreas into the retroperitoneum, mesentery, mediastinum, and elsewhere, through tissue damaged by activated proteases, vasoactive substances, and inflammatory mediators.27
Microbiology of Pancreatic Infection
Pancreatic superinfection (both infected necrosis and abscess) usually involves gastrointestinal flora, including aerobes and anaerobes. Historically, both gram-negative (most commonly Escherichia coli and Klebsiella species, less commonly Enterobacter, Pseudomonas, Proteus, and others) and gram-positive (enterococcal, streptococcal, and staphylococcal species) bacteria participate, and infections may be monomicrobial or polymicrobial. In a collected series of 45 articles, representing more than 1100 cases of secondary pancreatic infections,28 the causative organisms were E. coli (35%), Klebsiella pneumoniae (24%), Enterococcus spp. (24%), Staphylococcus spp. (14%), and Pseudomonas spp. (11%).
One group29 has reported a different microbiologic picture of infected pancreatic necrosis in alcoholic and biliary pancreatitis among 70 patients with similar degrees of necrosis and who underwent surgery for pancreatitis. These authors note a higher rate of infection overall and a preponderance of gram-negative organisms in the biliary disease patients, compared with a tendency toward more gram-positive pancreatic infections in the alcoholic group. The authors hypothesize that these differences might be explained by a biliary origin of pancreatic infection among patients with biliary disease, in contrast to a hematogenous origin of infection from catheter contamination in the alcoholic population. Of note, other work has shown that mortality from pancreatitis is related to the severity of the attack and not the underlying cause.30
Earlier exposure to broadly active antimicrobial therapy changes the flora that cause infections, and increasingly resistant bacterial infections and fungal infections have become more common.31 One group reports no correlation of fungal infection with negative outcomes,32 but other studies suggest otherwise. One report33 includes prospective data on 57 patients with infected necrotizing AP from 1983 to 1995, of whom 7 patients (12%) developed either pure fungal infection or mixed fungal and bacterial infection; isolates were Candida albicans and Torulopsis glabrata, detected an average of 36 (range, 18 to 80) days after onset of pancreatitis. Among these patients, 4 of 7 had “primary” fungal infection that developed in the absence of prior operative interventions. Fungal infection was associated with ERCP as the cause of AP (P = .02) and with exposure to parenteral nutrition and broad-spectrum antibiotics. Treatment included amphotericin B in 5 patients, of whom 2 received antifungal therapy, only after developing candidemia 35 and 67 days, respectively, after diagnosis of pancreatic fungal infection; 2 additional patients did not receive antifungal therapy at all because of concerns about toxicity. There was a trend toward higher mortality rates among patients with fungal isolates compared with patients with bacterial infection. Survivors underwent twice as many necrosectomies as nonsurvivors, suggesting that aggressive surgical management of these infections is warranted. Another study reports a 41% rate of Candida infection in peripancreatic sepsis (7 of 17 consecutive patients managed between 1988 and 1992). The mortality rate was 0% for the 10 patients without fungal infection, compared with 42% among the Candida-infected patients (P = .05), without apparent relationship to microbiologic cure.34 Another group35 observed fungal infections in 17 of 46 patients (37%) with infected necrosis over an 8-year period. There was no mortality difference attributable to fungal infection. A lower rate of fungal infection without mortality benefit was noted in a subset of 18 patients who received prophylactic antifungal treatment.
Overall, the profile of organisms suggests most pancreatic infections originate in the gastrointestinal tract and seed the pancreas via the bowel, the biliary tree, the lymphatics, or the bloodstream. Initially, bowel flora may translocate across a gastrointestinal mucosal barrier damaged by ischemia during the hypovolemic phase of AP.
Management of Pancreatic Infection
In most cases, treating pancreatic infection requires antimicrobial therapy directed at organisms identified in cultures of the infected site, in combination with mechanical removal of the infected material. Although some groups36 have reported successful medical management of infected necrosis, most have traditionally believed that thorough surgical débridement of infected necrosis and removal of all associated fluid collections are necessary. The timing of surgery is a matter of some debate in the literature. The intended benefit from early intervention is prompt removal of the infected material in hopes of more rapid resolution of the inflammatory processes. However, a delay in surgery may allow for a more stable patient with better-demarcated areas of necrotic tissue. No studies have evaluated the optimal timing of surgery for infected necrosis in particular, but one randomized clinical trial studying patients with severe necrotizing pancreatitis found a trend toward higher mortality (58% vs. 27%) associated with early surgery.37 Surgical approaches (i.e., necrosectomy with continuous closed lavage, débridement with open packing, or necrosectomy and drainage with planned reoperation) have not been found to differ in efficacy.38,39 Surgical management often requires multiple staged operations to remove all necrotic pancreatic and peripancreatic material. For patients with infected necrosis or pancreatic abscess, percutaneous catheter drainage has traditionally been considered a reasonable adjunct to surgery for initial stabilization of a septic patient or for postoperative management of further abscesses. In contrast, postpancreatitis abscesses remote from the pancreas itself and superinfected pancreatic pseudocysts are unlikely to be associated with significant amounts of necrotic tissue; these may be managed successfully by catheter drainage or by surgical drainage in conjunction with appropriate antimicrobial therapy.27
