An English surgeon by the name of Sir James Paget reported on a condition of eczematous change of the nipple–areola complex associated with underlying breast malignancy in 1874.1 It is now recognized that Paget disease denotes an entity of intraepithelial adenocarcinoma within the epidermis of the nipple–areola complex that is associated with underlying in situ or invasive mammary carcinoma in 92% to 100% of cases.2-4 Paget cells, large cells with pale cytoplasm and prominent nucleoli, identified within nipple epidermis on histology confirm diagnosis. Ninety percent of these will overexpress Her-2/neu.
Paget disease usually presents as a scaling, erythematous, eczematous lesion of the nipple that can be mistaken as a benign condition leading to delayed diagnosis (Fig.19-1). Usually the disease is unilateral, beginning at the nipple, and may spread to the areola; however, there are instances where only the areola may be affected. Late stages may be associated with ulceration, crusting, serous or bloody nipple discharge, and nipple retraction or flattening (Fig. 19-2). Patients may complain of pain, burning, and/or itching. Physical exam may reveal an underlying breast mass in 30% to 50% of cases. Rarely, Paget disease will be identified on a mastectomy specimen without clinical signs of disease (no skin lesion).
The pathogenesis of Paget disease has been long debated, with 2 main competing theories: the epidermotrophic theory and the transformation theory. The epidermotrophic theory, currently the more favored theory, states that neoplastic ductal epithelial cells migrate through the ductal system of the breast into the epidermis of the nipple. Evidence for this lies in the observation that both the underlying mammary carcinoma and the intraepithelial nipple lesion will have similar staining of markers such as CEA, c-erb-B2, and Her-2/neu,6,7 suggesting that the nipple lesion arose from the breast malignancy. In addition, there is some research pointing to the ability of the Her2/neu receptor acting as an agent that induces chemotaxis of tumor cells, allowing for migration of malignant cells to the nipple, thus giving a mechanistic explanation supporting the epidermotrophic theory.8,9
On the other hand, the transformation theory suggests that epidermal keritinocytes within the nipple transform into malignant Paget cells, implying that Paget disease is actually an in situ carcinoma. Evidence for this lies in the fact that not all intraepithelial malignant lesions are associated with underlying mammary carcinoma. In addition, some breast cancers are located peripheral to the nipple lesion, suggesting 2 concurrent but separate processes. Electron microscopy studies of cell junctions have been able to identify tight junctions between adjacent Paget cells, suggesting that they may not have migrated from underlying breast tissue.10 Additional evidence for the transformation theory lies in the detection of a “pre-Paget” cell—half keritinocyte, half Paget, also known as a Toker cell.11 This cell could represent an intermediate or precursor to Paget, in line with the transformation theory.
The differential diagnosis for Paget disease includes a variety of other benign and malignant conditions, including atopic or contact dermatitis, erosive adenomatosis (nipple adenoma), psoriasis, hyperkeratosis of the nipple–areola, eczema, Bowen disease, basal cell carcinoma, superficial spreading malignant melanoma, and pemphigus vulgaris. Immunohistochemistry stains can differentiate these various pathologies (CEA, c-erb-B2, Her-2/neu).
The diagnosis of Paget disease is made with a full-thickness wedge biopsy of the nipple–areola complex. On histology, Paget cells can be identified within the epidermis of the nipple (Fig. 19-3). In lower epidermal layers, Paget cells can form gland-like structures. Immunohistochemical stains for CEA, keratin 7, androgen receptor, c-erb-B2, and other oncoproteins and cell cycle–related antigens may be positive and can aid in diagnosis.
Figure 19-3
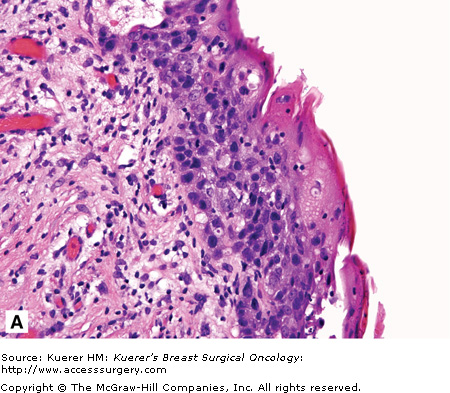
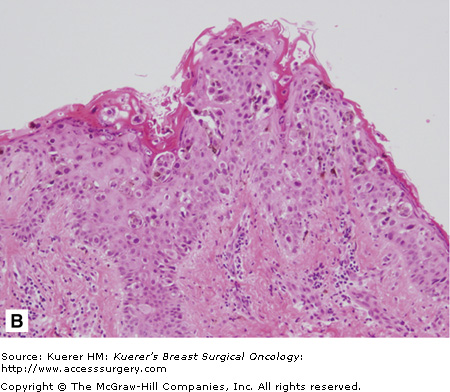
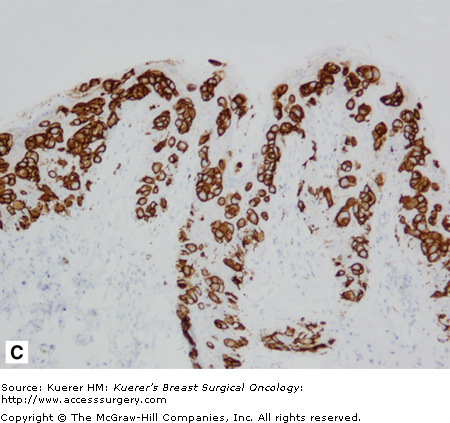
Histologic appearance of Paget disease. A. High-power view showing the surface of the nipple with neoplastic epithelial cells, which are histologically similar to the high-grade intraductal carcinoma cells present in the underlying lactiferous ducts. B. Tissue section of nipple shows presence of neoplastic epithelial cells distributed singly and in clusters (arrows). C. Some of the tumor cells contain brownish pigment derived from ingestion of melanin pigment from adjacent melanocytes. The tumor cells demonstrate strong and diffuse membranous staining for Her-2/neu, a commonly noted feature in Paget disease. (Courtesy of Dr Syed A. Hoda, Department of Pathology, New York Presbyterian Hospital—Cornell [A] and Dr Savitri Krishnamurthy, Department of Pathology, MD Anderson Cancer Center [B and C].)