Several recent studies suggest that infected pancreatic necrosis may also be managed successfully via catheter drainage, without surgical intervention. In one report, primary CT-guided percutaneous catheter drainage was successful for approximately one half of the patients with acute necrotizing pancreatitis, and the presence of multisystem organ failure was a more important indicator of outcome than the presence of infection.40 For patients in whom catheter drainage is inadequate, several newer approaches to surgical management have been described. One recent publication describes a randomized controlled trial that demonstrated reductions in proinflammatory response as well as reductions in a composite clinical end point of major complications or death for patients treated with endoscopic transgastric necrosectomy (transgastric puncture, retroperitoneal drainage, and necrosectomy) compared with surgical necrosectomy.41 Another group describes a prospective cohort study supporting the safety and efficacy of video-assisted retroperitoneal débridement (VARD) for infected pancreatic walled-off necrosis. In this study of 40 patients with pancreatic necrosis who had infection determined using Gram stain or culture, percutaneous drains were placed at enrollment, and computed tomographic scans were repeated at 10 days. Patients who had more than a 75% reduction in collection size were treated with drains. Other patients were treated with VARD. Crossover to open surgery was performed for technical reasons and/or according to surgeon judgment. Overall, 85% of patients were eligible for this minimally invasive approach, including 60% of surgical patients. Most patients (81%) required only one surgical procedure, and the mortality and complication rates compared favorably with open débridement. Of interest, a reduction in collection size of 75% according to the results of computed tomographic scans at 10 to 14 days predicted the success of percutaneous drainage alone.42
The role of surgery in the management of sterile necrosis is more controversial. Some believe that a subset of patients with severe sterile necrosis that has organized over the course of a prolonged illness (4-6 weeks or more) may benefit from surgical débridement.43 The decision to drain sterile fluid collections also is based predominantly on symptoms.
Prevention of Pancreatic Infection
Because infection may be associated with increased mortality rates in AP despite aggressive medical and surgical therapy, major efforts have been oriented toward preventing infection. Studies have focused on maintaining the gut barrier function, probiotics, selective gut decontamination (SGD) with oral, nonabsorbable antibiotics, and early therapy with systemic antibiotics. A reasonable aim for such studies is to identify interventions that decrease the frequency of pancreatic infection, leading to fewer surgical procedures and lower mortality rates.
Early Enteral Feeding
Several groups have studied enteral feeding in AP for its ability to lower infection risk both by reducing dependence on central venous access for parenteral alimentation and by sustaining the integrity of the intestinal barrier. In animal studies of AP,44 enteral nutrition was associated with less bacterial and/or endotoxin translocation into mesenteric lymph nodes but did not influence pancreatic healing or overall survival. In one study of humans, 38 patients with severe AP were randomized to parenteral nutrition or to enteral nutrition via nasojejunal tube (NJT) within the first 48 hours after admission. The NJT patients suffered fewer complications (P < .05) and fewer infectious complications (P < .01).45 Of note, all patients received imipenem from admission until clinical recovery and restoration of normal CRP concentrations. The authors speculate that enteral feeding “improves the gut immune system, restores normal gut structure and microflora, and aids the mucosa in withstanding challenges… it is, in fact, still unclear whether enteral feeding improves the rate of septic morbidity or whether total parenteral nutrition (TPN) itself causes an increase in septic complications.” Another study of 89 patients with pancreatitis observed that enteral nutrition significantly reduced septic complications but did not affect the rates of multiple organ failure or death.46
Probiotics have been evaluated in addition to enteral feeding. A randomized, double-blind study showed significantly less pancreatic sepsis and fewer surgical interventions in 22 AP patients given live Lactobacillus for 1 week, compared with 23 control patients given heat-killed Lactobacillus. Both groups received early enteral feeding with oat fiber supplementation as a substrate for the lactic acid bacteria.47 In a subsequent double-blind, placebo-controlled study, 298 patients with severe AP received a multispecies probiotic product or placebo, administered via NJT along with tube feeding. Infection rates were similar between groups, but mortality was higher in the probiotic group (16% vs. 6%; RR, 2.53). Nine patients in the probiotic group developed bowel ischemia (8 of whom died), compared with none in the placebo group (P = .004). The researchers concluded that this probiotic should not be administered to patients with predicted severe AP.48 Commentators provide several possible explanations for these unexpected results, including a potentially harmful interaction between the probiotic and the enteral feeding formula used. They also speculate that “patients with multiorgan dysfunction who need vasopressors to maintain systemic circulation might have severe splanchnic hypoperfusion. Probiotics with enteral feeding might result in intestinal oxygen consumption exceeding supply, resulting in overt ischemia.”49 In a follow-up study, bacteremia, infected necrosis, organ failure, and mortality were all associated with intestinal barrier dysfunction early in the course of AP. This was determined by measuring excretion of intestinal fatty acid binding protein (a parameter for enterocyte damage), recovery of polyethylene glycols (a parameter for intestinal permeability), and excretion of nitric oxide (a parameter for bacterial translocation) in urine samples that were collected 24 to 48 hours after randomization to probiotic or placebo treatment and 7 days thereafter from 141 patients with predicted severe AP. The specific combination of probiotic strains used in this study reduced bacterial translocation overall but was associated with increased bacterial translocation and enterocyte damage in patients with organ failure.50
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree